Introduction to Chorioretinitis.
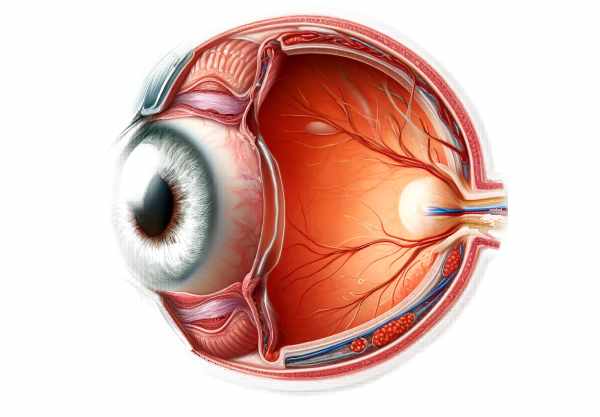
Chorioretinitis is an inflammatory disease that affects the choroid and retina of the eye. The choroid is a layer of blood vessels and connective tissue located between the sclera (white of the eye) and the retina. Its function is to provide oxygen and nutrients to the retina’s outer layers. If left untreated, inflammation in these structures can cause significant visual impairment. Chorioretinitis can be caused by a variety of infectious and non-infectious conditions, including autoimmune disorders, infections, and trauma. Common symptoms include blurred vision, eye pain, redness, and light sensitivity. Understanding chorioretinitis is critical for early detection and effective treatment to avoid long-term vision problems.
Understanding Chorioretinitis.
Etiology.
Chorioretinitis can be caused by a variety of factors, which are broadly classified as infectious or non-infectious etiology.
Infectious Causes
- Bacterial Infections: Chorioretinitis can be caused by bacteria including Mycobacterium tuberculosis, Treponema pallidum (syphilis), and Borrelia burgdorferi (Lyme disease). Ocular tuberculosis is a major cause in endemic areas.
- Viral Infections: Chorioretinitis is commonly caused by viruses such as herpes simplex virus (HSV), cytomegalovirus (CMV), and varicella-zoster virus (VZV). CMV is especially prevalent in immunocompromised patients, such as those living with HIV/AIDS.
- Fungal Infections: Fungal organisms like Candida, Aspergillus, and Histoplasma can cause chorioretinitis, particularly in immunocompromised people.
- Parasitic Infections: Toxoplasma gondii is the most common cause of chorioretinitis worldwide. Toxoplasmosis-related chorioretinitis can be congenital or acquired, and it is a major cause of posterior uveitis.
Non-infectious Causes
- Autoimmune Diseases: Sarcoidosis, Behçet’s disease, and Vogt-Koyanagi-Harada (VKH) syndrome can all result in chorioretinitis via autoimmune mechanisms.
- Systemic Inflammatory Diseases: Inflammatory bowel disease (IBD) and systemic lupus erythematosus (SLE) can cause ocular inflammation, including chorioretinitis.
- Trauma and Surgery: Traumatic eye injuries and surgical procedures can both cause chorioretinitis, either directly or indirectly.
- Drug Reactions: Some medications, including biologics and chemotherapy agents, can cause inflammatory reactions in the eyes.
Pathophysiology.
Chorioretinitis is characterized by an inflammatory response that affects the choroid and retina. Infections, autoimmune reactions, and other systemic conditions can all cause inflammation. The immune system’s response to these stimuli causes the release of cytokines and other inflammatory mediators, resulting in the characteristic symptoms of chorioretinitis.
- Inflammatory Cascade: The immune system recognizes pathogens or autoantigens, which initiates the inflammatory response. This results in the release of cytokines, chemokines, and other mediators, which attract inflammatory cells to the site of infection or injury.
- Cellular Infiltration: Immune cells, such as neutrophils, lymphocytes, and macrophages, infiltrate the choroid and retina, causing tissue damage and disrupting normal cellular architecture. This can result in the formation of granulomas in conditions such as tuberculosis or sarcoidosis.
- Vascular Changes: Inflammation can cause increased vascular permeability, resulting in fluid leakage, hemorrhage, and edema in the retina and choroidal tissues. This weakens the blood-retinal barrier, disrupting nutrient and oxygen supply to the retina.
- Fibrosis and Scarring: Chronic inflammation can cause fibrosis and scarring in the choroid and retina, resulting in permanent structural damage and vision loss.
