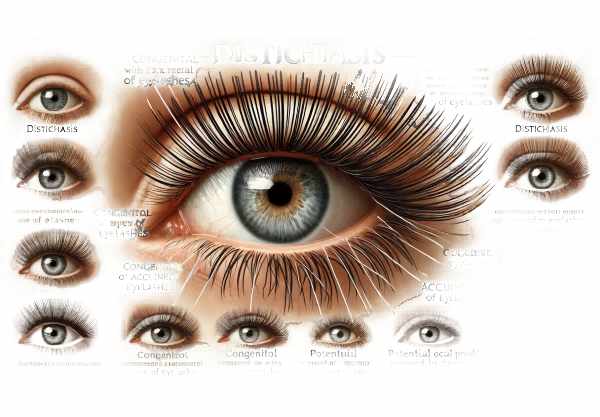
What is Distichiasis?
Distichiasis is an ocular condition marked by the abnormal growth of an extra row of eyelashes from the meibomian glands, which are located along the eyelid edges. These extra lashes can cause significant discomfort and irritation when they come into contact with the cornea and conjunctiva. Distichiasis can be congenital, meaning it was present at birth, or acquired as a result of a variety of underlying conditions. This condition frequently causes symptoms such as redness, tearing, and the sensation of a foreign body in the eye, which can lead to corneal abrasions and ulcers if left untreated. Understanding distichiasis is critical for early detection and treatment to avoid long-term complications.
Detailed Analysis of Distichiasis
Distichiasis is the presence of an extra row of eyelashes, which can result in a variety of ocular problems. There are two types of the condition: congenital and acquired, each with its own set of causes and risk factors.
Pathophysiology
In congenital distichiasis, the meibomian glands, which normally secrete oils to lubricate the eye, develop abnormally into hair follicles, resulting in extra eyelashes. This abnormal development occurs during embryogenesis, resulting in the presence of additional eyelashes at birth. Although these extra lashes are finer and shorter than normal eyelashes, they can cause significant ocular irritation.
Acquired distichiasis, on the other hand, is the result of changes in the eyelid margin caused by a variety of conditions. Chronic inflammation, trauma, or scarring can cause meibomian gland metaplasia, resulting in hair follicles. This type of distichiasis usually appears later in life and is linked to underlying conditions like blepharitis, Stevens-Johnson syndrome, ocular cicatricial pemphigoid, and other inflammatory diseases.
Clinical Features
The clinical manifestation of distichiasis varies depending on the severity and number of abnormal eyelashes. Common symptoms include:
- Ocular Irritation: Patients frequently report a constant feeling of something in their eyes (foreign body sensation), which causes frequent blinking and discomfort.
- Redness and Inflammation: Excess eyelashes can cause chronic irritation to the conjunctiva, resulting in redness and inflammation.
- Excessive Tearing: Tear production may increase in response to irritation caused by extra lashes.
- Corneal Abrasions and Ulcers: Prolonged contact between abnormal eyelashes and the cornea can result in corneal abrasions and, in severe cases, corneal ulcers. These complications can impair vision and cause severe pain.
- Photophobia: Light sensitivity can develop as a result of chronic irritation and inflammation of the ocular surface.
Risk Factors
Several risk factors influence the development of acquired distichiasis:
- Chronic Inflammation: Blepharitis and meibomian gland dysfunction can cause chronic inflammation of the eyelid margins, which increases the risk of developing distichiasis.
- Autoimmune Disorders: Autoimmune diseases like Stevens-Johnson syndrome and ocular cicatricial pemphigoid are high risk factors.
- Trauma and Surgery: Eyelid trauma or previous surgical procedures can change the anatomy of the eyelid margin, potentially resulting in distichiasis.
- Infections: Recurrent eyelid infections, such as herpes zoster ophthalmicus, can lead to the development of distichiasis.
Complications
Untreated distichiasis can result in a variety of complications that affect ocular health and vision:
- Corneal Scarring: Multiple abrasions and ulcers can cause corneal scarring, which can permanently impair vision.
- Infections: Aberrant eyelashes cause corneal damage, which increases the risk of secondary bacterial infections, resulting in keratitis and other complications.
- Vision Loss: Severe corneal involvement and scarring can cause significant vision impairment and, in some cases, blindness.
Differential Diagnosis
It is critical to distinguish distichiasis from other conditions that exhibit similar symptoms.
- Trichiasis: Trichiasis is the misdirection of normal eyelashes toward the cornea. Unlike distichiasis, which causes an extra row of eyelashes from the meibomian glands, trichiasis causes normal lashes to grow inward.
