Introduction to Diabetic Vitreopathy
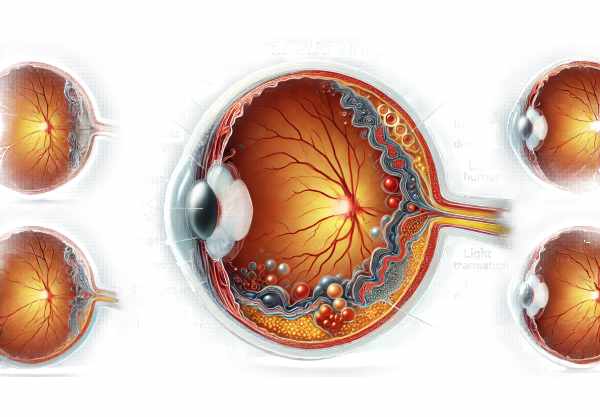
Diabetic vitreopathy is a relatively unknown but significant ocular complication of diabetes mellitus. It entails changes in the vitreous humor, a clear gel-like substance that fills the space between the lens and the retina in the eye. Diabetic vitreopathy can cause symptoms such as floaters, blurriness, and vision impairment, all of which have an impact on quality of life. Understanding the mechanisms, risk factors, and progression of diabetic vitreopathy is critical for early diagnosis and treatment. This condition emphasizes diabetes’s broader impact on ocular health, in addition to diabetic retinopathy, which is well known.
In-Depth Look at Diabetic Vitreopathy
Diabetic vitreopathy is defined as changes in the vitreous humor caused by chronic hyperglycemia and diabetes-related metabolic disturbances. The vitreous humor is essential for the structural integrity of the eye and proper light transmission to the retina. Changes in composition and structure can have a significant impact on vision.
Pathophysiology
The pathophysiology of diabetic vitreopathy is characterized by a series of biochemical and structural changes in the vitreous humor. Chronic hyperglycemia causes the accumulation of advanced glycation end products (AGEs) in the vitreous, which can cause structural proteins like collagen to cross-link and lose flexibility. This causes the vitreous to become more liquefied, a phenomenon known as vitreous syneresis.
Furthermore, diabetes causes the blood-retinal barrier to break down, allowing proteins and other molecules to leak into the vitreous humor and alter its composition. Increased permeability of retinal vessels can cause the accumulation of inflammatory mediators in the vitreous, which contributes to inflammation and further vitreous changes.
Clinical Features
Diabetic vitreopathy frequently manifests with a variety of symptoms that can vary in severity. Common symptoms include:
- Floaters: Patients frequently report seeing floaters, which are small, shadowy shapes that move across the field of vision. These are caused by the aggregation of collagen fibers and other cellular debris within the vitreous.
- Blurred Vision: Changes in the vitreous may cause light to scatter differently as it passes through the eye, resulting in blurred or distorted vision.
- Photopsia: Some patients experience light flashes, also known as photopsia, which occur when the vitreous tugs on the retina.
- Reduced Visual Acuity: In more advanced cases, changes in the vitreous can significantly impair visual acuity, making it difficult to carry out daily activities.
Stages of Diabetic Vitreopathy
Diabetic vitreopathy progresses in stages, depending on the severity of the vitreous changes:
Early Stage:
In the early stages, the vitreous humor may liquefy slightly, and floaters may appear. Visual acuity may remain relatively unchanged, but patients may experience occasional visual disturbances.
The Intermediate Stage:
During the intermediate stage, vitreous syneresis becomes more visible. The increased liquefaction can result in more frequent and visible floaters. Patients may also notice intermittent blurring of vision and increased sensitivity to light.
Advanced Stage:
In the advanced stages, the vitreous humor undergoes significant structural changes. The risk of posterior vitreous detachment (PVD) rises as the vitreous pulls away from the retina. This can result in more severe visual disturbances and a higher risk of retinal tears or detachments.
Risk Factors
Several factors influence the onset and progression of diabetic vitreopathy:
- Diabetes Duration: The longer someone has diabetes, the more likely they are to develop vitreous changes.
- Glycemic Control: Uncontrolled blood sugar levels promote the buildup of AGEs and other harmful molecules in the vitreous humor.
- Diabetic Retinopathy: The presence of diabetic retinopathy, particularly proliferative diabetic retinopathy (PDR), increases the risk of vitreous changes caused by neovascularization and inflammation.
- Hypertension: High blood pressure worsens vascular damage and increases the permeability of retinal vessels, which contributes to vitreous changes.
- Dyslipidemia: High levels of cholesterol and triglycerides are linked to increased oxidative stress and inflammation, which affects the vitreous humor.
Complications
Diabetic vitreopathy can cause a variety of complications, some of which are sight-threatening.
Posterior vitreous detachment (PVD):
PVD is a common complication that occurs when the vitreous humor separates from the retina. While usually harmless, it can increase the risk of retinal tears or detachment if the vitreous pulls on the retina during separation.
