What is Corneal Edema?
Corneal edema is characterized by swelling of the cornea, which is the clear, dome-shaped surface that covers the front of the eye. This swelling occurs when fluid accumulates in the corneal layers, resulting in a thickened, cloudy appearance and impaired vision. Corneal edema can be caused by a variety of factors, including trauma, infection, inflammation, and underlying medical conditions like Fuchs’ endothelial dystrophy. It is a significant ocular issue because it affects corneal transparency and thus vision quality. Understanding the underlying mechanisms, symptoms, and risk factors for corneal edema is critical for successful management and prevention.
Corneal Edema Detailed Examination
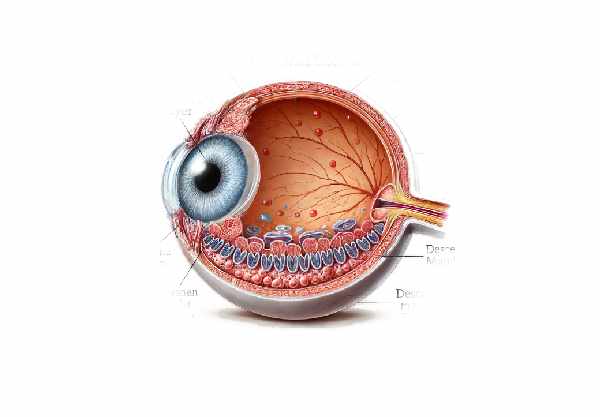
Corneal edema occurs when the cornea’s natural ability to regulate fluid balance is impaired. The cornea consists of five layers: the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium. The endothelium helps keep the cornea clear by pumping excess fluid from the stroma. When endothelial cells are damaged or dysfunctional, fluid accumulates, causing edema.
The causes of corneal edema
- Fuchs’ Endothelial Dystrophy is a genetic disorder in which endothelial cells gradually die off, resulting in chronic corneal edema. It is one of the most common causes of corneal edema, especially among older adults.
- Post-Surgical Edema: Corneal swelling may occur following eye surgeries such as cataract extraction or corneal transplantation. Trauma from surgery can temporarily disrupt the function of endothelial cells, resulting in fluid accumulation.
- Trauma: Physical injuries to the eye, such as a blow or a penetrating wound, can harm the corneal structure and endothelial cells, causing edema.
- Infections: Bacterial, viral, or fungal infections can irritate and damage the cornea, resulting in swelling. Herpes simplex keratitis is a notable example of an infection that can result in significant corneal edema.
- Inflammatory Conditions: Uveitis and other inflammatory disorders can spread to the cornea, resulting in endothelial dysfunction and swelling.
- Contact Lens Overwear: Prolonged use of contact lenses can cause hypoxia (a lack of oxygen) and mechanical stress on the cornea, resulting in edema.
- Glaucoma: In glaucoma, elevated intraocular pressure compresses the corneal endothelium, impairing function and causing fluid buildup.
Symptoms of Corneal Edema
The symptoms of corneal edema vary according to the severity and underlying cause. Common symptoms include:
- Blurred Vision: When the cornea swells, its transparency decreases, resulting in cloudy or blurry vision. Patients may notice a significant decrease in visual acuity, particularly upon waking.
- Halos and Glare: Light scattering from corneal edema can cause patients to see halos around lights and experience increased glare, especially at night or in bright light conditions.
- Eye Pain: Depending on the cause, corneal edema can be uncomfortable or painful. This is particularly true if the edema is caused by trauma or infection.
- Foreign Body Sensation: Corneal swelling can cause irritation and discomfort by giving the sensation that something is in the eye.
- Redness: The eye may appear red and swollen, particularly if the edema is caused by infection or inflammation.
- Photophobia: Increased sensitivity to light is common in corneal edema, making patients uncomfortable in bright environments.
Pathophysiology
The primary cause of corneal edema is disruption of the endothelial pump function. Endothelial cells maintain corneal transparency by actively pumping excess fluid from the stroma. When these cells are damaged or reduced in number, their ability to regulate fluid balance is impaired, resulting in fluid accumulation in the cornea.
- Endothelial Cell Loss: Conditions such as Fuchs’ endothelial dystrophy cause a progressive loss of endothelial cells. As these cells die, the remaining cells grow to cover the defect, but they eventually become overwhelmed, resulting in fluid leakage into the stroma.
