What is Juvenile Idiopathic Arthritis-Related Eye Disorder?
Juvenile idiopathic arthritis-related eye disease (JIA-associated uveitis) is an inflammatory condition that affects the eyes of children suffering from juvenile idiopathic arthritis. If not diagnosed and treated promptly, this ocular disease can cause serious complications, including vision loss. It primarily manifests as chronic anterior uveitis, which is defined by inflammation of the uvea, the eye’s middle layer. Regular monitoring and early intervention are required to effectively manage this condition.
Detailed Investigation of Juvenile Idiopathic Arthritis-Related Eye Disease
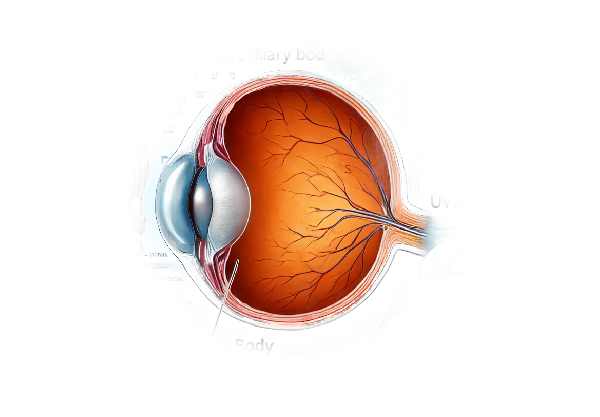
Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in children, and it is frequently associated with vision problems, particularly uveitis. Uveitis is an inflammation of the uveal tract, which includes the iris, ciliary body, and choroid. Uveitis in JIA is typically characterized by chronic anterior uveitis, which affects the front part of the eye.
Epidemiology and Risk Factors
JIA affects roughly one in every 1,000 children, with uveitis developing in 10-20% of these cases. Certain JIA subtypes, particularly oligoarticular JIA, and children who test positive for antinuclear antibodies (ANA) are more likely to develop uveitis. Girls are more commonly affected than boys, and uveitis usually appears within the first few years of arthritis diagnosis.
Pathophysiology
The exact mechanisms that cause JIA-associated uveitis are unknown, but they involve an autoimmune response in which the body’s immune system attacks its own tissues. In JIA, the autoimmune response attacks the joints and, in the case of uveitis, the uveal tract of the eyes. If left untreated, this inflammation can damage various structures within the eye, resulting in complications.
Clinical Presentation
Children with JIA-associated uveitis may be asymptomatic, particularly in the early stages, emphasizing the importance of regular eye screenings. When symptoms appear, they may include:
- Redness of the Eye: Persistent redness without pain may indicate underlying uveitis.
- Eye Pain: Eye pain is less common in children than in adults, but it can occur, especially if the inflammation is severe.
- Photophobia: One of the most common symptoms is sensitivity to light.
- Blurred Vision: Inflammation can reduce vision clarity, causing blurred vision.
- Floaters are dark spots that appear to float across the visual field as a result of inflammatory debris in the vitreous humor.
Complications
Without proper treatment, JIA-associated uveitis can result in several serious complications:
- Cataracts: Inflammation or prolonged use of corticosteroids to treat it can cause clouding of the lens.
- Glaucoma: Increased intraocular pressure can result from inflammation or treatment, causing optic nerve damage.
- Band Keratopathy: Calcium deposits on the cornea can form, causing visual impairment.
- Synechiae: These are adhesions between the iris and the lens or cornea that can cause pupil irregularities and block aqueous humor flow, potentially leading to glaucoma.
- Cystoid Macular Edema: Swelling in the macula, or central part of the retina, can result in significant vision loss.
Differential Diagnosis
Other conditions can resemble JIA-associated uveitis, necessitating differential diagnosis. This includes:
- Infectious Uveitis: Caused by bacterial, viral, or fungal infections, and frequently accompanied by systemic symptoms.
- Other Autoimmune Diseases: Sarcoidosis and Behçet’s disease can both cause uveitis.
- Trauma: Eye injuries can cause inflammation that resembles uveitis.
Prognosis
The prognosis for children with JIA-associated uveitis is dependent on the timing and efficacy of treatment. Many children can keep their vision healthy with early detection and proper management. However, delayed or inadequate treatment of inflammation can cause permanent vision damage.
Methods to Diagnose JIA Eye Issues
Diagnosing JIA-associated uveitis requires a multifaceted approach that includes regular screenings, clinical evaluations, and specialized tests.
Regular Screening
Children with JIA should have regular ophthalmologic examinations, as early uveitis can be asymptomatic. The frequency of screenings varies depending on the subtype of JIA and the presence of risk factors such as ANA positivity. Eye exams are typically recommended every 3 to 6 months for high-risk children and once a year for those at low risk.
Clinical Evaluation
- Slit-Lamp Examination: This is the primary method of diagnosing uveitis. A slit lamp allows for a detailed examination of the anterior segment of the eye, which aids in the identification of inflammation markers such as cell and flare in the anterior chamber, keratic precipitates, and iris nodules.
- Visual Acuity Test: Measuring visual acuity can aid in determining the effect of uveitis on vision. Any reduction in visual clarity may warrant further investigation.
- Tonometry: Measuring intraocular pressure is critical because uveitis and its treatments can progress to glaucoma. To avoid optic nerve damage, elevated intraocular pressure must be treated promptly.
Imaging and Diagnostic Tests
- Optical Coherence Tomography (OCT) is a non-invasive imaging technique that produces detailed cross-sectional images of the retina and optic nerve. It can detect and monitor complications like cystoid macular edema and changes in the optic nerve.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream to see how blood flows in the retina and choroid. It aids in the identification of leakage and inflammation that would otherwise go undetected during a routine examination.
