Introduction to Choroidal Neovascularization.
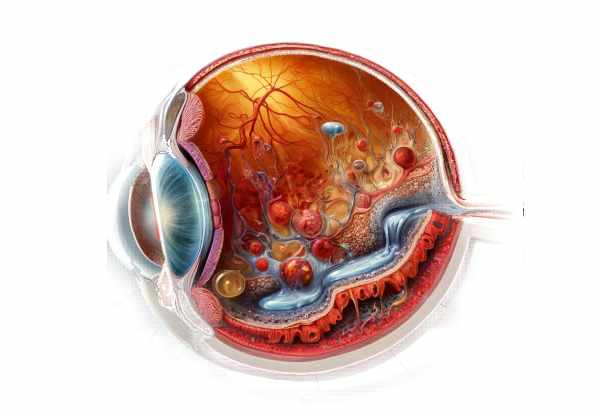
Choroidal neovascularization (CNV) is a serious ocular condition characterized by the abnormal growth of new blood vessels from the choroid, the eye’s vascular layer, into the surrounding retina. If not treated, this abnormal vascular proliferation can cause severe visual impairment or even blindness. CNV is commonly associated with a variety of retinal diseases, particularly age-related macular degeneration (AMD), but it can also be caused by other conditions such as high myopia, ocular trauma, or inflammation. Understanding the pathophysiology, risk factors, and clinical manifestations of CNV is critical for early detection and effective treatment, preserving vision and improving patient outcomes.
Choroidal Neovascularization Insights
Choroidal neovascularization is the development of new blood vessels from the choroid through the Bruch’s membrane and into the subretinal or sub-RPE (retinal pigment epithelium) space. These newly formed vessels are typically fragile and prone to leakage, resulting in the accumulation of fluid, lipids, and blood beneath the retina, disrupting its architecture and functionality.
Pathophysiology
CNV is caused by a variety of factors, including hypoxia, oxidative stress, and inflammatory processes. The underlying mechanism frequently involves the activation of angiogenic factors like vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF). These factors stimulate the proliferation and migration of endothelial cells, resulting in neovascularization. In the case of AMD, the accumulation of drusen (extracellular material deposits) beneath the retina can interfere with the normal function of the RPE and Bruch’s membrane, creating an environment conducive to CNV development.
Risk Factors
There are several risk factors associated with the development of CNV:
- Age: Advanced age is a significant risk factor, especially for CNV caused by AMD.
- Genetics: Genetic predisposition is important, with variations in specific genes, such as CFH and ARMS2, linked to an increased risk of AMD and CNV.
- Smoking: Tobacco use is a well-documented risk factor for the progression of retinal diseases and the development of CNV.
- High Myopia: Severe myopia can cause structural changes in the retina and choroid, which raises the risk of CNV.
- Inflammation: Chronic inflammatory conditions of the eye, such as uveitis, can predispose people to CNV.
- Trauma: Ocular trauma can damage the retinal and choroidal layers, potentially leading to neovascularization.
Clinical Manifestations
The symptoms of CNV vary according to the location and extent of the neovascular growth. The most common clinical manifestations are:
- Blurred Vision: Often the first symptom, caused by fluid buildup and retinal distortion.
- Metamorphopsia: A distortion of vision in which straight lines appear wavy or curved due to retinal photoreceptor displacement.
- Scotomas: Dark or blind spots in the visual field caused by neovascular membranes that interfere with central vision.
- Photopsia: Flashes of light caused by retinal traction or subretinal fluid.
- Reduced Visual Acuity: Progressive loss of sharp vision, particularly in the central visual field, which can significantly impair daily activities.
Associated Conditions
CNV is commonly associated with several ocular conditions, including:
- Age-Related Macular Degeneration (AMD) is the most common cause of CNV, especially in people over the age of 50. If not treated, AMD-related CNV can cause severe central vision loss.
- Pathologic Myopia: High myopia, especially in people with axial elongation of the eyeball, can lead to degenerative changes that promote CNV.
- Angioid Streaks: Breaks in Bruch’s membrane caused by systemic conditions like pseudoxanthoma elasticum can result in CNV.
- Ocular Histoplasmosis Syndrome (OHS): A fungal infection-related condition that can lead to CNV via inflammatory damage to the retina and choroid.
- Central Serous Chorioretinopathy (CSCR): Chronic or recurrent CSCR can cause RPE changes and then CNV.