Vitreous hemorrhage:
In cases of proliferative diabetic retinopathy, fragile new blood vessels may bleed into the vitreous humor, resulting in vitreous hemorrhage. This can cause sudden vision loss and the formation of dark floaters.
** Retinal Detachment**:
If the vitreous humor pulls too hard on the retina, it can cause retinal tears and subsequent retinal detachment, which is a serious condition that necessitates immediate surgical intervention to avoid permanent vision loss.
Macular edema:
Changes in the vitreous can lead to the development of macular edema, which occurs when fluid accumulates in the macula, the central part of the retina responsible for sharp vision. This can result in significant visual impairment.
Molecular and Biochemical Mechanisms
The molecular mechanisms underlying diabetic vitreopathy include several pathways influenced by chronic hyperglycemia:
AGEs and Crosslinking:
The accumulation of AGEs causes collagen and other structural proteins in the vitreous to cross-link, reducing flexibility and promoting liquefaction.
Oxidative Stress.
Hyperglycemia-induced oxidative stress causes the release of reactive oxygen species (ROS), which harm cellular components and exacerbate vitreous changes.
Inflammatory mediators
The breakdown of the blood-retinal barrier allows inflammatory mediators to enter the vitreous, resulting in chronic inflammation and structural changes.
Proteolytic Enzyme:
Enzymes such as matrix metalloproteinases (MMPs) play a role in vitreous matrix remodeling. In diabetes, dysregulation of these enzymes can result in excessive degradation of vitreous components.
Epidemiology
The prevalence of diabetic vitreopathy varies according to the population studied and the diagnostic criteria used. It is frequently underdiagnosed due to the subtlety of early symptoms and a lack of general awareness among patients and healthcare providers.
Global prevalence:
Diabetic vitreopathy is thought to affect a large proportion of people with long-term diabetes, especially those with poor glycemic control and concurrent diabetic retinopathy.
The Impact on Quality of Life:
Diabetic vitreopathy causes visual disturbances such as floaters and blurred vision, which can have a significant impact on quality of life. These symptoms can disrupt daily activities, reduce productivity, and add to psychological stress.
How to Prevent Diabetic Vitreopathy?
- Maintain Optimal Glycemic Control: Keeping blood glucose levels within the target range is critical for lowering the risk of diabetic vitreopathy and preventing progression.
- Regular Eye Examinations: Have a comprehensive eye exam at least once a year to detect diabetic vitreopathy and other ocular complications.
- Control Blood Pressure: Managing hypertension with lifestyle changes and medications reduces vascular stress and protects the vitreous humor.
- Healthy Diet: Eat a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins to improve overall vascular health and lower oxidative stress.
- Quit Smoking: Smoking cessation is critical for reducing oxidative stress and vascular damage, lowering the risk of diabetic complications.
- Manage Lipid Levels: To reduce vascular risk, regularly monitor and control cholesterol and triglyceride levels with diet, exercise, and medications.
- Stay Physically Active: Regular physical activity can help improve insulin sensitivity, lower blood pressure, and improve overall cardiovascular health.
- Monitor Weight: Maintaining a healthy weight lowers the risk of insulin resistance and related metabolic issues.
- Educate Yourself: Stay informed about diabetes management and potential complications so you can take proactive steps to maintain your health.
- Follow Medical Advice: Follow your healthcare provider’s diabetes management recommendations, which include medication adherence and lifestyle changes.
Diagnostic methods
Diabetic vitreopathy is diagnosed through a combination of standard ophthalmic examinations and advanced imaging techniques that evaluate changes in the vitreous humor and associated retinal structures. Early detection is critical for managing this condition and avoiding future complications.
Complete Eye Examination:
An ophthalmologist’s comprehensive eye examination includes a detailed patient history as well as a visual acuity assessment. A dilated fundus examination allows the ophthalmologist to examine the retina and vitreous for signs of diabetic changes such as floaters, vitreous hemorrhage, or posterior vitreous detachment (PVD).
Fundus Photography*:
Fundus photography is the process of capturing detailed images of the retina and vitreous with a specialized camera. These photographs serve as a baseline and can be compared over time to track the progression of diabetic vitreopathy. Fundus photography is especially useful for determining the extent of vitreous changes and identifying areas of concern.
Optical Coherence Tomography(OCT):
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and vitreous. It is especially useful for detecting and monitoring diabetic macular edema (DME) and vitreous syneresis. OCT can detect subtle changes in vitreous structure and measure retinal thickness, allowing researchers to assess the impact of diabetic vitreopathy on retinal health.
Optical Coherence Tomography Angiogram (OCTA):
OCTA is a more advanced form of OCT that visualizes the retinal and choroidal vasculature without the use of dye. It captures detailed images of blood flow and can detect microvascular changes such as capillary non-perfusion and neovascularization. OCTA is becoming a valuable tool for early detection and monitoring of diabetic vitreopathy and other retinal conditions.