Clinical Manifestations
Chorioretinitis causes a variety of symptoms, which can vary in severity depending on the underlying cause and the extent of inflammation. The most common clinical manifestations are:
- Visual Disturbances: Patients may have blurred vision, floaters, or scotomas (blind spots). These symptoms are frequently caused by retinal edema, hemorrhages, or exudates on the visual pathway.
- Photophobia: Light sensitivity is a common complaint caused by inflammation in the retina and choroidal tissues.
- Eye Pain: Pain can be a noticeable symptom, especially if the inflammation affects the anterior segment of the eye or there is an increase in intraocular pressure.
- Redness and Swelling: The eye may become red and swollen, especially if the inflammation spreads to the anterior segment, resulting in secondary iritis or sclerosis.
- Night Vision Issues: Damage to photoreceptor cells can impair night vision, making it difficult for patients to see in low-light situations.
Complications:
If left untreated, chorioretinitis can cause a number of serious complications, including:
- Cystoid Macular Edema (CME): Inflammation can cause fluid accumulation in the macula, resulting in CME and severe central vision loss.
- Retinal Detachment: Severe inflammation can cause retinal tears or detachment, requiring immediate surgical intervention to avoid permanent vision loss.
- Neovascularization: Chronic inflammation can promote the formation of abnormal blood vessels, which can bleed or cause additional retinal damage.
- Optic Nerve Damage: Inflammation can spread to the optic nerve, causing optic neuropathy and additional visual impairment.
- Glaucoma: Increased intraocular pressure due to inflammation or steroid treatment can cause glaucoma, which can further damage the optic nerve and impair vision.
Risk Factors
Several factors can raise the risk of developing chorioretinitis.
- Immunocompromised State: People with weakened immune systems, such as those with HIV/AIDS, undergoing chemotherapy, or taking immunosuppressive medications, are more susceptible to infectious causes of chorioretinitis.
- Autoimmune Diseases: Patients with autoimmune conditions such as SLE, rheumatoid arthritis, or sarcoidosis are more likely to develop noninfectious chorioretinitis.
- Infection Exposure: Traveling to areas where certain infections (e.g., toxoplasmosis, tuberculosis) are prevalent, as well as contact with infected animals, can increase the risk.
- Ocular Trauma: Previous eye injuries or surgeries can put people at risk for inflammatory reactions that lead to chorioretinitis.
- Genetic Predisposition: Genetic factors may influence susceptibility to autoimmune and inflammatory diseases that cause chorioretinitis.
Essential Preventive Measures
Chorioretinitis is prevented by reducing the risk of infection, managing underlying conditions, and protecting the eyes from trauma. Here are some important preventative measures:
- Regular Eye Examinations: Regular visits to an ophthalmologist can help detect early signs of inflammation or infection, allowing for prompt treatment.
- Managing Chronic Conditions: Proper treatment for chronic illnesses such as diabetes, autoimmune diseases, and HIV/AIDS can lower the risk of developing chorioretinitis.
- Vaccinations: Staying up to date on vaccinations, such as measles, rubella, and varicella, can help prevent viral infections that can lead to chorioretinitis.
- Safe Animal Handling: To reduce the risk of toxoplasmosis, avoid contact with cat feces and practice good hygiene when handling pets.
- Travel Precautions: Vaccinations and avoiding high-risk areas can reduce the risk of contracting tuberculosis or Lyme disease.
- Protective Eyewear: Wearing protective eyewear in situations where eye injuries are likely, such as certain occupations or sports, can help prevent trauma-induced chorioretinitis.
- Early Treatment of Infections: Using appropriate antibiotics or antiviral medications to treat systemic infections can help prevent them from spreading to ocular tissues.
- Avoiding Immunosuppressive Agents: To reduce the risk of inflammation, use immunosuppressive medications sparingly and closely monitor for ocular side effects.
- Healthy Lifestyle: Leading a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking can boost the immune system and lower the risk of inflammatory diseases.
- Regular Monitoring for High-Risk Patients: Patients with known risk factors should be monitored on a regular basis for signs of chorioretinitis to ensure early detection and treatment.
Diagnostic methods
Chorioretinitis is diagnosed through a comprehensive evaluation that includes clinical assessment as well as advanced imaging techniques. Early and accurate diagnosis is critical for effective treatment and avoidance of complications.
Standard Diagnostic Techniques
- Clinical Examination*:
- Visual Acuity Test: Determines the level of vision loss or impairment.
- Slit-Lamp Examination: A thorough examination of the anterior segment of the eye to detect any signs of inflammation.
