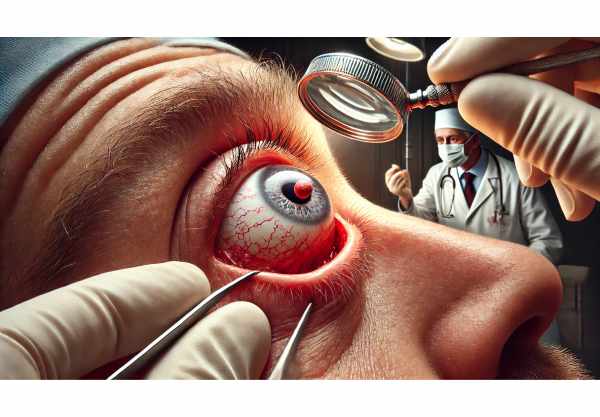
What is a Foreign Body in Eye?
A foreign body in the eye is any external object or substance that enters and remains within the eye. This can include everything from small particles like dust, sand, and metal shavings to larger objects like glass fragments. Such incidents are common and can occur in a variety of settings, including the workplace, at home, and during outdoor activities. The presence of a foreign body in the eye can cause significant discomfort, irritation, and potential injury, necessitating immediate attention to avoid complications.
In-depth Examination of Foreign Body in Eye
A foreign body in the eye is a common ocular emergency that can arise from a variety of activities and environments. Understanding the nature, causes, and possible outcomes of this condition is critical for effective management and prevention.
Types of Foreign Bodies
Foreign bodies can be classified according to their nature and the material they are made of.
- Superficial Foreign Bodies: These are commonly found on the eye’s surface, such as the conjunctiva or cornea. Common examples include dust, sand, eyelashes, and small insects.
- Embedded Foreign Bodies penetrate the eye’s surface and lodge in deeper structures. Examples include metal shards, wood splinters, and glass fragments.
- Chemical Foreign Bodies: Acids, alkalis, and other chemicals can burn and damage eye tissues.
Common Causes
Foreign bodies can enter the eye for a variety of reasons, many of which are related to specific activities or environments:
- Occupational Hazards: People who work in construction, metalworking, or woodworking are more likely to be exposed to particles and debris.
- Outdoor Activities: Sports, gardening, and other recreational activities can result in foreign objects such as dirt, insects, or plant materials entering the eye.
- Household Incidents: Cooking, cleaning, and handling household chemicals are all potential hazards.
Symptoms
The symptoms of a foreign body in the eye differ depending on the size, type, and location of the object. Common symptoms include:
- Pain and Discomfort: The sensation of something in the eye, which is commonly described as gritty or sharp pain.
- Redness and Irritation: An inflammation of the eye caused by irritation or injury.
- Tearing: Increased tear production as a natural response to removing the foreign object.
- Blurred Vision: Visual disturbances that can be temporary or permanent, depending on their severity.
- Photophobia: Light sensitivity, often accompanied by squinting or difficulty opening one’s eyes.
- Swelling: Swelling of the eyelids or surrounding tissues caused by trauma or irritation.
Pathophysiology
When a foreign object enters the eye, it can cause mechanical disruption and inflammation of the surrounding tissues. The first response is the activation of the body’s defense mechanisms to remove the object and repair the damage. This includes:
- Tear Production: The lacrimal glands secrete tears to remove the foreign body.
- Inflammation: The immune system uses inflammation to contain and repair the affected area.
- Fibrosis: If the foreign body causes significant damage, scar tissue may develop as part of the healing process.
Complications
A foreign body in the eye can cause a variety of complications if not treated promptly and appropriately.
- Corneal Abrasion: Foreign object-induced scratches on the corneal surface that can cause pain and visual disturbances.
- Infection: A foreign body can introduce bacteria or fungi into the eye, resulting in infections like conjunctivitis or keratitis.
- Corneal Ulcer: Persistent irritation and damage to the cornea can cause the formation of serious ulcers that require immediate medical attention.
- Iritis: Inflammation of the iris that causes pain, light sensitivity, and blurred vision.
- Vision Loss: Severe or untreated cases can result in partial or complete vision loss, particularly if the foreign body damages the cornea or other critical structures.
Differential Diagnosis
Differentiating a foreign body in the eye from other ocular conditions is critical for effective treatment. The following conditions may cause similar symptoms:
- Conjunctivitis: Inflammation of the conjunctiva, usually caused by infection or allergies.
- Dry Eye Syndrome: Insufficient tear production causes dryness and irritation.
- Blepharitis: Inflammation of the eyelid margins, which can cause discomfort and a gritty sensation.
- Eyelash or Debris: An eyelash or other small debris can cause symptoms similar to a foreign body.
Risk Factors
Certain factors may increase the likelihood of a foreign body incident:
- Occupational Exposure: Work with machinery, chemicals, or airborne particles.
- Lack of Protective Eyewear: Failure to wear safety glasses or goggles in potentially hazardous environments.
- Environmental Conditions: Windy, dusty, or polluted conditions may heighten the risk.
- Recreational Activities include sports and outdoor activities that do not require proper eye protection.
Diagnostic Tools for Foreign Body in Eye
Diagnosing a foreign body in the eye requires a thorough approach to accurately determining the object’s presence and location, as well as assessing any associated damage. Here are the main diagnostic methods:
Clinical Examination
A thorough clinical examination by an ophthalmologist is the first step in diagnosing a foreign body in the eye. Key components are:
- Patient History: Obtaining details about the incident, such as the type of foreign body, the circumstances of entry, and the onset of symptoms.
