Introduction to Corneal Dystrophies
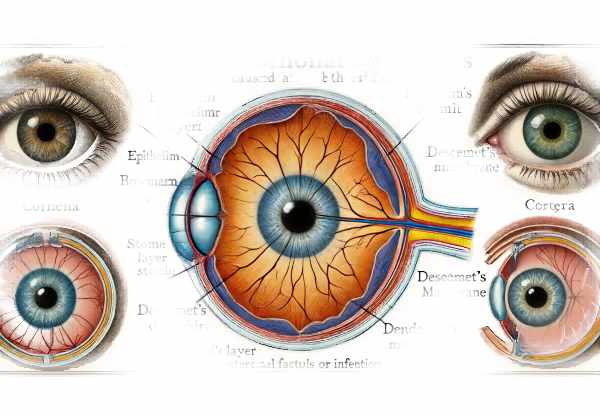
Corneal dystrophies are a group of genetic, often progressive, eye disorders distinguished by the accumulation of abnormal material in the cornea, the clear, front layer of the eyeball. These conditions commonly affect both eyes and are inherited. Corneal dystrophies can have a significant impact on vision and comfort, depending on the type and severity. Unlike corneal degenerations, which are frequently associated with aging or environmental factors, corneal dystrophies are typically present at birth or develop early in life. They can cause blurred vision, discomfort, and, in some cases, severe pain. Understanding the different types of corneal dystrophies, their causes, and the effects on vision is critical for effective management and treatment.
Corneal Dystrophies Insights
Corneal dystrophies are classified according to which layer of the cornea they affect: the epithelium, Bowman’s layer, stroma, Descemet’s membrane, or endothelium. Each type has unique characteristics, but they all share features such as being inherited, bilateral (affecting both eyes), and not caused by external factors such as infection or inflammation.
Types of Corneal Dystrophies
- Epithelial Basement Membrane Dystrophy (EBMD), also known as Map-Dot-Fingerprint Dystrophy, is the most common corneal dystrophy. It affects the epithelial layer and its basement membrane, causing map-like, dot-like, or fingerprint-like patterns on the cornea. Symptoms may include blurred vision, recurring erosions, and discomfort.
- Reis-Bücklers Dystrophy: This condition affects the Bowman’s layer, resulting in the formation of scar tissue. It typically manifests in childhood with symptoms such as recurring erosions, pain, and visual impairment. Scar tissue may cause the cornea to appear cloudy.
- Granular Corneal Dystrophy: Granular dystrophy affects the stroma and is identified by the presence of crumb-like, opaque deposits. These deposits can cause visual disturbances and frequently worsen over time, resulting in severe vision impairment.
- Lattice Corneal Dystrophy: Lattice dystrophy, which also affects the stroma, causes amyloid deposits to form in the form of branching, lattice-like lines. As these deposits build up, they can cause recurring corneal erosion and vision loss.
- Macular Corneal Dystrophy: The accumulation of mucopolysaccharides in the stroma causes diffuse cloudiness and vision impairment. It usually appears in childhood or adolescence and can lead to severe visual disability.
- Fuchs’ Endothelial Dystrophy: This condition affects the endothelium, the innermost layer of the cornea that keeps it clear by pumping out excess fluid. In Fuchs’ dystrophy, endothelial cells gradually die, causing corneal swelling, haziness, and vision loss, particularly in the morning.
- Posterior Polymorphous Corneal Dystrophy (PPCD): This condition affects both Descemet’s membrane and the endothelium. It can result in vesicles, bands, or geographic opacities on the posterior cornea. While it is often asymptomatic, it can also cause visual disturbances and, in rare cases, glaucoma.
Pathophysiology
The pathophysiology of corneal dystrophies is characterized by genetic mutations that result in abnormal synthesis or deposition of various substances within the cornea. Depending on the type of dystrophy, these substances may consist of proteins, lipids, mucopolysaccharides, or amyloid.
- Genetic Basis: The majority of corneal dystrophies are inherited in an autosomal dominant manner, which means that a single copy of the mutated gene from one parent can cause the condition. However, some dystrophies, such as macular corneal dystrophy, have an autosomal recessive inheritance pattern, requiring two copies of the mutated gene, one from each parent.
- Abnormal Deposits: Genetic mutations cause the production of abnormal proteins or other substances, which accumulate in the cornea. For example, in granular dystrophy, hyaline material accumulates, whereas in lattice dystrophy, amyloid deposits develop.
- Cellular Dysfunction: In conditions such as Fuchs’ endothelial dystrophy, endothelial cells do not function properly, resulting in fluid accumulation within the cornea. This fluid buildup causes corneal swelling and haziness, which impairs vision.