- Ectropion and Entropion: Ectropion (outward turning of the eyelid) and entropion (inward turning of the eyelid) can cause similar symptoms as a result of eyelash contact with the ocular surface, but they are caused by distinct anatomical changes.
- Blepharitis: Blepharitis, or chronic inflammation of the eyelid margins, can cause symptoms similar to distichiasis but does not result in abnormal growth of extra eyelashes.
Epidemiology
The incidence of distichiasis varies greatly depending on the population and underlying conditions. Congenital distichiasis is uncommon, but acquired forms can occur more frequently, especially in association with chronic inflammatory and autoimmune conditions.
Global prevalence:
According to studies, congenital distichiasis is uncommon, affecting only a small percentage of the population. Individuals with underlying inflammatory and autoimmune disorders have a higher risk of developing distichiasis.
Gender and age:
There is no significant gender difference in congenital distichiasis, but acquired forms may be more common in adults, especially those with chronic inflammatory conditions. Age-related changes in the eyelids and meibomian glands can also contribute to the onset of acquired distichiasis.
The Impact on Quality of Life:
Distichiasis symptoms, such as chronic irritation, tearing, and photophobia, can have a significant impact on quality of life. Patients may experience discomfort during daily activities, resulting in decreased productivity and social interactions. Severe corneal involvement can cause significant vision impairment, further affecting the patient’s quality of life.
Reducing Distichiasis Risk
- Regular Eye Examinations: Schedule regular eye exams to detect early signs of distichiasis and other ocular conditions, allowing for prompt treatment.
- Manage Inflammatory Conditions: Reduce your risk of developing distichiasis by effectively managing chronic inflammatory conditions like blepharitis and meibomian gland dysfunction.
- Maintain Eyelid Hygiene: To avoid infections and inflammation, practice good eyelid hygiene, which includes regular cleaning of the eyelid margins.
- Avoid Eyelid Trauma: Keep your eyes safe from trauma and injuries that can change the anatomy of the eyelid margin and lead to distichiasis.
- Monitor for Symptoms: If you notice redness, tearing, or the sensation of a foreign body in your eye, seek medical attention right away.
- Follow Treatment Plans: Stick to treatment plans for underlying conditions that can cause distichiasis, such as autoimmune disorders and infections.
- Use Protective Eyewear: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports or hazardous work environments.
- Stay Hydrated: Stay hydrated to improve overall eye health and meibomian gland function.
- Healthy Diet: Eat a well-balanced diet high in essential nutrients to promote ocular health and lower the risk of inflammatory conditions.
- Consult Specialists: If you have a family history of distichiasis or other ocular conditions, seek personalized advice and management strategies from an ophthalmologist or specialist.
Diagnostic Techniques for Distichiasis
A comprehensive eye examination and several specialized tests are required to accurately diagnose distichiasis and assess its impact on ocular health. Early and accurate diagnosis is critical for successful management and prevention of complications.
Complete Eye Examination:
A thorough eye examination by an ophthalmologist is the first step in diagnosing distichiasis. This involves assessing the patient’s medical history, symptoms, and visual acuity. The examination focuses on the eyelid margins, conjunctiva, and cornea to detect extra eyelashes and assess any associated irritation or damage.
Slit Lamp Examination:
A slit-lamp examination provides a magnified view of the eye structures, allowing for close examination of the eyelid margins, conjunctiva, and cornea. This examination detects the extra row of eyelashes that is characteristic of distichiasis, as well as any associated corneal abrasions, ulcers, or inflammation.
Eyelid Eversion*:
Eyelid eversion entails gently flipping the eyelid inside out to better see the meibomian gland openings and the location of the extra eyelashes. This technique is especially useful for detecting fine and short aberrant lashes that would be difficult to see otherwise.
** Fluorescein Staining**:
Fluorescein staining is a diagnostic test that identifies areas of corneal damage. Fluorescein dye is applied to the ocular surface, and the eye is examined using blue light. Areas of corneal abrasion or ulceration will fluoresce, indicating the degree of damage caused by the abnormal eyelashes.
photographic documentation:
High-resolution digital photography of the eyelid margins and ocular surface can help document the presence and severity of distichiasis. These images serve as a baseline for monitoring disease progression and treatment efficacy.
Meibography:
Meibography is a technique for imaging the meibomian glands located within the eyelids. This non-invasive test evaluates the structure and function of the meibomian glands, which can be affected by distichiasis. Meibography produces detailed images of the glandular architecture and aids in the identification of any pathological changes.
Tear Film Analysis:
Analyzing the tear film can reveal information about the stability and quality of the tear layer, which may be compromised in patients with distichiasis. Tear break-up time (TBUT) and tear osmolarity tests can help determine how distichiasis affects tear film stability and ocular surface health.
Confocal microscopy:
Confocal microscopy is a cutting-edge imaging technique that produces cellularly detailed images of the cornea and conjunctiva. This test detects microscopic changes in the ocular surface and determines the extent of damage caused by the extra eyelashes. Confocal microscopy is especially useful in determining the severity of corneal involvement.
Genetic Test:
Genetic testing may be recommended for patients with congenital distichiasis in order to identify specific genetic mutations linked to the condition. This information can be useful for family counseling and understanding hereditary patterns of distichiasis.
Combining these diagnostic methods enables a thorough evaluation of distichiasis, resulting in an accurate diagnosis and effective management. Regular follow-up exams are required to track disease progression and evaluate the efficacy of treatment options.
Distichiasis Treatment Strategies
The treatment of distichiasis focuses on symptom relief, avoiding complications, and addressing the root causes. To effectively manage this condition, both standard and innovative treatments are used.
Lubricating Eye Drops and Ointments
Lubricating eye drops and ointments can help relieve the irritation caused by extra eyelashes. These products help to protect the ocular surface by keeping moisture in and reducing friction between the lashes and the cornea. They are especially effective for treating mild cases of distichiasis and patients awaiting more definitive treatment.
Epilation:
Epilation is the manual removal of abnormal eyelashes using fine forceps. While this provides immediate relief, the eyelashes frequently regrow, necessitating subsequent treatments. Epilation is a simple and non-invasive method, but it may not be appropriate for long-term management due to the frequent recurrence of lashes.
Cryotherapy:
Cryotherapy is a procedure that uses extremely cold temperatures to destroy the hair follicles of abnormal eyelashes. This treatment has the potential to provide longer-lasting results than epilation. Cryotherapy is performed with a cryoprobe, which applies cold temperatures to the eyelid margins, effectively removing unwanted lashes. However, there is a possibility of collateral damage to adjacent tissues.
Electrolysis:
Electrolysis is the application of an electric current to hair follicles, which destroys them and prevents regrowth. This method is effective for permanently removing extra eyelashes, but it requires precision to avoid damaging adjacent tissues. Electrolysis is typically done in a series of sessions to achieve the best results.
Laser ablation:
Laser ablation employs focused laser energy to target and destroy hair follicles. This technique allows for the precise and effective removal of abnormal eyelashes while causing minimal damage to the surrounding tissues. Laser ablation can provide long-term relief from distichiasis and is widely preferred due to its accuracy and low recurrence rates.
Surgical options:
In severe cases of distichiasis, surgical intervention may be required. Surgery options include:
- Eyelid Margin Resection: This procedure involves the removal of a section of the eyelid margin that contains the abnormal hair follicles. It is effective at removing the source of the extra eyelashes, but it necessitates careful surgical technique to avoid disrupting eyelid function.
- Tarsal Rotation: Tarsal rotation surgery involves repositioning the tarsal plate (a dense connective tissue structure within the eyelid) to direct the growth of abnormal eyelashes away from the ocular surface. This procedure can treat both congenital and acquired distichiasis.
- Anterior Lamellar Recession: This surgery involves the recession of the anterior lamella (the front layer of the eyelid) to remove or redirect the abnormal eyelashes. It is especially beneficial for patients with severe eyelid margin involvement.
Innovative and Emerging Therapies:
Advances in medical research and technology are leading to the development of new treatments for distichiasis.
- Regenerative Medicine: Research into regenerative medicine seeks to repair and restore normal function of the meibomian glands, potentially preventing the formation of abnormal eyelashes.
- Gene Therapy: Gene therapy shows promise in treating congenital distichiasis by correcting the genetic mutations that cause the condition. Although this approach is still in the experimental stage, it has the potential to provide a long-term solution.
- Targeted Anti-Inflammatory Treatments: Creating targeted anti-inflammatory treatments can aid in managing the underlying inflammatory conditions that contribute to acquired distichiasis, lowering the risk of recurrence.
Patient education and support:
It is critical to educate patients about distichiasis, its potential complications, and the treatment options available. Support groups and resources can offer additional information and emotional support, assisting patients in coping with their condition and adhering to treatment plans.
Combining these established and emerging treatments allows for a more comprehensive approach to distichiasis management, with the goal of reducing symptoms, preventing complications, and improving patients’ quality of life.
Trusted Resources
Books
- “Ocular Surface Disease: Cornea, Conjunctiva, and Tear Film” by Edward J. Holland
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski






