What is Globe Rupture?
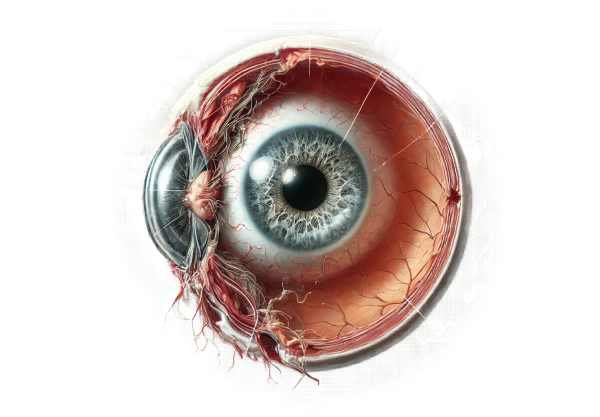
Globe rupture is a severe ocular condition in which the integrity of the eye’s outer membranes, including the sclera and cornea, is compromised due to trauma. This injury causes the extrusion of intraocular contents, which can result in significant vision loss or even blindness if not treated promptly. Globe rupture is classified as an ophthalmic emergency, necessitating immediate medical attention to preserve eye function and avoid further complications. The condition can be caused by either blunt or penetrating trauma and is frequently associated with other ocular and orbital injuries.
Comprehensive Examination of Globe Rupture
Globe rupture is a catastrophic event with serious consequences for vision and overall ocular health. Understanding the nature of this injury, including its causes, clinical features, and potential complications, is critical for timely and effective treatment.
Pathophysiology
Globe rupture occurs when a forceful impact on the eye exceeds the tensile strength of the sclera or cornea, resulting in a breach in these protective layers. This breach may cause intraocular fluid leakage and ocular tissue extrusion. The pathophysiology may differ depending on the type and severity of the trauma:
- Blunt Trauma: High-velocity impacts, such as sports injuries, car accidents, or physical assaults, can result in a sudden increase in intraocular pressure. This pressure spike can cause the globe to rupture at its weakest points, which are usually near the limbus or the insertion of the extraocular muscles.
- Penetrating Trauma: Sharp objects, such as knives or shrapnel, can directly penetrate the sclera or cornea. These injuries can cause localized or extensive damage, depending on the object’s size, shape, and velocity.
- Perforating Trauma: In more severe cases, an object can enter and exit the eye, resulting in two or more rupture sites. This type of injury is frequently associated with high-energy impacts and poses a high risk of serious complications.
Clinical Presentation
The clinical presentation of a globe rupture can vary greatly depending on the nature and severity of the injury. The key signs and symptoms include:
- Severe Pain: Patients usually experience intense ocular pain right after the injury. This pain is frequently aggravated by movements or attempts to open the eye.
- Visual Disturbances: The degree of vision loss varies depending on the severity of the injury. Patients may report blurred vision, double vision, or total blindness in the affected eye.
- Extrusion of Intraocular Contents: Globe rupture is characterized by the prolapse of ocular tissues such as the iris or vitreous humor through the rupture site. This extrusion is frequently visible upon inspection.
- Hyphema: Blood accumulation in the anterior chamber of the eye is common in globe rupture cases, resulting in a visible reddish tint in the affected eye.
- Corneal or Scleral Lacerations: Visible cuts or tears in the cornea or sclera are clear signs of globe rupture. These lacerations may be accompanied by subconjunctival hemorrhage, in which blood accumulates beneath the conjunctiva.
- Decreased Intraocular Pressure: Due to intraocular fluid leakage, the affected eye may feel softer when palpated than the uninjured eye.
Complications
Globe rupture can cause a variety of complications, some of which are immediate and others that develop over time:
- Infection: Bacteria or other pathogens can enter the eye through the rupture site, causing endophthalmitis, a serious and potentially blinding infection.
- Sympathetic Ophthalmia: This rare autoimmune condition develops when trauma to one eye causes an inflammatory response in the uninjured eye, potentially resulting in bilateral vision loss.
- Retinal Detachment: The force of the trauma can cause the retina to detach from the underlying tissue, resulting in significant vision impairment if not treated immediately.
- Cataract Formation: Trauma can cause cataract formation, resulting in lens clouding and vision impairment.
- Optic Nerve Damage: Severe trauma can injure the optic nerve, causing permanent vision loss.
Risk Factors
Certain factors can raise the risk of a globe rupture.
- Occupational Hazards: Workers in construction, manufacturing, and other high-risk environments are more likely to sustain ocular trauma.
- Involvement in High-Risk Sports: Activities like boxing, martial arts, and contact sports raise the risk of eye injuries.
- Previous Ocular Surgery: Eyes that have had previous surgical procedures, such as LASIK or cataract surgery, may be more prone to rupture.
- Age: Elderly people may have weaker scleral tissue, which raises the risk of rupture during trauma.
Understanding the pathophysiology, clinical presentation, and potential complications of globe rupture is critical for healthcare providers. This knowledge allows for timely diagnosis and appropriate intervention, which are critical for maintaining vision and preventing further damage.
Evaluating Globe Rupture
Globe rupture is diagnosed using a combination of clinical evaluation, imaging studies, and, in some cases, laboratory tests. Prompt and accurate diagnosis is critical for initiating treatment and improving results.
Clinical Evaluation
- History & Physical Examination: A detailed history of the injury, including the cause, timing, and any immediate symptoms, is required. The physical examination focuses on evaluating visual acuity, looking for visible lacerations, prolapsed tissues, and signs of hyphema or subconjunctival hemorrhage.
- Seidel Test: Fluorescein dye is applied to the ocular surface and examined using cobalt blue light. A positive Seidel test, in which the dye streams away from the rupture site, indicates the presence of aqueous humor leakage.