- Ultrasound Biomicroscopy: When visualization of the posterior segment is difficult due to media opacities such as cataracts or dense vitreous inflammation, ultrasound biomicroscopy can aid in assessing the ciliary body and pars plana.
Lab Tests
Laboratory tests can help with diagnosis by identifying underlying causes and associated conditions.
- Antinuclear Antibody (ANA) Test: ANA positivity is a risk factor for uveitis in JIA and can help determine the frequency of eye screenings.
- Complete Blood Count (CBC): This test detects signs of systemic inflammation or infection.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): Elevated levels suggest systemic inflammation, which supports the diagnosis of active JIA.
Juvenile Idiopathic Arthritis and Eye Disease Treatment
The treatment of juvenile idiopathic arthritis (JIA)-related eye disease focuses on reducing inflammation, preventing complications, and preserving vision. Treatment options vary depending on the severity and duration of uveitis.
Medical Management
- Corticosteroids are the first-line treatment for acute uveitis.
- Topical Corticosteroids: Eye drops containing prednisolone or dexamethasone are commonly used to reduce inflammation.
- Periocular or Systemic Corticosteroids: In more severe cases, periocular injections or oral corticosteroids may be required to reduce inflammation.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications can help manage minor inflammation and are sometimes used in conjunction with corticosteroids.
- Immunomodulatory Therapy: Immunomodulatory drugs are frequently required for patients with chronic or recurring uveitis who do not respond well to corticosteroids.
- Methotrexate: A common disease-modifying antirheumatic drug (DMARD) that reduces the need for corticosteroids by controlling systemic inflammation.
- Another DMARD: In cases where methotrexate is insufficient or not tolerated, sulfasalazine or leflunomide may be used instead.
- Biologic Agents: Advances in biologic therapies have created new treatment options for refractory uveitis.
- Tumor Necrosis Factor (TNF) Inhibitors: Adalimumab and infliximab have been shown to effectively treat severe uveitis associated with JIA.
- Interleukin-6 (IL-6) Inhibitors: Tocilizumab is another biologic that can help treat JIA-related uveitis.
- Other Biologics: Agents that target different pathways, such as abatacept (a T-cell co-stimulation inhibitor), should also be considered.
- Antibiotics and antivirals: When infectious agents are suspected or confirmed, appropriate antimicrobial therapy is required to treat the underlying infection and reduce ocular inflammation.
Surgical Interventions
Surgical options are considered for treating uveitis complications such as cataracts, glaucoma, and band keratopathy.
- Cataract Surgery: Phacoemulsification with intraocular lens implantation is frequently required in children who develop significant lens opacities as a result of chronic inflammation or steroid use.
- Glaucoma Surgery: Trabeculectomy or the implantation of glaucoma drainage devices may be required to control intraocular pressure.
- Keratoprosthesis: In cases of severe corneal damage, a corneal transplant or artificial cornea (keratoprosthesis) may be necessary.
Innovative and Emerging Therapies
- Biologic Therapies: Ongoing research into biologic agents is expanding the options for targeted therapy, thereby improving outcomes for children with refractory uveitis.
- Gene Therapy: New research is looking into the potential of gene therapy to treat underlying genetic factors that contribute to JIA and associated uveitis.
- Stem Cell Therapy: Research into stem cell therapy raises the prospect of regenerative treatments that can repair damaged ocular tissues and restore vision.
Multidisciplinary Approach
To provide comprehensive care for JIA-related eye disease, a multidisciplinary team of pediatric rheumatologists, ophthalmologists, and other specialists is frequently required. Regular follow-ups and coordinated care plans are critical for monitoring disease activity, adjusting treatments, and responding quickly to complications.
Effective Strategies for Improving and Avoiding Juvenile Idiopathic Arthritis-Related Eye Disease
- Regular Eye Exam: Ensure that children with JIA receive routine eye examinations as recommended by their healthcare provider. Early detection of uveitis is critical for avoiding complications.
- Medication Adherence: Consistently follow the prescribed treatment regimen. Skipping doses or discontinuing medication without seeking medical advice can result in flare-ups and complications.
- Monitor for Symptoms: Parents and caregivers should be on the lookout for signs of eye problems such as redness, pain, photophobia, or vision changes. Inform your healthcare provider as soon as possible if you experience such symptoms.
- Healthy Lifestyle: Promote a well-balanced diet, regular exercise, and enough sleep to improve overall health and reduce inflammation.
- Protective Eyewear: Wear protective eyewear during activities that could cause eye injuries, especially in active children.
- Avoid Infections: Maintain good hygiene to reduce the risk of infections that can worsen uveitis. Ensure that vaccinations are up to date, as recommended by your pediatrician.
- Stress Management: Teach children stress-reduction techniques, hobbies, and support groups. Stress can harm the immune system and worsen autoimmune conditions.
- Stay Informed: Educate yourself and your child about JIA and its potential complications, such as uveitis. Understanding the disease can help you manage it better.
- Regular Follow-Ups: Attend all scheduled appointments with your rheumatologist and ophthalmologist. Regular monitoring is critical for adjusting treatment and detecting early signs of complications.
- Communicate with Healthcare Providers: Keep open lines of communication with all members of the healthcare team. Please report any medication side effects or changes in symptoms to ensure the best possible care.
Trusted Resources
Books
- “Textbook of Pediatric Rheumatology” by James T. Cassidy, Ross E. Petty, Ronald M. Laxer, and Carol B. Lindsley
- “Ocular Inflammatory Disease and Uveitis Manual” by John J. Huang and Narsing A. Rao
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright and Peter H. Spiegel
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- American College of Rheumatology (ACR): www.rheumatology.org
- Arthritis Foundation: www.arthritis.org
- MedlinePlus: medlineplus.gov