Ultrasound B Scan:
The ultrasound B-scan is a useful tool for evaluating the vitreous and retina, particularly when media opacities such as cataracts or vitreous hemorrhage prevent direct visualization. This imaging modality provides detailed information about vitreous consistency, the presence of PVD, and any retinal detachments.
fluorescein angiography (FA):
FA involves injecting a fluorescent dye into a vein and photographing the dye as it circulates through the retinal vessels. This test detects areas of retinal ischemia, neovascularization, and leakage. While FA is primarily used to diagnose diabetic retinopathy, it can also reveal information about the vitreous and its relationship with the retina.
** Electroretinography (ERG)**:
ERG measures the retina’s electrical responses to light stimulation. It reveals information about the functional state of retinal cells, particularly photoreceptors and inner retinal layers. ERG can help diabetic patients detect early retinal dysfunction and assess the effect of vitreous changes on retinal function.
Advanced Imaging Techniques:
New imaging techniques, such as adaptive optics and hyperspectral imaging, provide detailed views of retinal structures and metabolic changes. These methods show promise for improving the early detection and monitoring of diabetic vitreopathy.
Combining these diagnostic methods results in a comprehensive evaluation of the vitreous and retina, allowing for early detection and precise management of diabetic vitreopathy. Regular screenings and prompt diagnosis are critical for diabetes patients to avoid vision loss and improve their outcomes.
Treatment Options for Diabetic Vitreopathy
The treatment of diabetic vitreopathy focuses on controlling the underlying diabetes, preventing disease progression, and dealing with complications. Standard and emerging therapies both contribute to the comprehensive management of this condition.
** Blood Sugar Control**:
Maintaining optimal blood glucose levels is critical for treating diabetic vitreopathy. Tight glycemic control can help prevent the onset and progression of vitreous changes. Patients are encouraged to monitor their blood glucose levels on a regular basis, to take their medications as prescribed, and to make lifestyle changes such as eating a healthy diet and exercising regularly.
Anti-VEGF Treatment:
Anti-VEGF injections are a common treatment for diabetic macular edema (DME) and proliferative diabetic retinopathy (PDR). Medications like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) prevent the growth of abnormal blood vessels and reduce retinal swelling. These injections can help to stabilize the vitreous and prevent future complications.
Laser Photocoagulation*:
Laser photocoagulation is an established treatment for diabetic retinopathy that can also be used to treat diabetic vitreopathy complications. Focal laser therapy targets specific areas of retinal leakage in DME, whereas pan-retinal photocoagulation (PRP) treats widespread retinal ischemia in PDR. Laser treatment can help seal leaking blood vessels, reduce edema, and prevent the formation of new, abnormal vessels.
Corticosteroids Injections:
Intravitreal corticosteroid injections, such as triamcinolone acetonide and dexamethasone implants, are used to treat DME that does not respond to anti-VEGF therapy. Steroids decrease inflammation and vascular permeability, which reduces retinal swelling. However, they can raise the risk of cataracts and glaucoma, necessitating close monitoring.
Vitrectomy:
Vitrectomy is a surgical procedure used to treat advanced diabetic vitreopathy complications like vitreous hemorrhage and tractional retinal detachment. Vitrectomy involves removing the vitreous gel and replacing it with a saline solution or gas bubble. This procedure helps to remove blood from the vitreous cavity and relieves traction on the retina, preventing further vision loss.
Emerging Therapies:
Innovative treatments and emerging therapies are constantly being investigated to improve outcomes for diabetic vitreopathy patients. This includes:
- Gene Therapy: Studies are underway to develop gene therapies that target specific pathways involved in diabetic vitreopathy. Gene editing tools, such as CRISPR-Cas9, have the potential to correct genetic predispositions and prevent disease progression.
- Neuroprotective Agents: Neuroprotective drugs are designed to preserve retinal neurons and prevent neurodegeneration caused by diabetic vitreopathy. These drugs target the oxidative stress, inflammation, and apoptosis pathways.
- Stem Cell Therapy: Stem cells are being studied for their ability to regenerate damaged retinal cells and restore vision. This novel approach shows promise in treating advanced stages of diabetic vitreopathy.
- Artificial Intelligence (AI): AI and machine learning algorithms are being used in screening and diagnostic processes to improve early detection and personalised treatment plans.
Patient education and support:
It is critical to educate patients on the importance of blood sugar control, regular eye exams, and following treatment plans. Support groups and diabetes education programs can help patients find additional resources and motivation to manage their condition effectively.
Combining these standard and emerging treatments allows for a more comprehensive approach to diabetic vitreopathy management, with the goal of preserving vision and improving patients’ quality of life.
Trusted Resources
Books
- “Diabetic Retinopathy: Evidence-Based Management” by Elia Duh
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Diabetes and Ocular Disease: Past, Present, and Future Therapies” by Ingrid U. Scott