Pathologic Characteristics
Histologically, CNV is caused by the proliferation of endothelial cells, which form new blood vessels that penetrate the Bruch’s membrane. These vessels frequently lack normal protective barriers, making them susceptible to leakage and hemorrhage. The surrounding tissues may exhibit chronic inflammation, fibrosis, and disruption of normal retinal and choroidal architecture.
Effect on Vision and Quality of Life
CNV can significantly impair vision, particularly central vision, which is required for tasks like reading, driving, and recognizing faces. The impact on vision can significantly reduce quality of life, making it difficult to perform daily activities and increasing reliance on others. The psychological impact of visual impairment, such as anxiety and depression, is also a major concern for patients with CNV.
Advancements in Research
Current research into the molecular mechanisms of CNV has identified a number of potential therapeutic targets. Advances in gene therapy, RNA interference, and the development of novel angiogenesis inhibitors show promise for more effective and less invasive therapies. Understanding the genetic and environmental factors that contribute to CNV remains a major focus, with the goal of developing preventive strategies and personalized treatment approaches.
Epidemiology
The prevalence of CNV varies globally, with higher rates found in areas with a higher incidence of AMD and myopia. CNV associated with AMD is a leading cause of severe visual impairment in elderly people in developed countries. Epidemiological studies have demonstrated the importance of early detection and intervention in preventing irreversible vision loss.
Differential Diagnosis
Distinguishing CNV from other retinal and choroidal conditions is critical for effective treatment. Central serous chorioretinopathy, macular edema, and polypoidal choroidal vasculopathy can all produce similar symptoms and imaging findings. A thorough clinical evaluation and advanced imaging techniques are required for accurate diagnosis.
Prevention Tips
- Regular Eye Examinations: Routine eye exams, particularly for those over 50 or with high myopia, can aid in the early detection and monitoring of retinal conditions that may lead to CNV.
- Healthy Diet: A diet high in leafy greens, fruits, and omega-3 fatty acids improves overall eye health and may lower the risk of retinal disease. Foods rich in antioxidants, such as vitamins A, C, and E, are especially beneficial.
- Smoking Cessation: Avoiding tobacco use is critical because it increases the risk of developing CNV and other retinal conditions.
- UV Protection: Wearing UV-blocking sunglasses can protect your eyes from harmful light exposure, which can lead to retinal damage.
- Manage Chronic Conditions: Properly managing systemic conditions such as hypertension, diabetes, and inflammatory diseases can lower the risk of CNV.
- Avoid Ocular Trauma: Keeping the eyes safe from injuries and avoiding activities that could cause trauma can help prevent conditions that could lead to CNV.
- Monitor Visual Changes: Be aware of any changes in vision, such as blurriness, distorted vision, or dark spots, and seek immediate medical attention if these symptoms occur.
- Genetic Counseling: For people who have a family history of retinal disease, genetic counseling and testing can help them understand their risk and plan preventive measures.
- Reduce Blue Light Exposure: Limiting screen time and using blue light filters on devices can help protect the eyes from potential damage caused by prolonged exposure to blue light.
- Exercise Regularly: Regular physical activity benefits overall health, including eye health, by improving blood circulation and lowering the risk of CNV-causing conditions.
Diagnostic methods
Choroidal neovascularization (CNV) is diagnosed using a combination of clinical evaluation and advanced imaging techniques to accurately identify and assess the condition.
Clinical Examination
The first step in diagnosing CNV is a comprehensive clinical examination by an ophthalmologist, which includes a detailed patient history and visual acuity testing. A dilated fundus examination is required to visualize the retina and choroid, which contain CNV-specific features such as subretinal fluid, hemorrhages, and grayish-green choroidal lesions.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique that produces high-resolution cross-sections of the retina. OCT is extremely useful for detecting and monitoring CNV because it can detect subretinal or intraretinal fluid, retinal thickening, and disruptions in the retinal layers. Enhanced depth imaging (EDI) OCT provides more detailed visualization of the choroid, which aids in the assessment of choroidal involvement.
Fluorescein Angiography(FA)
Fluorescein angiography is performed by injecting fluorescein dye into the retinal and choroidal vasculature via an IV. This imaging technique aids in determining the precise location and size of the neovascular membranes. CNV typically appears as areas of early hyperfluorescence followed by progressive dye leakage in the later phases, indicating abnormal blood vessel growth and leakage.
Indocyanine green angiography (ICG)
Indocyanine green angiography (ICG) uses indocyanine green dye to better visualize the choroidal vasculature than fluorescein angiography. ICG is especially effective for detecting CNV when the lesions are obscured by hemorrhage or pigmentation. It produces detailed images of the choroidal blood vessels, which can aid in distinguishing CNV from other choroidal conditions.
Fundus Autofluorescence (FAF)
Fundus autofluorescence (FAF) imaging detects the natural fluorescence produced by lipofuscin in the retinal pigment epithelium. FAF can aid in detecting areas of RPE dysfunction and damage associated with CNV. This technique is useful for determining the overall health of the retina and tracking disease progression.
Optical Coherence Tomography Angiography(OCTA)
OCTA is a novel imaging modality that allows for detailed visualization of retinal and choroidal blood flow without the need for dye injections. It enables the detection of neovascular networks associated with CNV, demonstrating the extent and activity of the neovascularization. OCTA can also be used to monitor treatment response and detect recurrence.
B-Scan Ultrasonography
When dense media opacities, such as cataracts or vitreous hemorrhage, make direct visualization impossible, B-scan ultrasonography can be used to detect intraocular abnormalities. This technique produces cross-sectional images of the eye, which can aid in the detection of subretinal fluid and retinal detachment associated with CNV.
Treatment
The treatment for choroidal neovascularization (CNV) aims to control abnormal blood vessel growth, reduce fluid leakage, and preserve vision. Standard and emerging therapies are used depending on the severity and underlying cause of CNV.
Anti-VEGF Therapy
Anti-VEGF (vascular endothelial growth factor) therapy is the foundation of CNV management. Intravitreal injections of medications such as ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) inhibit VEGF, a key factor in the development of CNV. These treatments help to reduce neovascular growth and fluid leakage while also improving or stabilizing vision. Regular injections, usually monthly, are required at first, followed by a maintenance schedule based on the patient’s response.
Photodynamic therapy (PDT)
Photodynamic therapy entails administering a photosensitizing agent (verteporfin) via IV before applying a non-thermal laser to the affected area. The activated drug produces reactive oxygen species, which selectively damage the abnormal blood vessels. PDT is less commonly used since the introduction of anti-VEGF therapy, but it is still an option for certain types of CNV, particularly those associated with central serous chorioretinopathy.
Laser Photocoagulation
Laser photocoagulation employs thermal laser energy to coagulate and seal abnormal blood vessels. This treatment is better suited for well-defined, extrafoveal CNV lesions that pose a lower risk of damaging central vision. It has been largely replaced by anti-VEGF therapy, but it is still used in certain cases.
Innovative and Emerging Therapies
Genetic Therapy
Gene therapy is a new field that aims to provide long-term treatment for CNV by delivering genes that encode anti-angiogenic factors directly to the retina. Early clinical trials are looking into the safety and efficacy of this approach, with the goal of reducing the need for multiple intravitreal injections.
RNA Interference (RNAi) Therapies
RNAi therapies target specific messenger RNA (mRNA) molecules to prevent the production of proteins involved in CNV development. These therapies aim to silence the genes responsible for VEGF production, providing a novel approach to treatment.
Combination Therapies
Different treatment modalities, such as anti-VEGF agents with PDT or anti-VEGF agents with corticosteroids, are being investigated to improve therapeutic outcomes. The rationale is that targeting multiple pathways at the same time may improve disease control and reduce the frequency of treatments.
Sustained-Release Implants
Sustained-release drug delivery systems, such as intravitreal implants, are being developed to allow for the controlled release of anti-VEGF agents over time. These implants are intended to reduce the number of intravitreal injections and improve patient compliance.
Novel Anti-Angiogenic Agents
There is ongoing research to develop new anti-angiogenic agents with various mechanisms of action. These agents target alternative pathways involved in neovascularization and are intended to provide additional treatment options for patients who are resistant to current therapies.
Trusted Resources
Books
- Age-Related Macular Degeneration by Jennifer I. Lim
- Retinal Vascular Disease by A.M. Joussen, T.W. Gardner, B. Kirchhof, S.J. Ryan
- Retina by Stephen J. Ryan, SriniVas R. Sadda, David R. Hinton










