What is keratitis?
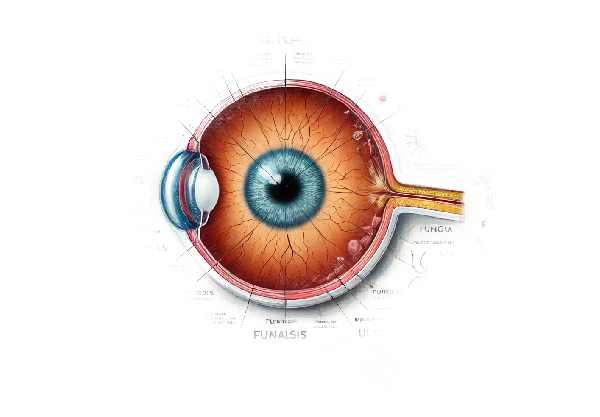
Keratitis is an inflammation of the cornea, the transparent, dome-shaped surface that covers the front of the eye. This condition can cause pain, redness, and vision problems, and if not treated, it can progress to severe complications, including vision loss. Infections (bacterial, viral, fungal, or parasitic), injuries, contact lens use, or other underlying health conditions can all cause keratitis. Early detection and treatment are critical to preventing long-term eye damage.
Detailed Investigation of Keratitis
Keratitis is a complex condition with numerous causes, symptoms, and complications. Understanding the various forms of keratitis and their underlying mechanisms is critical for accurate diagnosis and treatment.
Types of Keratitis
- Infectious Keratitis: Caused by microbial agents like bacteria, viruses, fungi, and parasites.
- Bacterial Keratitis: Bacteria such as Pseudomonas aeruginosa and Staphylococcus aureus are commonly associated with contact lens use. Poor contact lens hygiene, minor eye injuries, or underlying eye conditions can all cause it.
- Viral Keratitis: Herpes simplex virus (HSV) is the most common cause of viral keratitis, which can reoccur and leave significant corneal scars. Other viral agents include the varicella-zoster virus (VZV), which causes shingles.
- Fungal Keratitis: This type is less common and is typically caused by fungi like Fusarium, Aspergillus, or Candida. It frequently occurs following eye trauma involving organic material or in people with weakened immune systems.
- Parasitic Keratitis: Acanthamoeba keratitis is a rare but serious infection that affects contact lens wearers, particularly those who clean their lenses with tap water.
- Non-Infectious Keratitis: This type is caused by a variety of factors other than infections.
- Exposure Keratitis: Occurs when the cornea becomes exposed to air due to incomplete eyelid closure, which can occur during sleep or in conditions such as Bell’s palsy.
- Allergic Keratitis: Caused by allergic reactions, and is frequently associated with conditions such as atopic keratoconjunctivitis.
- Photokeratitis: Caused by UV light exposure, such as welding without proper eye protection or long-term exposure to sunlight.
Signs of Keratitis
The symptoms of keratitis differ depending on the cause and severity of the condition. Common symptoms include eye redness and swelling.
Pain or discomfort in the eye
Symptoms may include excessive tears or discharge, as well as blurred or decreased vision.
- Photophobia, or sensitivity to light
- A sensation of a foreign body in the eye.
Keratitis, in severe cases, can result in corneal ulcers, which are open sores on the cornea that cause significant pain and vision impairment.
Pathophysiology
Keratitis is characterized by inflammation and corneal tissue damage. In infectious keratitis, pathogens invade the cornea, triggering an immune response that results in inflammation and tissue damage. The pathogen’s virulence and the host’s immune response determine the severity of the inflammation and the extent of corneal damage.
Non-infectious keratitis has multiple mechanisms. For example, exposure keratitis occurs when the cornea dries out due to inadequate eyelid closure, causing inflammation and damage. Immune responses to allergens cause inflammation of the cornea and conjunctiva, which causes allergic keratitis. Photokeratitis occurs when UV radiation causes direct damage to the corneal epithelium, resulting in cell death and inflammation.
