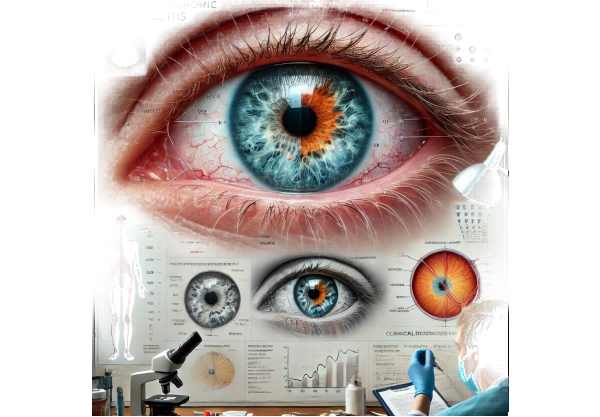
What is Fuchs Heterochromic Iridocyclitis?
Fuchs’ Heterochromic Iridocyclitis (FHI) is a chronic, usually unilateral inflammatory condition of the eye. It is distinguished by an unusual combination of iris color changes (heterochromia), low-grade anterior uveitis (iridocyclitis), and the presence of small, white keratic precipitates on the corneal endothelium. If not treated properly, this condition can result in complications such as cataracts and glaucoma. Although the exact cause is unknown, it is thought to be a rare and relatively benign condition that develops gradually and progresses slowly.
Comprehensive Investigation of Fuchs’ Heterochromic
Iridocyclitis
Fuchs’ Heterochromic Iridocyclitis (FHI), first described by Ernst Fuchs in 1906, is an intriguing ocular condition with distinct clinical features. FHI requires a thorough examination of its pathophysiology, clinical presentation, associated complications, and epidemiology.
Pathophysiology
The exact cause of FHI is unknown, but several hypotheses have been proposed, including infectious, autoimmune, and genetic factors. Some studies link rubella, herpes simplex virus, and toxoplasmosis, while others suggest an autoimmune response targeting the iris and ciliary body. The condition primarily affects the anterior segment of the eye, resulting in chronic low-grade inflammation.
Clinical Presentation
FHI is distinguished from other types of uveitis by the following symptoms and signs:
- Heterochromia: One of the most distinguishing features of FHI is heterochromia, in which the affected eye appears lighter than the unaffected eye. This change is caused by the loss of stromal melanocytes in the iris, which leads to depigmentation. However, heterochromia is not always present, making it a less reliable diagnostic feature in certain situations.
- Low-Grade Anterior Uveitis: Inflammation in FHI is typically mild and chronic, affecting the anterior segment of the eye (iris and ciliary body). Unlike other types of uveitis, FHI usually does not cause significant pain, redness, or photophobia. The inflammation is often so subtle that it goes unnoticed until complications arise.
- Keratic Precipitates: Small, white, stellate-shaped keratic precipitates (KPs) on the corneal endothelium are a characteristic of FHI. These precipitates are usually scattered across the corneal surface and can remain for months or even years.
- Anterior Chamber Cells and Flare: The anterior chamber may have a mild presence of inflammatory cells and a flare, indicating ongoing inflammation.
Complications
Although FHI is generally a benign condition, it can cause a number of complications if not properly managed:
- Cataracts: Cataracts are the most common FHI-related complication. Chronic inflammation associated with FHI accelerates lens opacification, resulting in vision impairment. Cataracts in FHI patients typically develop slowly but can become visually significant over time.
- Glaucoma: Increased intraocular pressure (IOP) in FHI may result in secondary glaucoma. Chronic inflammation causes trabecular meshwork damage, as well as the deposition of inflammatory cells, which contribute to IOP elevation.
- Vitreous Opacities: In some cases, patients with FHI may develop opacities in the vitreous body, which can worsen vision.
Epidemiology
FHI is a rare condition, accounting for only 1-3% of all uveitis cases. It affects both men and women equally and can develop at any age, but it is most commonly diagnosed in young to middle-aged adults. The condition is typically unilateral, meaning that only one eye is affected, though bilateral cases have been reported.