- Increased Intraocular Pressure (IOP): High IOP, as seen in glaucoma, can compress endothelial cells and impair their function. This increased pressure can also cause fluid to enter the cornea from the anterior chamber.
- Inflammation and Infection: Inflammatory mediators produced during infections or autoimmune conditions can directly harm endothelial cells or cause secondary inflammation that impairs their function.
- Hypoxia: Prolonged contact lens wear or poor lens hygiene can result in hypoxic conditions, depriving the cornea of essential oxygen. Hypoxia can cause endothelial cell dysfunction and subsequent corneal edema.
Impact on Vision
The effects of corneal edema on vision can be mild to severe, depending on the extent of the swelling and the underlying cause. In mild cases, patients may notice slight blurriness or halos around lights. In more severe cases, vision can become significantly impaired, making daily tasks difficult.
- Mild Edema: Patients may experience occasional blurred vision, especially in the morning. This is due to the cornea naturally swelling during sleep when the eyes are closed, and the tear film is not replenished.
- Moderate Edema: Visual disturbances like halos, glare, and increased light sensitivity become more noticeable. Patients may struggle with activities such as reading, driving, and recognizing faces.
- Severe Edema: The cornea may become visibly cloudy, resulting in legal blindness. Severe pain and discomfort are also common, particularly if the root cause is an infection or trauma.
Progress and Prognosis
The progression of corneal edema is determined by both the underlying cause and the effectiveness of treatment. For example, Fuchs’ endothelial dystrophy progresses slowly over many years, and vision may gradually deteriorate. With appropriate treatment, such as endothelial keratoplasty, the prognosis can be greatly improved.
In cases of post-surgical or traumatic edema, if the underlying cause is addressed promptly, the prognosis is generally favorable, and the cornea can return to normal transparency with appropriate management.
How to Prevent Corneal Edema
- Regular Eye Exams: Schedule routine comprehensive eye exams to detect early signs of corneal edema and other eye conditions. Early detection can help to manage symptoms and slow their progression.
- Protect Your Eyes: Wear protective eyewear when performing activities that could result in eye injury, such as sports, woodworking, or chemical handling.
- Proper Contact Lens Hygiene: To avoid infections and corneal damage, follow the recommended contact lens use guidelines, which include proper cleaning, storage, and timely replacement.
- Manage Underlying Health Conditions: Keep systemic conditions like diabetes and hypertension under control, as they can have an impact on overall eye health. Proper management can help reduce the likelihood of developing corneal problems.
- Prevent Overuse of Contact Lenses: Do not wear contact lenses for longer than recommended, and make sure they fit properly to avoid hypoxia and mechanical stress on the cornea.
- Treat Eye Infections Promptly: If you have an eye infection, seek medical attention right away to avoid complications like corneal edema.
- Control Glaucoma: If you have glaucoma, follow your treatment plan to maintain normal intraocular pressure and protect the corneal endothelium.
- Avoid Eye Rubbing: Do not rub your eyes, especially if they are irritated, as this can aggravate corneal conditions and lead to additional complications.
- Stay Hydrated: Drink plenty of water to maintain proper tear production and avoid dry eyes, which can lead to corneal problems.
- Monitor for Symptoms: Keep an eye out for blurred vision, halos, and eye pain. Seek medical attention as soon as you notice any of these symptoms to prevent the condition from worsening.
Corneal Edema: Diagnostic Techniques
Diagnosing corneal edema requires a combination of clinical exams and advanced imaging techniques to accurately assess the extent of swelling and determine the underlying cause. Here are some of the most common diagnostic methods used:
- Slit Lamp Examination: This is an important tool in the diagnosis of corneal edema. A slit lamp examination involves an ophthalmologist using a specialized microscope to examine the eye under high magnification. This allows for more detailed visualization of the cornea’s layers, which aids in the detection of swelling, cloudiness, and other abnormalities. The slit lamp can also detect associated conditions like corneal guttata in Fuchs’ endothelial dystrophy.
- Pachymetry: The cornea’s thickness is measured using ultrasound or optical coherence tomography (OCT). This test is critical for diagnosing corneal edema because it measures the extent of corneal swelling. Increased corneal thickness is a clear sign of edema.
- Ocular Coherence Tomography (OCT): OCT generates high-resolution, cross-sectional images of the cornea, allowing for a thorough examination of its structure. OCT can detect subtle changes in corneal thickness and layering, making it a valuable tool for diagnosing and monitoring corneal edema. It is especially useful in determining the extent of endothelial damage and fluid accumulation.
