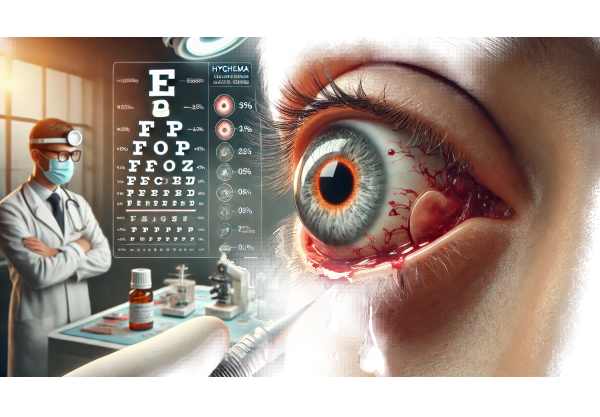
What is hyphema?
Hyphema is an ocular condition characterized by the presence of blood in the anterior chamber of the eye, which is located between the cornea and the iris. Trauma to the eye is a common cause of this condition, which results in bleeding from blood vessels in the iris or ciliary body. Hyphema can range from a small amount of blood that has little effect on vision to a severe accumulation that causes significant visual impairment and increases intraocular pressure. Prompt diagnosis and appropriate management are critical for avoiding complications and maintaining vision.
In-Depth Look at Hyphema
Hyphema requires immediate medical attention because it has the potential to cause significant ocular morbidity. Understanding the underlying mechanisms, risk factors, symptoms, and complications of hyphema is critical for proper diagnosis and treatment.
Pathophysiology
Hyphema occurs when blood vessels in the eye, particularly those in the iris or ciliary body, rupture and leak into the anterior chamber. This can result from a variety of mechanisms:
- Trauma: The most common cause of hyphema is eye trauma, which can be blunt or penetrating. Such injuries can damage the blood vessels in the anterior segment, causing bleeding.
- Surgical Complications: Intraocular surgeries, such as cataract extraction and glaucoma procedures, can occasionally cause hyphema due to unintentional injury to the blood vessels.
- Neovascularization: Conditions such as diabetic retinopathy or retinal vein occlusion can result in abnormal blood vessel growth that is prone to bleeding.
- Blood Dyscrasias: Patients with bleeding disorders or those taking anticoagulants are at a higher risk of spontaneous hyphema.
Classification
Hyphema is usually classified based on the amount of blood in the anterior chamber:
- Microhyphema: Red blood cells suspended in aqueous humor that do not form a visible layer.
- Grade 1: Blood takes up less than one-third of the anterior chamber.
- Grade 2: Blood is present in one-third to one-half of the anterior chamber.
- Grade 3: Blood fills half or less of the anterior chamber.
- Grade 4: Total hyphema, also known as “eight-ball hyphema,” in which the anterior chamber is completely filled with blood.
Symptoms
The presentation of hyphema varies according to the severity of the bleeding. Common symptoms include:
- Visual Impairment: Reduced visual acuity is the primary symptom, with the degree of vision loss proportional to the amount of blood in the anterior chamber.
- Pain: High intraocular pressure can cause severe pain and discomfort.
- Photophobia: Hypersensitivity to light is frequently associated with hyphema.
- Red Eye: The presence of visible blood in the anterior chamber causes the eye to appear red.
Complications
Hyphema can cause a number of serious complications, particularly if not treated promptly:
- Increased Intraocular Pressure (IOP): Blood in the anterior chamber can clog the trabecular meshwork, preventing aqueous humor outflow and increasing IOP. Persistent elevation can lead to glaucoma and optic nerve damage.
- Rebleeding: Secondary hemorrhage can occur within a few days of the initial bleed, and it is often more severe and more likely to cause complications.
- Corneal Blood Staining: Prolonged contact of blood with the corneal endothelium can cause staining, which can result in permanent vision loss.
- Optic Atrophy: High IOP and recurrent bleeding can cause optic nerve damage and atrophy, resulting in permanent vision loss.