Differential Diagnosis
FHI must be distinguished from other types of uveitis and conditions with similar characteristics. Differential diagnosis includes:
- Herpetic Uveitis: Caused by the herpes simplex or herpes zoster virus, this type of uveitis is characterized by increased inflammation, pain, and corneal involvement, including dendritic keratitis.
- Posner-Schlossman Syndrome: This condition, characterized by recurrent episodes of elevated IOP and mild anterior uveitis, is similar to FHI. Posner-Schlossman syndrome, on the other hand, is distinguished by the absence of the characteristic heterochromia and persistent keratic precipitates found in FHI.
- HLA-B27 Associated Uveitis: Symptoms include acute, recurring episodes of anterior uveitis accompanied by pain, redness, and photophobia. This type of uveitis is frequently associated with systemic conditions such as ankylosing spondylitis.
- Sarcoidosis is a multisystem inflammatory disease that can result in uveitis. Sarcoidosis-related uveitis is often characterized by granulomatous inflammation and can affect both the anterior and posterior segments of the eye.
Pathologic Findings
The histopathological examination of FHI-affected eyes reveals chronic inflammatory changes in the iris and ciliary body, as well as the loss of iris pigment epithelial cells. Another notable finding is the presence of stellate-shaped keratin precipitates on the corneal endothelium. Despite these changes, the overall architecture of the eye remains relatively intact when compared to other types of uveitis.
Effect on Vision and Quality of Life
The effect of FHI on vision and quality of life varies according to the severity of complications like cataracts and glaucoma. Patients in the early stages may not notice any significant visual disturbances. However, as cataracts progress or glaucoma develops, vision can be severely impaired, affecting daily activities and overall quality of life.
Genetic and Infectious Theories
While the exact etiology of FHI remains unknown, several theories have been proposed:
- Infectious Theory: Some studies have linked FHI to viral infections such as rubella, herpes simplex virus, and toxoplasmosis. These infections may cause an immune response, resulting in chronic inflammation in the eye.
- Genetic Theory: Although FHI is not usually inherited in a straightforward Mendelian manner, genetic predisposition may play a role. Certain genetic markers have been linked to the condition, implying that some people are more likely to develop it.
Diagnostic methods
Fuchs’ Heterochromic Iridocyclitis is diagnosed using a combination of clinical evaluation, imaging studies, and laboratory tests.
Clinical Evaluation
- Slit-Lamp Examination: A thorough examination with a slit lamp microscope allows the ophthalmologist to see the characteristic signs of FHI, such as heterochromia, keratic precipitates, and mild anterior chamber inflammation. This is frequently the first step in diagnosing the problem.
- Tonometry: Measuring intraocular pressure (IOP) is critical for detecting any elevation that may indicate secondary glaucoma. Tonometry is useful for tracking disease progression and treatment efficacy.
- Dilated Fundus Examination: This examination evaluates the posterior segment of the eye for signs of vitreous opacities or other abnormalities that may be associated with FHI.
Imaging Studies
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT produces high-resolution images of the anterior segment structures, assisting in determining the extent of inflammation and detecting subtle changes in the corneal endothelium and iris.
- Ultrasound Biomicroscopy (UBM): UBM is useful for assessing anterior segment structures in greater detail, especially when standard slit-lamp examination is inconclusive.
Lab Tests
- Serology: Blood tests may be used to rule out infectious causes of uveitis, including herpes simplex virus, rubella, and toxoplasmosis. Although these infections are not definitively linked to FHI, serology can aid in differential diagnosis.
- Polymerase Chain Reaction (PCR): PCR analysis of aqueous humor samples can detect viral DNA or RNA, indicating an infectious cause.
Additional Diagnostic Tools
- Gonioscopy: This test examines the anterior chamber angle for abnormalities that may predispose to glaucoma. It is particularly useful for monitoring patients with high IOP.
- Fluorescein Angiography: Although not commonly used to diagnose FHI, fluorescein angiography can help assess the blood-retinal barrier and rule out other causes of uveitis.