- Intraocular Pressure Measurement: While measuring IOP is usually part of an eye examination, it should be done with caution in cases of suspected globe rupture to avoid exacerbating the injury. A lower IOP compared to the uninjured eye can be a diagnostic indicator.
Imaging Studies
- Computed Tomography (CT) Scan: A CT scan of the orbit is considered the gold standard for diagnosing globe rupture. It provides detailed images of the eye and surrounding structures, assisting in determining the rupture site, the extent of the injury, and the presence of any foreign bodies.
- B-Scan Ultrasonography: When a CT scan is not immediately available, B-scan ultrasonography can be used to assess the globe’s integrity and detect intraocular foreign bodies or retinal detachments. However, its application is restricted if there is significant ocular surface disruption.
- Magnetic Resonance Imaging (MRI): MRI is generally not the first choice due to its longer acquisition time and sensitivity to metal, which may be present in penetrating injuries. However, it can be useful in certain situations to assess soft tissue damage.
Lab Tests
- Cultures and Sensitivity Testing: If there is a suspicion of infection, especially in penetrating injuries, cultures taken from the wound site can help guide antibiotic therapy.
- Blood Tests: Although not directly diagnostic of globe rupture, blood tests may be required to assess overall patient health, particularly in polytrauma cases or when surgical intervention is planned.
Treatment.
Treatment for globe rupture is an urgent medical need that necessitates a multifaceted approach to preserve vision and avoid complications. Immediate intervention usually includes stabilization, surgical repair, and comprehensive post-operative care.
Initial Management
- Stabilization: The first step is to stabilize the patient, particularly if other systemic injuries are present. Keep the patient calm and avoid putting any pressure on the eye.
- Shielding the Eye: Put a protective shield over the injured eye to prevent further damage. Avoid applying any pressure to the globe, including direct application of eye patches.
- Pain and Infection Control: Use systemic analgesics to alleviate pain and broad-spectrum intravenous antibiotics to avoid infection.
Surgical Intervention
- Primary Repair: The surgery to repair the globe rupture should be performed as soon as possible, preferably within 24 hours. The objectives are to close the wound, restore structural integrity to the eye, and preserve as much vision as possible. This involves suturing the scleral or corneal lacerations.
- Removing any foreign bodies while limiting further trauma to the eye.
- Addressing any prolapsed intraocular contents and repositioning them as needed.
- Vitrectomy: In severe cases with significant intraocular hemorrhage or retinal detachment, a pars plana vitrectomy may be required. This procedure removes the vitreous humor to clear any blood and debris, allowing access to repair retinal detachments.
- Lens Removal: If the lens is damaged, a lensectomy may be required, with or without additional intraocular lens implantation.
Post-operative Care
- Medication: Topical and systemic antibiotics are commonly used in post-operative care to prevent infection, corticosteroids to reduce inflammation, and IOP medications.
- Close Monitoring: Regular follow-up appointments are required to monitor the healing process, assess visual recovery, and detect complications such as infection, retinal detachment, or glaucoma.
- Rehabilitation: Vision rehabilitation services may be required to help patients adjust to any permanent vision loss.
Innovative and Emerging Therapies
- Tissue Engineering: Research into bioengineered ocular tissues offers hope for better results in globe rupture repair. This includes creating artificial corneas and scleral grafts that can integrate with natural tissues.
- Stem Cell Therapy: Experimental treatments utilizing stem cells aim to regenerate damaged ocular tissues, potentially improving recovery in severe globe rupture cases.
- Advanced Imaging Techniques: Imaging innovations such as high-resolution OCT improve the ability to assess and plan surgical repairs, resulting in more precise and effective interventions.
- Gene Therapy: While still in its early stages, gene therapy shows promise for treating underlying conditions that predispose people to severe ocular injuries, potentially improving long-term outcomes.
Effective treatment of globe rupture entails prompt surgical intervention, comprehensive post-operative care, and ongoing research into advanced therapies to improve patient outcomes.
Best Practices to Prevent Globe Rupture
- Use Protective Eyewear: Always wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports, construction work, or handling hazardous materials.
- Follow Safety Protocols: Follow workplace safety guidelines, particularly in environments where there is a high risk of ocular trauma. This includes wearing face shields, helmets, and other protective equipment.
- Education and Training: Educate employees and athletes about the importance of eye protection and proper safety precautions to avoid eye injuries.
- Secure Living Environment: Make sure your home environment is safe, especially for children and the elderly. This includes securing sharp objects and providing adequate lighting to avoid falls and accidents.
- Avoid High-Risk Behaviors: Avoid high-risk activities that do not provide adequate protection, such as handling fireworks, DIY projects without safety glasses, and reckless driving.
- Regular Eye Exams: Regular comprehensive eye exams can aid in the detection and management of conditions that weaken the eye structure, making it more prone to rupture.
- Immediate Attention to Eye Injuries: Seek immediate medical attention for any eye injury, no matter how minor it appears, to avoid complications that could lead to globe rupture.
- Maintain Overall Health: Control systemic conditions such as diabetes and hypertension, which can impair ocular health and increase the risk of eye injury.
- Use Safety Equipment Properly: Ensure that safety equipment is used correctly and consistently, with proper fit to provide the best protection.
- Promote Safe Sports Practices: Encourage athletes to wear appropriate protective gear and educate them on the risks of eye injuries.
Individuals who follow these preventive measures can significantly reduce their risk of globe rupture while also maintaining good ocular health.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “Trauma and Emergency Care for the Ophthalmologist” by Brian C. Joondeph and William B. Trattler
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn






