What is Choroidal Nevus?
A choroidal nevus is a benign pigmented growth in the choroid, the vascular layer of the eye that lies between the retina and the sclera. A choroidal nevus, similar to a freckle or mole on the skin, is usually asymptomatic and discovered by chance during routine eye exams. While generally harmless, a choroidal nevus should be closely monitored due to the small risk of developing into malignant melanoma, a serious and potentially vision-threatening condition. Understanding the nature, risk factors, and potential complications of choroidal nevi is critical for successful patient management and early detection of malignant changes.
Choroidal Nevus Insights
Choroidal nevi are relatively common, with studies estimating that they affect 5-10% of the general population. These pigmented lesions are made up of melanocytes, which produce melanin, the pigment that gives our skin, hair, and eyes their color. Choroidal nevi are most commonly found in people over the age of 40, with Caucasians having a higher prevalence than other ethnic groups.
Pathophysiology
A choroidal nevus is thought to be congenital, caused by an abnormal accumulation of melanocytes during fetal development. However, unlike cutaneous nevi, choroidal nevi rarely change over time. The exact cause of these conditions is unknown, but genetic and environmental factors may play a role.
Features
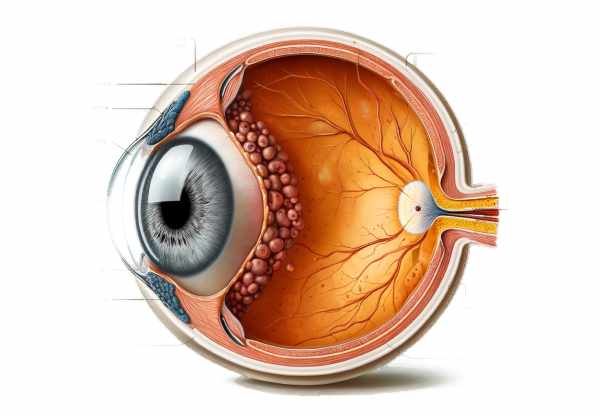
A choroidal nevus is a flat or slightly elevated, variably pigmented lesion on the choroid. These lesions are usually gray to brown in color and may be accompanied by drusen, which are small yellowish deposits that can form on the surface of the nevus. The presence of drusen indicates chronicity and is commonly used to distinguish benign nevi from suspicious lesions. Choroidal nevi are typically less than 5 millimeters in diameter and are commonly found in the posterior segment of the eye, near the optic disc or macula.
Risk Factors
Several factors can impact the development and progression of choroidal nevi:
- Age: The likelihood of detecting a choroidal nevus rises with age.
- Race: Choroidal nevi are more commonly found in people with lighter skin tones, particularly Caucasians.
- Genetics: Having a family history of ocular or cutaneous nevi may increase the risk of developing choroidal nevi.
- Sun Exposure: While the role of UV radiation in the development of choroidal nevi is less certain than that of cutaneous nevi, there is some evidence that excessive sun exposure may contribute to their formation.
Clinical Manifestations
Most choroidal nevi are asymptomatic and do not impair vision. Patients may experience visual disturbances if the nevus is large or close to critical structures like the macula or optic nerve. Symptoms can include:
- Visual Acuity Changes: Blurred or decreased vision if the nevus presses on the macula or other critical areas.
- Metamorphopsia: Distorted vision or visual field defects, especially when associated with retinal detachment or subretinal fluid accumulation.
- Floaters: The perception of floating spots in the visual field caused by nevus-induced secondary changes in the vitreous body.
Potential Complications
While the majority of choroidal nevi are benign throughout life, a small percentage can progress to choroidal melanoma. The risk of transformation is estimated to be one in 8,000 per year. Factors that increase the likelihood of malignancy are:
- Thickness: Nevi that are thicker than 2 millimeters are deemed suspicious.
- Subretinal Fluid: The presence of fluid beneath the retina covering the nevus may indicate active growth and an increased risk.
- Symptoms: A sudden onset of symptoms such as vision changes or photopsia may indicate malignant changes.