Treatment for Fuchs’ Heterochromic Iridocyclitis
Treatment for Fuchs’ Heterochromic Iridocyclitis (FHI) aims to alleviate symptoms, reduce inflammation, and prevent complications like cataracts and glaucoma. The approach varies according to the severity of the condition and the presence of any associated complications.
- Topical Steroids are used to reduce inflammation in the anterior segment of the eye.
- Administration: Steroid eye drops are commonly used in mild cases to control chronic low-grade inflammation. Regular monitoring is required to avoid potential complications, such as increased intraocular pressure and cataract formation.
- Management of Intraocular Pressure (IOP): – Medications: Patients with high IOP can use beta-blockers, prostaglandin analogs, carbonic anhydrase inhibitors, or alpha agonists to reduce IOP and prevent glaucoma.
- Surgical Interventions: If medical management is ineffective, surgical procedures such as trabeculectomy or the implantation of glaucoma drainage devices may be required to control IOP.
- Indication for cataract surgery: Many patients with FHI develop cataracts, which can severely impair vision.
- The Procedure: Cataract extraction with intraocular lens implantation is a common procedure. Because of the possibility of chronic inflammation complications, such as zonular weakness, special care must be taken during surgery.
Innovative and Emerging Therapies
- Intravitreal Injections: – Anti-VEGF Agents: These injections are primarily used for macular edema, but are also being studied for their potential to manage inflammation and neovascularization in FHI.
- Steroid Injections: Intravitreal steroids may have longer-lasting anti-inflammatory effects than topical steroids.
- Laser Therapy includes Selective Laser Trabeculoplasty (SLT). This procedure lowers IOP by increasing the outflow of aqueous humor through the trabecular meshwork. It is a less invasive alternative to surgical intervention that can be especially beneficial for patients with FHI-related glaucoma.
- Advanced Imaging and Monitoring includes OCT and UBM. These imaging techniques enable more precise monitoring of disease progression and treatment response, allowing therapies to be tailored to each patient’s specific needs.
- Immunomodulatory Therapy: – Biologic Agents: Research into biologic agents targeting specific immune pathways could provide more effective treatment for chronic uveitis conditions like FHI.
Combining these standard treatments with novel approaches allows healthcare providers to provide more comprehensive and effective management of Fuchs’ Heterochromic Iridocyclitis, potentially improving outcomes and quality of life for affected individuals.
Best Ways to Avoid Fuchs’ Heterochromic iridocyclitis
While it may be impossible to completely prevent Fuchs’ Heterochromic Iridocyclitis due to its unknown cause, certain practices can help manage the risk and prevent complications.
- Regular Eye Examinations: Schedule routine eye exams, especially if you have a family history of uveitis or other ocular conditions. Early detection can help to manage the condition more effectively.
- Prompt Treatment of Infections: Treat any eye infections as soon as possible and thoroughly to reduce the risk of complications that may lead to uveitis.
- Manage Systemic Conditions: Manage systemic inflammatory or autoimmune diseases that may increase the risk of uveitis with appropriate medical care.
- Monitor Symptoms: Keep an eye out for any changes in vision, eye discomfort, or signs of inflammation, and seek medical attention right away if any of these symptoms appear.
- Protect Your Eyes: Wear protective eyewear when participating in activities that could result in eye injury or exposure to infectious agents.
- Healthy Lifestyle: Maintain a healthy lifestyle that includes a well-balanced diet high in antioxidants, regular exercise, and adequate hydration to support overall vision health.
- Avoid Smoking: Smoking increases the risk of developing many eye diseases. To minimize your risk, avoid smoking and limit your exposure to secondhand smoke.
Individuals who follow these preventive measures can better manage their risk and potentially reduce their chances of developing complications from Fuchs’ Heterochromic Iridocyclitis.
Trusted Resources
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Peter J. Garg
Online Resources
- American Academy of Ophthalmology: AAO
- National Eye Institute: NEI
- American Uveitis Society: AUS
- Mayo Clinic: Mayo Clinic