Risk Factors
Several risk factors may increase the likelihood of developing keratitis:
- Contact Lens Use: Improper use, poor hygiene, and prolonged use of contact lenses are all risk factors for infectious keratitis.
- Eye Trauma: Eye injuries, particularly those involving organic matter, can introduce keratitis-causing pathogens.
- Immune System Compromise: Conditions like HIV/AIDS, diabetes, and the use of immunosuppressive drugs can make you more susceptible to infection.
- Ocular Surface Diseases: Dry eye syndrome and blepharitis can weaken the corneal surface, increasing the risk of keratitis.
- Environmental Factors: Exposure to contaminated water, such as swimming in lakes or cleaning contact lenses with tap water, can cause keratitis, specifically Acanthamoeba keratitis.
Complications
Keratitis, if left untreated, can cause severe complications such as:
- Corneal Scarring: Permanent scarring can impair vision and necessitates surgical intervention, such as corneal transplant.
- Corneal Ulcers: Deep ulcers can cause severe pain, vision loss, and an increased risk of corneal perforation.
- Endophthalmitis: An infection that spreads inside the eye and can cause blindness if not treated promptly.
- Vision Loss: Severe or untreated keratitis can cause partial or complete loss of vision.
Epidemiology
Keratitis prevalence varies around the world, with higher rates seen in areas with widespread contact lens use and limited access to clean water and healthcare. Bacterial keratitis is more common in developed countries, while fungal and parasitic keratitis are more common in tropical and developing areas.
Diagnostic methods
Keratitis is diagnosed using a combination of clinical examinations, laboratory tests, and imaging techniques to determine the cause and severity of the condition.
Clinical Examination
The first step in diagnosing keratitis is a comprehensive clinical examination by an eye care professional. This includes:
- Visual Acuity Test: Evaluates the patient’s vision to determine the degree of visual impairment.
- Slit-Lamp Examination: A thorough examination of the cornea, anterior chamber, and other parts of the eye with a specialized microscope. The slit lamp can detect signs of inflammation, ulceration, and foreign bodies.
- Fluorescein Staining: Using a fluorescein dye on the eye’s surface to highlight areas of corneal damage or ulceration. The dye glows under blue light, allowing the practitioner to detect defects in the corneal epithelium.
Microbiological Testing
Microbiological testing is essential for determining the cause of infectious keratitis.
- Corneal Scrapings: Taking samples from the corneal surface with a sterile instrument. The samples are then cultured to determine whether they contain bacteria, fungi, or parasites.
- Viral Cultures and PCR: Samples with suspected viral keratitis may be tested using viral cultures or polymerase chain reaction (PCR) to detect viral DNA or RNA.
- Gram Staining and Giemsa Staining: Staining techniques for observing bacteria and other microorganisms under a microscope.
Imaging Studies
Imaging techniques can provide more information about the extent and severity of keratitis.
- Anterior Segment Optical Coherence Tomography (AS-OCT): This non-invasive imaging technique generates detailed cross-sectional images of the cornea, allowing for the assessment of the depth and extent of corneal involvement.
- Confocal Microscopy is a high-resolution imaging technique that can see individual cells and microorganisms within the cornea. It is especially useful in diagnosing Acanthamoeba keratitis.
Additional Tests
Other tests may be performed, depending on the suspected cause and clinical presentation:
- Blood Tests: To detect any underlying systemic conditions that may predispose the patient to keratitis.
- Allergy Testing: In cases of allergic keratitis, allergy testing can help identify the specific allergens causing the condition.
Keratitis treatment
The underlying cause, severity, and extent of keratitis determine treatment. The primary goals are to remove the causative agent, reduce inflammation, relieve symptoms, and avoid complications like scarring and vision loss. Here, we look at various treatment options and emerging therapies.
Pharmacologic Treatments
- Antibacterial Agents: For bacterial keratitis, topical antibiotics are the primary treatment. Fluoroquinolones (e.g., moxifloxacin, ciprofloxacin) are common first-line antibiotics. Depending on the culture results, more specific antibiotics may be prescribed. Serious infections may necessitate systemic antibiotics.