- Orange Pigmentation: The presence of orange pigment, most commonly lipofuscin, on the nevus’ surface is a cause for concern.
- Margin Proximity to the Optic Disc: Nevi with a higher risk profile are monitored more closely.
Monitoring and Follow-up
Given the risk of malignant transformation, choroidal nevi must be monitored on a regular basis. Ophthalmologists typically perform periodic eye examinations, including detailed imaging studies, to monitor any changes in the size, shape, or appearance of the nevus. Optical coherence tomography (OCT), fundus photography, and ultrasonography are common methods for documenting and assessing these lesions over time.
Effects on Quality of Life
A choroidal nevus has little impact on the majority of people’s lives. However, the psychological burden of knowing there is a risk of cancer can lead to anxiety and stress. Regular follow-up and clear communication from healthcare providers can help to alleviate these concerns by ensuring patients understand the benign nature of their condition and the importance of ongoing monitoring.
Advancements in Research
Recent advances in ocular imaging and genetic research have provided new insights into the nature of choroidal nevi and their susceptibility to transformation. Researchers are looking into the genetic mutations linked to uveal melanoma in order to better understand how the disease progresses from benign to malignant. Furthermore, advances in imaging technologies, such as enhanced depth imaging OCT and autofluorescence, improve the ability to detect subtle changes in choroidal nevi, potentially leading to earlier intervention and better outcomes.
Epidemiology
Choroidal nevi are found in a variety of populations, with an increased prevalence among older adults and those with lighter skin tones. According to epidemiological studies, while the majority of choroidal nevi remain stable, the small risk of malignancy emphasizes the importance of routine eye exams for early detection and management.
Differential Diagnosis
Differentiating choroidal nevi from other pigmented lesions of the eye is critical for effective treatment. Choroidal melanomas, congenital hypertrophy of the retinal pigment epithelium (CHRPE), and other intraocular tumors can all exhibit similar clinical characteristics. Comprehensive eye exams, including advanced imaging and, in some cases, biopsy, are required to accurately diagnose and distinguish these conditions.
Prevention Tips
- Regular Eye Examinations: Seek routine comprehensive eye exams from an ophthalmologist, especially if you have a family history of ocular conditions or are in a high-risk group.
- Protect Your Eyes from UV Radiation: Wear sunglasses that completely block UVA and UVB rays to reduce potential UV damage to your eyes, which may aid in the prevention or progression of choroidal nevi.
- Monitor for Symptoms: Be aware of any changes in your vision, such as blurriness, visual distortions, or new floaters, and notify your eye care professional right away.
- Maintain a Healthy Lifestyle: A well-balanced diet high in antioxidants, regular exercise, and quitting smoking can all benefit overall eye health and potentially lower the risk of complications associated with choroidal nevi.
- Know Your Family History: If you have a family history of ocular or cutaneous nevi, discuss it with your eye doctor, as it may affect your risk and the frequency of monitoring needed.
- Avoid Prolonged Sun Exposure: To reduce the risk of UV-induced eye damage, limit your exposure to direct sunlight, particularly during peak hours.
- Use Protective Eyewear: When participating in activities that may result in eye injury, such as sports or certain occupations, wear appropriate protective eyewear to avoid trauma that could affect existing nevi.
- Stay Informed: Learn about the signs and symptoms of potentially malignant changes in choroidal nevi so that you can seek medical attention as soon as possible if necessary.
- Follow Up Diligently: Follow your eye doctor’s recommendations for follow-up visits and imaging studies to track the nevus’ progression over time and detect any early signs of change.
Diagnostic methods
A choroidal nevus is diagnosed through a thorough eye examination and the use of advanced imaging techniques to assess the characteristics and track any changes over time.
Clinical Examination
An ophthalmologist performs a detailed clinical examination to diagnose a choroidal nevus. This includes a dilated fundus examination to see the retina and choroid, which allows the doctor to detect any pigmented lesions. The nevus usually appears as a flat or slightly elevated gray to brown lesion in the choroid.