- Specular Microscopy: This imaging technique focuses on the corneal endothelium. Specular microscopy produces images of the endothelial cell layer that can be used to assess cell density, size, and shape. Reduced endothelial cell count and abnormal cell morphology may indicate endothelial dysfunction, which is a common cause of corneal edema.
- Fluorescein Staining: This test involves applying fluorescein dye to the eye’s surface to highlight corneal defects. Areas of epithelial disruption will fluoresce in blue light, indicating possible fluid entry points into the cornea. This method is useful in determining the integrity of the epithelial barrier.
- Tonometry: Measuring intraocular pressure (IOP) is critical in the diagnostic process, particularly when glaucoma is suspected. Elevated IOP can compress the corneal endothelium, impairing its function and resulting in edema. Tonometry provides important information about the eye’s pressure status.
- Endothelial Cell Count: Advanced imaging techniques, such as confocal microscopy, can provide an endothelial cell count, which is critical for diagnosing conditions like Fuchs’ endothelial dystrophy. A low cell count or abnormal cell morphology indicate poor endothelial function.
By combining these diagnostic methods, eye care professionals can accurately diagnose corneal edema, determine its severity, and plan the best course of treatment.
Corneal Edema: Treatment Methods
The treatment of corneal edema is intended to reduce swelling, restore corneal clarity, and address the underlying cause. Here are some standard treatment options and innovative therapies:
Standard Treatments
- Hypertonic Saline Solutions: Hypertonic saline eye drops or ointments are frequently used to remove excess fluid from the cornea. These solutions increase the osmotic gradient, causing fluid to flow from the cornea back into the tear film, reducing swelling and improving vision.
- Topical Steroids: When inflammation is a contributing factor, topical corticosteroids may be prescribed to reduce inflammation and prevent additional endothelial damage. However, their use should be closely monitored to avoid potential side effects such as increased IOP.
- Anti-Glaucoma Medications: If high IOP is causing or exacerbating corneal edema, medications to lower eye pressure are required. These medications help to prevent additional endothelial compression and damage, which reduces corneal swelling.
- Contact Lenses: Therapeutic soft contact lenses can serve as a bandage for the cornea, providing symptomatic relief. These lenses help to alleviate the pain and discomfort associated with epithelial disruptions caused by corneal edema.
Innovative and Emerging Therapies
- Endothelial Keratoplasty: In severe cases of endothelial dysfunction, surgical procedures such as Descemet’s Stripping Endothelial Keratoplasty (DSEK) or Descemet’s Membrane Endothelial Keratoplasty (DMEK) may be required. These procedures involve replacing damaged endothelial cells with healthy ones, which effectively restores the cornea’s pumping function and reduces edema.
- Rho Kinase Inhibitors: These new medications have shown promise in stimulating endothelial cell regeneration and reducing corneal edema. Rho kinase inhibitors aid in the repair and proliferation of endothelial cells, potentially providing a non-surgical treatment for endothelial dysfunction.
- Corneal Cross-Linking (CXL): Initially used for keratoconus, CXL is now being studied as a treatment for corneal edema. The procedure strengthens the corneal collagen fibers, which may stabilize the cornea and improve its resistance to fluid accumulation.
- Gene Therapy: Research into gene therapy is ongoing, with the goal of correcting genetic defects that cause conditions such as Fuchs’ endothelial dystrophy. Gene therapy could potentially restore normal endothelial function and prevent corneal edema from forming or worsening.
- Stem Cell Therapy: Stem cell research shows promise for regenerating damaged corneal endothelial cells. Stem cell therapy seeks to replace lost or dysfunctional endothelial cells, restoring the cornea’s fluid-pumping ability and reducing edema.
- Artificial Corneas (Keratoprostheses): For patients with severe corneal edema who are not suitable for traditional corneal transplants, artificial corneas offer an alternative. Keratoprostheses can restore vision when other treatments have failed, resulting in a significant improvement in quality of life.
By combining traditional and novel treatments, eye care professionals can effectively manage corneal edema, improve visual outcomes, and improve patients’ quality of life.
Trusted Resources
Books
- “Corneal Disorders: Clinical Diagnosis and Management” by Howard M. Leibowitz
- “Cornea: Fundamentals, Diagnosis and Management” by Jay H. Krachmer