- Recurrent Erosions: Many epithelial and Bowman’s layer dystrophies are characterized by recurring corneal erosions. These erosions occur when epithelial cells do not properly adhere to the underlying layers, resulting in pain, tearing, and blurred vision.
Symptoms and Clinical Features
The symptoms of corneal dystrophies differ greatly depending on their type and severity. Common symptoms include:
- Blurred Vision: As abnormal deposits build up, they disrupt the cornea’s transparency and refractive properties, resulting in blurred or distorted vision.
- Pain and Discomfort: Recurrent erosions, especially in dystrophies affecting the epithelium or Bowman’s layer, can cause severe pain and discomfort.
- Glare and Halos: Irregularities on the cornea’s surface can scatter light, resulting in glare, halos, and difficulty seeing in bright light or at night.
- Foreign Body Sensation: Even if no foreign body is present, erosions and surface irregularities can cause the sensation of something being in the eye.
Progress and Impact on Vision
Corneal dystrophies progress at different rates, ranging from slowly advancing conditions that cause gradual vision loss to more aggressive forms that significantly impair vision within a few years. The impact on vision is determined by the location and size of the deposits or structural changes within the cornea.
- Epithelial Dystrophies: These frequently cause recurring erosions and intermittent symptoms, with the possibility of chronic discomfort and fluctuating vision.
- Stromal Dystrophies: Conditions such as granular, lattice, and macular dystrophies usually result in progressive vision loss as deposits accumulate and disrupt corneal clarity.
- Endothelial Dystrophies: Fuchs’ endothelial dystrophy can result in significant visual impairment due to corneal swelling and haziness, especially in the morning when corneal edema is most noticeable.
Genetic Counseling
Given the hereditary nature of corneal dystrophies, genetic counseling may be an important part of patient care. Counseling informs individuals and families about the genetic basis of the condition, the risks of inheritance, and the implications for subsequent generations. Genetic testing may also be available to help identify specific mutations and confirm the diagnosis.
Prevention Tips
- Regular Eye Exams: Schedule routine comprehensive eye exams to detect early signs of corneal dystrophies and track any changes. Early detection can help to manage symptoms and slow their progression.
- Protect Your Eyes: Wear protective eyewear when performing activities that could result in eye injury, such as sports, woodworking, or chemical handling. Preventing trauma can lower the likelihood of exacerbating corneal conditions.
- Avoid Eye Rubbing: Do not rub your eyes, as this can aggravate corneal erosions and increase the risk of complications in conditions such as epithelial basement membrane dystrophy.
- Maintain Good Hygiene: Practice proper eye hygiene, especially if you wear contact lenses. To avoid infections that can exacerbate corneal dystrophies, ensure that lenses are properly cleaned, stored, and replaced on time.
- Manage Underlying Health Conditions: Keep systemic conditions like diabetes and hypertension under control, as they can have an impact on overall eye health. Proper management can reduce the likelihood of exacerbating corneal problems.
- Stay Hydrated: Drink plenty of water to maintain proper tear production and avoid dry eyes, which can exacerbate the symptoms of certain corneal dystrophies.
- Use Lubricating Eye Drops: If you have dry eyes, lubricating eye drops can help keep the corneal surface moist and healthy. This can help to alleviate discomfort and prevent erosion.
- Genetic Counseling: If you have a family history of corneal dystrophies, seek genetic counseling to better understand your risk and take preventative measures. This can also be useful in planning for future generations.
- Protect Against UV Exposure: Wear sunglasses that block 100% of UV rays to shield your corneas from harmful ultraviolet radiation, which can speed up the progression of some corneal dystrophies.
- Follow Prescribed Treatments: To avoid complications and further degeneration, comply with any prescribed treatments or medications for pre-existing eye conditions.
Corneal Dystrophies: Diagnostic Techniques
To accurately determine the type and severity of corneal dystrophies, a combination of clinical evaluations, imaging techniques, and genetic testing is used. Here are the main diagnostic methods used:
- Slit Lamp Examination is the primary diagnostic tool for corneal dystrophies. A slit lamp enables the clinician to examine the cornea at high magnification and illumination, revealing distinctive patterns and deposits associated with various types of dystrophies. This examination aids in determining the specific layer of the cornea affected.
- Corneal Topography: This non-invasive imaging technique measures the surface curvature of the cornea. It is especially effective at detecting irregularities and changes in corneal shape caused by dystrophies. Corneal topography produces detailed, color-coded maps that aid in the diagnosis of conditions such as keratoconus and determining the extent of corneal changes.
- Pachymetry: Pachymetry is the measurement of corneal thickness. This is critical for diagnosing dystrophies characterized by corneal thinning or thickening. Ultrasonic or optical pachymeters provide precise thickness measurements, which are critical for tracking disease progression and planning treatments.