- Fundus Examination: Direct or indirect ophthalmoscopy to visualize the retina and choroid, looking for signs of inflammation, hemorrhage, or scarring.
- Optical Coherence Tomography(OCT):
- OCT produces high-resolution cross-sectional images of the retina and choroid, enabling the detection of structural changes such as edema, detachment, or atrophy. This non-invasive imaging technique is critical for tracking the progression and response to treatment.
- Fluorescein Angiogram:
- This diagnostic test involves injecting a fluorescent dye into the bloodstream, which illuminates the retinal blood vessels with a specialized camera. It aids in the detection of leakage, ischemia, or neovascularization that would otherwise go undetected.
- B-Scan Ultrasoundography:
- Used when media opacities, such as vitreous hemorrhage, block the view of the retina. The B-scan produces a detailed image of the posterior segment, which aids in the identification of retinal detachments, choroidal thickening, and other intraocular abnormalities.
Innovative Diagnostic Techniques
- Indocyanine Green Angiogram (ICGA):
- Similar to fluorescein angiography, but with indocyanine green dye for better imaging of the choroidal circulation. It is particularly effective for detecting choroidal neovascularization and other deep tissue abnormalities.
- Fundus Autofluorescence(FAF):
- FAF imaging detects the RPE’s natural fluorescence. This technique aids in identifying areas of RPE damage or metabolic stress, which are critical in chronic inflammatory conditions.
- ** Electroretinography (ERG)**:
- ERG detects the electrical responses of different cell types in the retina to light stimuli. It provides functional information about the retina’s health, which is useful in determining the degree of retinal involvement in chorioretinitis.
- Multimodal Imaging*:
- Combining different imaging modalities (OCT, FAF, and ICGA) provides a comprehensive view of the retinal and choroidal structures, allowing for more accurate diagnosis and treatment response monitoring.
- Genetic and Molecular Tests:
- When a genetic or autoimmune component is suspected, genetic testing and molecular diagnostics can aid in the identification of underlying causes and the development of personalized treatment strategies.
Treatment.
Chorioretinitis is treated by addressing the underlying cause, controlling inflammation, and preventing complications. Medication, surgical interventions, and emerging therapies are all potential treatment options.
Standard Treatments
- Medications:
- Corticosteroids: Systemic or local corticosteroids (oral, topical, or periocular injections) are frequently used to reduce inflammation. They are effective at managing acute episodes and preventing recurrent inflammation.
- Antibiotics and antivirals: Used when an infectious cause has been identified. Antibiotics, for example, are used to treat bacterial infections such as syphilis and tuberculosis, while antivirals are used to treat viral infections like CMV and HSV.
- Immunosuppressive Agents: In cases of autoimmune or chronic inflammatory chorioretinitis, immunosuppressive drugs such as methotrexate, cyclosporine, or biologics (e.g., infliximab) may be used to control inflammation.
- Surgical Intervention:
- Vitrectomy: This surgical procedure involves removing the vitreous humor, particularly in cases of significant vitreous hemorrhage or retinal detachment. It helps to clear the visual axis, allowing for more effective retinal treatment.
- Laser Photocoagulation is used to treat retinal tears, detachments, and neovascularization. It helps to seal the retina to the underlying tissue, preventing further damage.
Innovative and Emerging Therapies
- Anti-VEGF Treatment:
- VEGF inhibitors, such as ranibizumab and bevacizumab, are injected into the eye to reduce neovascularization and macular edema. These treatments are especially effective for those who have secondary neovascular complications.
- Genetic Therapy:
- Gene therapy research aims to correct genetic defects or modulate immune responses in diseases such as chorioretinitis. While still experimental, these treatments hold promise for long-term disease control and vision preservation.
- Stem Cell Treatment:
- Stem cell therapy involves transplanting stem cells into the retina in order to regenerate damaged tissues. This novel approach is being investigated for its ability to restore vision in severe cases of chorioretinitis.
- Retinal Prosthetics:
- For patients with severe vision loss, retinal implants or “bionic eyes” can restore some visual function by electrically stimulating the remaining retinal cells. These devices are still in the experimental stage, but they provide hope for vision restoration.
- Biologics:
- Monoclonal antibodies and other biologic agents that target specific inflammatory pathways are being studied for their potential to control chronic inflammation without the side effects of traditional immunosuppressive drugs.
Trusted Resources
Books.
- “Ocular Inflammatory Disease” by Scott M. Whitcup & James T. Rosenbaum
- “Retina” by Stephen J. Ryan.
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup.










