Basics of Tumor-Related Glaucoma
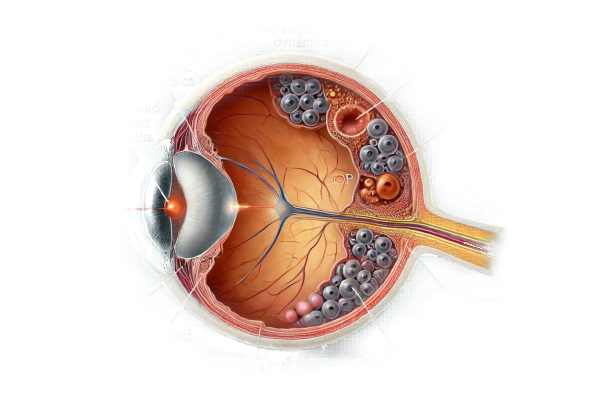
Glaucoma associated with ocular tumors is a secondary form of glaucoma caused by an intraocular tumor. These tumors can directly or indirectly raise intraocular pressure (IOP), resulting in glaucomatous optic neuropathy. This condition is especially difficult because it requires treating both the underlying tumor and the resulting glaucoma. Understanding the pathophysiology, clinical presentation, and diagnostic challenges is critical for effective disease management and vision preservation.
Clinical Features of Tumor-Related Glaucoma
Glaucoma caused by ocular tumors is a complex condition that develops when an intraocular tumor disrupts normal aqueous humor dynamics, resulting in increased intraocular pressure (IOP) and optic nerve damage. The relationship between ocular tumors and glaucoma is complex, with different mechanisms depending on the tumor’s location, size, and type.
Pathophysiology
The pathophysiology of glaucoma associated with ocular tumors includes several mechanisms:
- Direct Obstruction: Tumors inside the eye can physically block the aqueous humor outflow pathways. Tumors in the anterior segment, for example, can block the trabecular meshwork, preventing drainage and increasing IOP.
- Secondary Angle Closure: Tumors can cause secondary angle closure by pushing the iris forward, thereby narrowing or closing the angle between the iris and cornea. This mechanism is seen in ciliary body tumors and other anterior segment neoplasms.
- Neovascularization: Tumors can cause neovascularization, or the formation of abnormal blood vessels in the anterior segment. These vessels can obstruct the trabecular meshwork or form peripheral anterior synechiae, complicating aqueous outflow and raising IOP.
- Inflammation: Intraocular tumors can cause inflammatory responses, resulting in secondary uveitis. The resulting inflammatory cells and debris can clog the trabecular meshwork, exacerbating the IOP elevation.
- Pigment Dispersion: Certain tumors can cause pigment dispersion in the eye. The dispersed pigment may accumulate in the trabecular meshwork, obstructing aqueous humor drainage.
Types of Tumors
Several types of intraocular tumors can be linked to glaucoma:
- Uveal Melanoma is the most common primary intraocular tumor in adults. It can develop from the choroid, ciliary body, or iris, and depending on its size and location, it can cause secondary glaucoma via direct obstruction, angle closure, or neovascularization.
- Retinoblastoma: Retinoblastoma, which primarily affects children, can cause secondary glaucoma through mechanisms similar to uveal melanoma. Tumor-induced inflammation and neovascularization share common pathways.
- Metastatic Tumors: Tumors from other parts of the body, such as breast or lung cancer, can spread to the eye, resulting in secondary glaucoma. These tumors can cause angle closure or neovascularization, which complicates the clinical picture.
- Ciliary Body Tumors: Tumors that develop in the ciliary body can directly obstruct aqueous humor outflow or push the iris forward, resulting in secondary angle closure.
Clinical Presentation
Patients with glaucoma caused by ocular tumors may exhibit a variety of symptoms, depending on the tumor type, location, and extent. Common symptoms include:
- Elevated Intraocular Pressure: Persistent elevation of IOP despite standard glaucoma treatment is a reliable indicator of secondary glaucoma. This elevation can be acute or chronic, depending on how the tumor behaves.
- Visual Disturbances: Patients may experience blurred vision, visual field defects, or sudden vision loss, especially if the tumor affects the optic nerve or causes significant retinal detachments.
- Ocular Pain: Pain can be caused by increased intraocular pressure or tumor-related inflammation.
- Visible Mass: In some cases, a visible mass in the anterior segment may be present, especially with iris or ciliary body tumors.
- Red Eye: Tumors can cause chronic redness and inflammation, which can lead to uveitis or neovascularization.
Diagnostic Challenges
Diagnosing glaucoma associated with ocular tumours poses several challenges:
- Atypical Presentation: An intraocular tumor can cause an atypical presentation of glaucoma. Standard glaucoma treatments may not effectively control IOP, necessitating further investigation.
- Detection of Tumor: Recognizing the presence of an intraocular tumor necessitates a high level of suspicion, particularly in patients with refractory glaucoma. Detailed ocular examinations and imaging studies are required.
- Differential Diagnosis: Differentiating glaucoma caused by ocular tumors from other types of secondary glaucoma, such as neovascular or inflammatory glaucoma, necessitates careful consideration of clinical and imaging findings.
Methods to Diagnose Tumor-Linked Glaucoma
Glaucoma associated with ocular tumors is diagnosed using a combination of clinical examinations, imaging studies, and specialized tests. Here are the main diagnostic methods used:
Clinical Examination
- Comprehensive Eye Exam: A complete eye examination is required, including IOP measurement, slit-lamp biomicroscopy, and gonioscopy. These tests aid in detecting abnormalities in the anterior segment, angle structure, and the presence of a tumor.