- Antiviral Medications: Antiviral medications are used to treat viral keratitis, which is most commonly caused by the herpes simplex virus. Topical antiviral drops such as trifluridine or ganciclovir are frequently used in conjunction with oral antivirals such as acyclovir or valacyclovir to reduce viral replication and prevent recurrence.
- Antifungal Therapy: To treat fungal keratitis, use antifungal eye drops like natamycin or amphotericin B. Severe cases may require oral antifungal medications such as voriconazole. Fungal infections typically require longer treatment times due to their slow response to therapy.
- Antiparasitic Treatments: Acanthamoeba keratitis is treated with a topical antiseptic combination that includes polyhexamethylene biguanide (PHMB) and chlorhexidine. The treatment regimen is intensive and lengthy, frequently necessitating months of therapy to eradicate the parasite.
Adjunctive therapies
- Corticosteroids: Topical corticosteroids can be used to reduce inflammation in some cases of keratitis, especially after the infection has been controlled. However, they should be used with caution because they can worsen infections and slow healing.
- Cycloplegic Agents: These medications alleviate pain by paralyzing the ciliary muscles of the eye, which reduces spasms and light sensitivity. Examples are atropine and cyclopentolate.
- Lubricating Eye Drops: Artificial tears and lubricating eye drops can provide symptomatic relief and help maintain corneal hydration.
Surgical Interventions
- Debridement: In cases of viral and fungal keratitis, removing infected or necrotic corneal tissue (debridement) can help reduce the microbial load and improve the effectiveness of topical treatments.
- Corneal Transplantation: Severe keratitis with significant scarring or thinning of the cornea may necessitate corneal transplantation (keratoplasty). This procedure involves replacing damaged corneal tissue with healthy donor tissue in order to restore vision.
Emerging Therapies
- Photoactivated Chromophore for Keratitis and Corneal Cross-Linking (PACK-CXL): This novel therapy uses riboflavin (vitamin B2) and ultraviolet-A (UVA) light to strengthen the cornea and eliminate infections. PACK-CXL has shown promise in treating resistant microbial keratitis and reducing the need for corneal transplants.
- Nanotechnology-Based Treatments: Researchers are investigating the use of nanoparticles to deliver antimicrobial agents directly to the site of infection. This method could improve drug efficacy while reducing side effects.
- Gene Therapy: For herpes simplex virus-induced viral keratitis, gene therapy targeting viral replication mechanisms is an emerging area of research. This method attempts to provide a more permanent solution by altering the host’s response to the virus.
Effective Ways to Improve and Avoid Keratitis
- Maintain Proper Contact Lens Hygiene: Clean and disinfect contact lenses thoroughly, and replace them as directed by your eye care provider. Unless specifically designed for overnight use, avoid wearing contact lenses while sleeping.
- Avoid Tap Water Exposure: When cleaning contact lenses or cases, avoid using tap water. To avoid contamination, use only sterile saline or contact lens solution.
- Protect Your Eyes: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports, gardening, or working with hazardous materials.
- Maintain Good Eye Hygiene: Wash your hands before touching your eyes. This reduces the risk of introducing pathogens into the eye.
- Treat Underlying Conditions: Manage conditions that predispose you to keratitis, such as dry eye syndrome or blepharitis, through appropriate treatment and regular eye care visits.
- Be Cautious with Eye Makeup: To prevent contamination, use clean applicators and replace them on a regular basis. Avoid sharing your eye makeup with others.
- Limit UV Exposure: Wear UV-protected sunglasses to protect your eyes from excessive UV light, especially when outdoors or participating in activities such as skiing or swimming.
- Monitor and Manage Medical Conditions: Keep systemic conditions like diabetes and autoimmune diseases under control, as they can increase the risk of keratitis.
- Regular Eye Examinations: Seek regular eye exams from an eye care professional to detect and treat any early signs of keratitis or other eye conditions.
Trusted Resources
Books
- “Keratitis: Causes, Diagnosis, and Treatment” by Steven M. Rowe
- “Corneal Diseases: Clinical Evaluation and Management” by Jay H. Krachmer