Risk Factors
Several factors can raise the risk of developing hyphema:
- Trauma: Engaging in high-risk activities or contact sports increases the likelihood of eye injuries.
- Previous Ocular Surgery: Patients who have had eye surgery before are more likely to develop hyphema.
- Medical Conditions: People with hemophilia, von Willebrand disease, and other clotting disorders are more likely to experience bleeding episodes.
- Medications: Taking anticoagulants (such as warfarin or aspirin) can increase the risk of bleeding.
Differential Diagnosis
It is critical to distinguish hyphema from other conditions that may present with similar symptoms.
- Subconjunctival Hemorrhage: This condition causes bleeding on the surface of the eye, beneath the conjunctiva, but does not affect the anterior chamber.
- Uveitis: Inflammation of the uveal tract can cause redness, pain, and visual disturbances, but it usually does not result in visible blood in the anterior chamber.
- Corneal Abrasion: Corneal abrasions, while painful and associated with vision impairment, do not result in blood in the anterior chamber.
Prognosis
The severity of the initial injury, the presence of complications, and the promptness of treatment all influence the prognosis for hyphema. Minor hyphemas (Grade 1 and microhyphema) usually resolve with conservative treatment, whereas more severe cases (Grade 3 and 4) necessitate close monitoring and intervention to avoid long-term damage.
Hyphema Diagnostic Techniques
A thorough clinical evaluation and a battery of diagnostic tests to determine the extent of the bleeding and its impact on ocular structures are required to make a hyphema diagnosis. Here are the main diagnostic methods used:
Comprehensive Eye Examination
A thorough eye examination by an ophthalmologist is essential for diagnosing hyphema. This includes:
- Visual Acuity Test: Measuring vision clarity can help determine how the hyphema affects visual function.
- Slit-Lamp Examination: This allows the doctor to examine the anterior chamber thoroughly, determining the presence and extent of blood. The slit lamp can also help diagnose any cornea, iris, or lens injuries.
- Intraocular Pressure Measurement: Checking the intraocular pressure is critical because high IOP can indicate potential complications such as glaucoma. This is usually done with a tonometer.
Gonioscopy
Gonioscopy is a procedure that uses a special lens to view the angle between the iris and the cornea. This examination determines whether blood is blocking the trabecular meshwork, which drains aqueous humor from the eye. Assessing the angle is critical for managing high intraocular pressure.
Ultrasound Biomicroscopy (UBM)
UBM can produce high-resolution images of the anterior segment structures. This imaging technique is especially useful when blood obscures the view of the anterior chamber. UBM aids in determining the extent of the bleeding and detecting any associated structural damage that would not be visible with a standard slit-lamp examination.
Anterior Segment Optical Coherence Tomography (AS-OCT)
AS-OCT is a noninvasive imaging technique that generates cross-sectional images of the anterior segment. It aids in the visualization of blood in the anterior chamber as well as the assessment of its impact on adjacent structures such as the cornea and iris. AS-OCT is useful for tracking the resolution of hyphema over time.
Fundus Examination
A thorough examination of the retina and optic nerve is carried out to detect any additional injuries or complications. This is possible with indirect ophthalmoscopy, which allows for a wide-field view of the retina. It is critical that the trauma or bleeding does not affect the posterior segment of the eye.
Blood Tests
Blood tests may be required in patients with known bleeding disorders or when hyphema occurs spontaneously. These tests include:
- Complete Blood Count (CBC): To assess overall health and identify any underlying conditions that could cause bleeding.
- Coagulation Profile: This includes prothrombin time (PT), activated partial thromboplastin time (aPTT), and international normalized ratio (INR) to assess clotting function.
- Screening for Systemic Diseases: Looks for conditions like diabetes or hypertension that could lead to hyphema.
Hyphema Treatment Options
The treatment of hyphema aims to lower intraocular pressure, prevent rebleeding, and preserve vision. Here are the standard treatment options together with innovative and emerging therapies:
Standard Treatment Options:
- Medical Management: – Bed Rest and Head Elevation: Patients should rest in bed with their head elevated to allow blood to settle and reabsorb. This position reduces intraocular pressure.