- Visual Acuity Test: Evaluates the patient’s vision to identify any changes or impairments.
- Slit-Lamp Examination: A slit lamp is used to closely examine the eye’s surface and structures, providing detailed visualization of the foreign body and any associated injuries.
- Fluorescein Staining: The application of fluorescein dye to the eye to highlight corneal abrasions or foreign bodies. The dye illuminates under blue light, making it easier to detect damage.
Imaging Techniques
Advanced imaging techniques may be required to locate deeply embedded foreign bodies or assess the extent of damage.
- X-Rays are useful for detecting radiopaque foreign bodies like metal or glass.
- CT Scans: Provide detailed images of the eye’s internal structures, which are useful for locating non-metallic foreign bodies and evaluating associated injuries.
- Ultrasound: Can be used to see foreign bodies and assess damage, especially when other imaging methods are inconclusive.
Additional Tests
In some cases, additional tests may be necessary to confirm the diagnosis and plan treatment:
- Culture and Sensitivity Tests: If an infection is suspected, samples can be collected to identify the causative organism and determine the best antibiotic treatment.
- Tonometer: Measures intraocular pressure to look for complications like secondary glaucoma.
Managing Foreign Body in Eye
Treatment for a foreign body in the eye focuses on removing the object, relieving symptoms, and avoiding complications like infection or further injury. Here are the standard treatment options and some innovative approaches that are currently being investigated:
Standard Treatment Options:
- Immediate Flushing: The first step in treating superficial foreign bodies is usually to flush the eye with saline or clean water. This can help wash away small particles such as dust or sand.
- Manual Removal: If flushing fails to remove the foreign body, an ophthalmologist may use specialized tools to carefully extract it. This procedure is typically carried out under a slit-lamp microscope for precision.
- Topical Anesthetics: Prior to removal, topical anesthetic drops are used to numb the eye and reduce discomfort during the procedure.
- Antibiotic Eye Drops/Ointments: Following removal, antibiotic eye drops or ointments are prescribed to prevent infection. This is especially important if the foreign body left an abrasion or open wound.
- Anti-inflammatory Medications: To reduce inflammation and pain, anti-inflammatory drops or oral medications may be recommended.
- Patching the Eye: In some cases, the eye may be patched to keep it closed and protected while it heals, particularly if there has been significant abrasion or trauma.
- Surgical Intervention: If a foreign body is deeply embedded or complications arise, surgical intervention may be required. This may include procedures to repair corneal lacerations or remove foreign objects from deeper eye structures.
Innovative and Emerging Therapies
- Advanced Imaging for Precision: The use of high-resolution imaging techniques, such as optical coherence tomography (OCT) and 3D imaging, improves the accuracy of foreign body detection and removal, lowering the risk of complications.
- Minimally Invasive Techniques: Novel minimally invasive surgical techniques and instruments are being developed to improve the safety and efficacy of foreign body removal.
- Biodegradable Antibiotic Inserts: Researchers are looking into the use of biodegradable antibiotic inserts that can be placed in the eye to provide long-term medication release, reducing the need for frequent drops.
- Laser-Assisted Removal: In some cases, laser technology is being used to aid in the removal of foreign bodies, providing a more controlled and precise approach.
- Stem Cell Therapy: For severe corneal injuries caused by a foreign body, stem cell therapy is a new field that seeks to regenerate damaged corneal tissue and restore vision.
- Innovative Drug Delivery Systems: Researchers are looking into new drug delivery systems, such as nanoparticle-based drops, to improve the effectiveness and duration of medications used after removal.
By combining standard treatments with innovative approaches, healthcare providers can better manage foreign body incidents in the eye, improving patient outcomes and lowering the risk of complications.
Tips to Avoid Foreign Body in Eye
- Wear Protective Eyewear: Always wear safety glasses or goggles when participating in activities that could result in eye injury, such as construction, metalworking, gardening, or playing sports.
- Caution with Chemicals: Handle chemicals with care and wear appropriate protective gear, such as goggles or face shields, to avoid splashes and accidental contact with the eyes.
- Be Aware of Environmental Hazards: Wear protective eyewear in windy, dusty, or polluted areas to protect your eyes from airborne particles.
- Implement Workplace Safety Protocols: In occupational settings, follow safety protocols and wear provided protective equipment to reduce the risk of eye injuries.
- Properly Maintain and Clean Eyewear: Keep your protective eyewear in good condition and clean, as damaged or dirty glasses can jeopardize protection.
- Avoid Rubbing Your Eyes: If you feel something in your eye, don’t rub it because it can embed the foreign body deeper. Instead, flush the eye with water or a saline solution.
- Store Household Items Securely: Keep household items that can cause eye injuries, such as sharp tools, chemicals, and cleaning agents, out of the reach of children.
- Educate on Eye Safety: Teach family members, particularly children, about the importance of eye safety and the proper use of protective eyewear.
- Regular Eye Exams: Routine eye exams can help detect potential problems early and keep your eyes healthy and protected.
Individuals who follow these preventive measures can significantly reduce their risk of encountering foreign bodies in their eyes while also maintaining good ocular health.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn and Dante J. Pieramici
Online Resources
- American Academy of Ophthalmology: AAO
- National Eye Institute: NEI
- Mayo Clinic: Mayo Clinic
- American Optometric Association: AOA