Fundus Photography
Fundus photography is an important tool for capturing the appearance of the nevus. High-resolution images of the retina and choroid are captured, establishing a baseline for future comparisons. This method aids in the tracking of nevus size, shape, and pigmentation changes over time.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining cross-sectional images of the retina and choroid. OCT can detect subtle changes in the choroid’s thickness and structure, as well as the presence of nevus-associated subretinal fluid or drusen. Enhanced depth imaging (EDI) OCT enables better visualization of deeper structures, including the entire thickness of the choroid.
B-scan ultrasonography assesses the thickness and internal reflectivity of the choroidal nevus. This imaging modality aids in the distinction between benign nevi and more suspicious lesions that may necessitate closer monitoring or intervention. Lesions with a high internal reflectivity and a thickness greater than 2 millimeters are considered more serious.
Fundus Autofluorescence (FAF)
Fundus autofluorescence (FAF) imaging detects the natural fluorescence produced by lipofuscin in the retinal pigment epithelium. FAF can detect areas of RPE atrophy or damage, which may be associated with choroidal nevi. This technique is useful for determining the health of the retina above the nevus.
Fluorescein Angiography(FA)
Fluorescein angiography involves injecting fluorescein dye into the bloodstream to visualize blood flow in the retina and choroidal vessels. This technique can assist in detecting any leakage or abnormal vascular patterns associated with the nevus, which may indicate a malignant transformation.
Indocyanine green angiography (ICG)
Indocyanine green angiography (ICG) uses a different dye to better visualize the choroidal vasculature. ICG is particularly useful for detecting choroidal neovascularization and other nevus-related abnormalities.
Choroidal Nevus Treatment Options
primary goal of managing choroidal nevi is to watch for signs of malignant transformation while also treating any symptoms that may arise.
Observation and Monitoring
Most patients with choroidal nevus require only regular observation and monitoring. This includes regular eye exams and imaging studies to monitor any changes in the size, shape, or appearance of the nevus. Patients are usually re-evaluated every 6 to 12 months, depending on the characteristics of the nevus and the presence of any risk factors for malignancy.
Photocoagulation
Laser photocoagulation can be used to treat symptomatic nevi or those that are growing or transforming. This treatment uses focused laser energy to create small burns around the nevus, with the goal of preventing future growth. While photocoagulation is effective, it is used with caution due to the risk of retinal damage and vision loss.
Plaque Radiotherapy
Plaque radiotherapy is a treatment option for nevi that exhibit suspicious characteristics or have progressed to choroidal melanomas. This method involves applying a small radioactive plaque to the surface of the eye, directly over the nevus. The radiation targets and destroys abnormal cells while preserving healthy tissue. Plaque radiotherapy is a localized treatment that can effectively manage malignant transformation while having minimal impact on overall vision.
Transpupillary Thermal Therapy (TTT)
Transpupillary thermotherapy (TTT) is a laser-based treatment that uses heat to eliminate abnormal cells. TTT is less invasive than traditional laser photocoagulation and can be used to treat small choroidal melanomas that develop from nevi. This technique is typically reserved for situations in which other treatments are ineffective.
Enucleation
Enucleation (surgical removal of the eye) may be required in rare cases when the choroidal nevus has progressed to a large or aggressive melanoma. This drastic measure is considered when the primary goal is to stop the spread of cancer and save the patient’s life. Enucleation is typically used as a last resort after other treatments have failed or are no longer feasible.
Emerging Therapies
The search for new treatments for choroidal nevi and their malignant counterparts is ongoing. Advances in genetic therapy, targeted molecular treatments, and immunotherapy point to more effective and less invasive options in the future. These new treatments aim to selectively target abnormal cells while reducing side effects and preserving vision.
Trusted Resources
Books
- Ocular Tumors in Animals and Humans by Hans E. Grossniklaus, Amy C. K. Kuo, and Karla L. Riddle
- Clinical Ophthalmic Oncology: Uveal Tumors by Arun D. Singh and Bertil E. Damato
- Intraocular Tumors: An Atlas and Textbook by Jerry A. Shields and Carol L. Shields