- Ocular Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the cornea, allowing for a thorough examination of each layer. This technique is extremely useful for diagnosing and monitoring dystrophies such as Fuchs’ endothelial dystrophy, in which changes in the endothelial layer and corneal thickness are critical indicators.
- Confocal Microscopy: This advanced imaging technique provides in-vivo, high-resolution images of the cornea at the cellular level. It is especially useful for identifying specific cellular changes and deposits associated with various corneal dystrophies. Confocal microscopy provides detailed images that help distinguish between different types of dystrophies.
- Specular Microscopy: Examines the cornea’s endothelial layer, producing detailed images and cell counts. This is critical for diagnosing and treating Fuchs’ endothelial dystrophy, as endothelial cell density and morphology are important parameters.
- Genetic Testing: Genetic testing can reveal specific mutations linked to corneal dystrophies. This is especially useful for confirming the diagnosis, determining the inheritance pattern, and offering genetic counseling. Advances in genetic testing techniques, such as next-generation sequencing, have increased the ability to detect a wide range of genetic mutations.
- Fluorescein Staining: This procedure involves applying a fluorescent dye to the eye’s surface to highlight corneal irregularities. Under blue light, areas of erosion or damage will fluoresce, making them more visible. This method is effective for detecting recurrent erosions caused by epithelial dystrophies.
Using these diagnostic methods, eye care professionals can accurately diagnose corneal dystrophies, determine the severity of the disease, and devise an appropriate treatment plan.
Corneal Dystrophies: Healing Techniques
Treatment for corneal dystrophies varies according to the type and severity of the condition. We’ll look at standard treatment options as well as innovative and emerging therapies.
Standard Treatments
- Lubricating Eye Drops: Artificial tears and lubricating eye drops are frequently used to alleviate symptoms of dryness and discomfort, especially in dystrophies that cause recurring erosion. These drops help keep the cornea moist and reduce irritation.
- Hypertonic Saline Solutions: To treat conditions such as Fuchs’ endothelial dystrophy, hypertonic saline drops or ointments are used to draw excess fluid from the cornea, reducing swelling and improving vision.
- Soft Contact Lenses: Therapeutic soft contact lenses can act as a protective barrier for the cornea, relieving pain and promoting healing in dystrophies that cause recurring erosions.
- Medications: Anti-inflammatory medications, such as corticosteroid eye drops, can help manage inflammation and reduce the risk of further damage in some dystrophies. Antibiotic drops may also be prescribed to prevent infection in corneal erosions.
- Phototherapeutic Keratectomy (PTK): An excimer laser is used to remove superficial corneal opacities and smooth irregularities, improving vision and alleviating symptoms in a variety of corneal dystrophies. This procedure is especially effective in treating surface dystrophies such as epithelial basement membrane dystrophy.
Innovative and Emerging Therapies
- Corneal Cross-Linking (CXL): CXL is primarily used to treat keratoconus, but it is also being studied for other corneal dystrophies. This treatment consists of applying riboflavin (vitamin B2) eye drops followed by UV light exposure, which strengthens and stabilizes the corneal collagen fibers.
- Descemet Membrane Endothelial Keratoplasty (DMEK): DMEK is an endothelial keratoplasty procedure that only transplants the endothelial layer and Descemet’s membrane. This technique provides faster visual recovery and better outcomes than traditional full-thickness corneal transplants, and it is especially effective for Fuchs’ endothelial dystrophy.
- Stem Cell Therapy: Recent research is looking into the use of stem cells to regenerate damaged corneal tissue. Stem cell therapy shows promise in treating conditions such as limbal stem cell deficiency and other severe corneal dystrophies, with the potential to restore normal cornea function and transparency.
- Gene Therapy: Researchers are looking into advances in gene therapy to correct genetic mutations that cause certain corneal dystrophies. While still in the experimental stage, gene therapy could provide a more targeted approach to treating hereditary corneal disorders, potentially preventing progression.
- Artificial Corneas: For patients who are not suitable for traditional corneal transplants, artificial corneas (keratoprostheses) are an option. These devices can restore vision after other treatments have failed, giving hope to those suffering from severe corneal dystrophies.
- Nanotechnology-Based Treatments: Nanotechnology research is paving the way for novel drug delivery systems in eye care. Nanoparticles can be designed to deliver therapeutic agents directly to the cornea, increasing treatment efficacy while reducing side effects.
The treatment of corneal dystrophies is evolving by combining standard treatments with innovative therapies, providing patients with better outcomes and a higher quality of life.
Trusted Resources
Books
- “Corneal Dystrophies: Diagnosis and Management” by Jay H. Krachmer
- “Corneal Disorders: Clinical Diagnosis and Management” by Howard M. Leibowitz