- Dilated Fundus Examination: A thorough examination of the retina and optic nerve is necessary. This examination may reveal signs of retinal detachment, optic nerve involvement, and other fundus changes associated with intraocular tumor.
Imaging Studies
- Ultrasound Biomicroscopy (UBM): UBM captures high-resolution images of the anterior segment structures, such as the iris, ciliary body, and anterior chamber angle. It is especially useful for detecting small tumors and determining their effects on aqueous humor dynamics.
- Optical Coherence Tomography (OCT): OCT is useful in imaging the retina and optic nerve head. It can aid in detecting retinal detachment, optic nerve changes, and other posterior segment abnormalities associated with intraocular tumors.
- B-Scan Ultrasonography: This imaging modality is useful for assessing the size and extent of larger intraocular tumors. B-scan ultrasonography detects tumor size, shape, and involvement of nearby structures.
- Fluorescein Angiography: Fluorescein angiography evaluates the retinal and choroidal vasculature. It is especially useful in detecting neovascularization and other vascular changes caused by intraocular tumors.
Specialized Tests
- Fine Needle Aspiration Biopsy (FNAB): When the diagnosis is uncertain, FNAB can be used to collect a tissue sample for histopathological examination. This procedure helps to confirm the tumor type and guide subsequent treatment.
- Magnetic Resonance Imaging (MRI): MRI produces detailed images of the orbit and brain, which aids in the detection of intraocular and orbital tumors, as well as any associated systemic involvement.
- Computed Tomography (CT): CT scans are useful for detecting calcifications within intraocular tumors, which can be associated with certain tumor types such as retinoblastoma.
Management Options for Tumor-Linked Glaucoma
The treatment of glaucoma caused by ocular tumors requires a multifaceted approach that addresses both the underlying tumor and the resulting glaucoma. Here are the conventional and emerging treatment options:
- Medications: Medication is frequently used as the first line of treatment to reduce intraocular pressure (IOP). This includes:
- Prostaglandin Analogs: Promotes uveoscleral outflow.
- Beta-blockers: Reduces aqueous humor production.
- Alpha Agonists: Both reduce production and increase outflow.
- Carbonic Anhydrase Inhibitors: Reduces aqueous humor production.
- Rho Kinase Inhibitors: Enhances trabecular outflow.
- Laser Therapy: Laser treatments can help manage IOP:
- Laser Trabeculoplasty: Improves outflow from the trabecular meshwork.
- Cyclophotocoagulation: Reduces aqueous humor production by focusing on the ciliary body.
- Surgical Interventions: If medications and laser therapy are insufficient, surgery may be required:
- Trabeculectomy: Opens a new drainage pathway for aqueous humor.
- Glaucoma Drainage Devices: Implants such as the Ahmed or Baerveldt implants aid in aqueous humor drainage.
- Goniotomy and Trabeculotomy: Procedures for improving aqueous outflow, particularly in cases of angle closure.
Tumor-Specific Treatments
- Radiotherapy: For malignant tumors like uveal melanoma, plaque brachytherapy or external beam radiotherapy can be used to control the tumor and reduce its effect on IOP.
- Surgical Excision: The tumor is completely or partially removed, depending on its size, location, and type. Enucleation (eye removal) may be necessary in severe cases.
- Chemotherapy: Used to treat systemic cancers that have spread to the eye, such as retinoblastoma.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): New techniques for fewer complications and faster recovery:
- iStent and Hydrus Microstent: Tiny devices used to improve trabecular outflow.
- Xen Gel Stent: Opens a new drainage pathway with minimal tissue disruption.
- Gene Therapy: Researchers are looking into therapies that can target genetic factors that cause glaucoma and tumor growth.
- Neuroprotection: New treatments seek to protect the optic nerve from damage. These include pharmacological agents and novel therapies that promote retinal ganglion cell health.
- Regenerative Medicine: Techniques like stem cell therapy are being studied for their ability to repair or replace damaged ocular tissues.
Effective treatment of glaucoma caused by ocular tumours necessitates a personalized approach that takes into account the specific type and characteristics of the tumour, the severity of the glaucoma, and the patient’s overall health.
Preventing Tumor-Related Glaucoma
- Regular Eye Exams: Have comprehensive eye exams to detect any early signs of ocular tumors and associated glaucoma. Early detection is critical to effective management.
- Monitor Systemic Health: Treat systemic conditions like hypertension, diabetes, and cancer, which can all lead to ocular complications.
- Protective Eyewear: Wear protective eyewear in environments where there is a risk of eye injury or exposure to hazardous substances.
- Family History Awareness: Be aware of your family’s history with ocular tumors and glaucoma. Genetic predispositions can heighten risk.
- Healthy Lifestyle: Lead a healthy lifestyle by eating a well-balanced diet, exercising regularly, and refraining from smoking and drinking excessively.
- UV Exposure Avoidance: Wear UV-blocking sunglasses to protect your eyes from excessive ultraviolet (UV) light.
- Prompt Treatment of Eye Conditions: If you experience persistent redness, pain, or vision changes, seek medical attention right away.
- Educate Yourself: Be aware of the symptoms and risk factors for ocular tumors and glaucoma. Early detection can lead to timely medical treatment.
- Genetic Counseling: Those with a family history of ocular tumors should seek genetic counseling to better understand the risks and preventive measures.
Individuals who follow these preventive measures can significantly reduce their risk of developing glaucoma caused by ocular tumors while also maintaining good ocular health.
Trusted Resources
Books
- “Ocular Tumors: Diagnosis and Treatment” by Jerry A. Shields and Carol L. Shields
- “Clinical Ophthalmic Oncology: Uveal Tumors” by Arun D. Singh
- “Intraocular Tumors: An Atlas and Textbook” by Jerry A. Shields and Carol L. Shields