- Eye Shield: Wearing a protective eye shield can help prevent further injury and promote healing.
- Medicines:
- Topical Steroids: Used to reduce inflammation and prevent synechiae (iris adhesion to the lens or cornea).
- Cycloplegics: To relieve pain by paralyzing the ciliary muscle and immobilizing the iris.
- Anti-glaucoma Medications: These include beta-blockers, alpha agonists, and carbonic anhydrase inhibitors, which reduce intraocular pressure.
- Surgical Intervention: – Anterior Chamber Washout: This procedure is performed when a large hyphema does not resolve with medical management or if there is a persistent elevation of intraocular pressure. It entails irrigating and aspirating blood from the anterior chamber.
- Paracentesis: A procedure that drains a small amount of aqueous humor from the anterior chamber to lower intraocular pressure and relieve pain.
- Monitoring and Follow-Up: Regular follow-up appointments are required to monitor intraocular pressure and ensure that the hyphema heals without complications. This includes regular check-ups to evaluate the eye’s condition and adjust treatment as necessary.
Innovative and Emerging Therapies
- Anti-fibrinolytic Agents: These medications, such as aminocaproic acid, can help prevent rebleeding by inhibiting the breakdown of clots in the anterior chamber. They are particularly effective in treating traumatic hyphema.
- Gene Therapy: Although still in the experimental stages, gene therapy shows promise for treating underlying conditions that predispose people to hyphema. Targeting specific genetic pathways may be able to reduce the risk of bleeding in susceptible patients.
- Minimally Invasive Surgical Techniques: Advances in surgical technology, such as micro-incisional surgery, have enabled more precise and minimally invasive hyphema management procedures. These techniques can shorten the recovery time and lower the risk of complications.
- Laser Therapy: Laser treatments are being investigated as a method of lowering intraocular pressure and treating related ocular conditions. Lasers can target and seal leaking blood vessels, lowering the risk of rebleeding.
By combining these treatment options, healthcare providers can develop a comprehensive plan to effectively manage hyphema, resulting in the best possible outcomes for patients.
Best Practices for Avoiding Hyphema
- Wear Protective Eyewear: Wear protective eyewear when participating in sports, working, or engaging in activities that could result in eye injury. This can greatly reduce the likelihood of trauma-induced hyphema.
- Manage Chronic Conditions: Maintain control of chronic conditions like diabetes and hypertension by visiting the doctor on a regular basis and following the treatment plan. Well-managed systemic conditions can lower the likelihood of ocular complications.
- Avoid Blood Thinners: If you are at risk for hyphema, limit your use of blood thinners. Before taking any anticoagulant medication, consult with your doctor.
- Regular Eye Exams: Have regular eye exams to detect and manage any underlying conditions that could increase the risk of hyphema, such as neovascularization or high intraocular pressure.
- Control Blood Sugar Levels: Maintaining stable blood sugar levels can help diabetic patients avoid diabetic retinopathy and associated neovascularization, lowering their risk of hyphema.
- Avoid Contact Sports: If you have a history of hyphema or other eye problems, you should avoid high-risk contact sports. Engage in activities that reduce the risk of eye injury.
- Educate Yourself: Discover the symptoms and risks of hyphema. Early detection and treatment can help prevent complications.
- Use Eye Shields Post-Surgery: Following any eye surgery, consult your surgeon about the use of eye shields to protect your eyes during the recovery period.
- Stay Hydrated and Healthy: Maintaining overall health through a well-balanced diet and adequate hydration can benefit eye health and lower the risk of complications.
- Monitor Medications: If you take blood clotting medications, discuss their effects with your doctor on a regular basis to avoid excessive bleeding risks.
Individuals who follow these preventive measures can reduce their risk of developing hyphema while also maintaining good overall eye health.
Trusted Resources
Books
- “Ophthalmology” by Myron Yanoff and Jay S. Duker
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Nika Bagheri, Brynn Wajda, and others
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling










