What is Lacrimal Gland Dislocation?
Lacrimal gland dislocation occurs when the lacrimal gland, which produces tears, moves out of its normal anatomical position. This dislocation can cause visible swelling, discomfort, and functional issues with tear production and drainage. Trauma, aging, or congenital abnormalities can all cause lacrimal gland dislocation, which has an impact on both the aesthetic appearance and health of the eye. Understanding this condition is critical for early diagnosis and effective treatment.
Comprehensive Look at Lacrimal Gland Dislocation
Lacrimal gland dislocation is a rare but serious condition that impairs the proper functioning and positioning of the lacrimal gland. The lacrimal gland is essential for maintaining eye health because it produces the aqueous layer of tear film, which lubricates, nourishes, and protects the ocular surface.
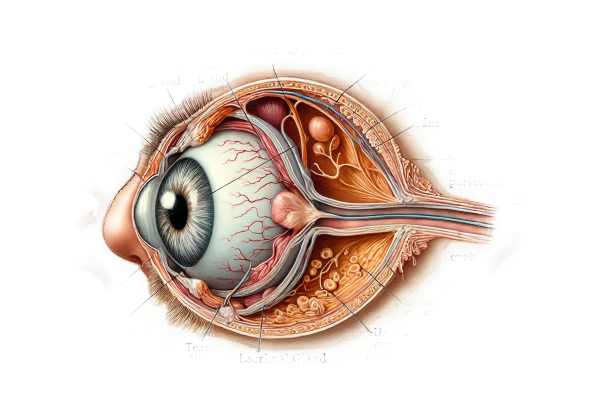
Structure and Function of the Lacrimal Gland
The lacrimal gland is a bilobed, almond-shaped structure located in the upper outer quadrant of the orbit, inside the frontal bone’s lacrimal fossa. It consists of two parts: the orbital lobe and the palpebral lobe. The gland secretes tears into the conjunctival sac via several excretory ducts. These tears then spread across the eye’s surface, providing necessary lubrication and protection before draining into the nasolacrimal duct.
Causes of Lacrimal Gland Dislocation
- Trauma: Blunt or penetrating trauma to the orbit can result in dislocation of the lacrimal gland. Accidents, sports activities, or physical altercations can all cause displacement of the gland from its anatomical position.
- Aging: As we age, the supportive tissues around the lacrimal gland weaken, causing it to sag or dislocate. This ptosis (drooping) is more common in older people due to the natural loss of tissue elasticity and strength.
- Congenital Abnormalities: Some people are born with anatomical variations or weaknesses in their orbital structures, making them prone to lacrimal gland dislocation. These congenital factors may manifest early in life or become apparent with age.
- Surgical Complications: Previous surgeries on the orbit or eyelids may inadvertently weaken the structures that support the lacrimal gland, leading to dislocation. Surgical trauma or scar tissue formation may exacerbate this condition.
- Inflammatory Conditions: Chronic inflammatory diseases, such as sarcoidosis or thyroid eye disease, can damage orbital tissues and cause the lacrimal gland to shift.
Symptoms of Lacrimal Gland Dislocation
The symptoms of lacrimal gland dislocation vary according to the severity and cause of the displacement. Common symptoms include:
- Visible Swelling: A visible bulge or swelling in the upper outer quadrant of the eyelid or orbit is a common indicator of dislocation.
- Discomfort or Pain: Patients may feel discomfort, tenderness, or pain in the affected area, particularly if the dislocation was caused by trauma or inflammation.
- Tearing and Dryness: Displacement of the lacrimal gland can disrupt normal tear production, resulting in excessive tearing (epiphora) or dryness and eye irritation.
- Functional Impairments: The dislocation can prevent proper tear drainage, resulting in chronic eye irritation, redness, and recurrent infections.
- Cosmetic Concerns: The asymmetry and swelling caused by lacrimal gland dislocation can be upsetting for patients, affecting their appearance and self-confidence.
Pathophysiology
Lacrimal gland dislocation disrupts the orbit’s normal anatomical relationships and supporting structures. The gland may relocate from its normal position in the lacrimal fossa to a more anterior, inferior, or medial location. This displacement can stretch or compress the glandular ducts, reducing tear secretion and drainage.
Trauma can directly displace the gland, damage the surrounding tissues, and cause inflammation and edema. Chronic inflammation or surgical complications can cause fibrosis and weakening of the supporting tissues, eventually allowing the gland to sag or dislocate.
Complications
If left untreated, lacrimal gland dislocation can result in a variety of complications:
- Chronic Inflammation: Improper tear drainage can result in conjunctivitis, keratitis, and other ocular surface diseases.
- Infections: Disruption in tear flow increases the risk of bacterial infections, which can result in conditions like dacryoadenitis (lacrimal gland inflammation) or dacryocystitis (lacrimal sac infection).
- Corneal Damage: Poor lubrication of the ocular surface can cause dry eye syndrome, corneal abrasions, or ulcers, jeopardizing vision and eye health.
- Functional and Cosmetic Issues: The physical appearance and functional impairments caused by lacrimal gland dislocation can have a significant impact on a patient’s quality of life, requiring prompt treatment.
Epidemiology
Lacrimal gland dislocation is a rare condition with limited epidemiological data available. It is more common in older adults as a result of age-related tissue changes, as well as in people who have had orbital trauma or inflammatory diseases. Both men and women are susceptible, and there is no significant gender bias.
Risk Factors
Several factors can raise the possibility of developing lacrimal gland dislocation:
- Age: Older people are more vulnerable due to natural deterioration of the orbital structures.
- Trauma: A history of orbital or facial trauma heightens the risk.
- Inflammatory Diseases: Sarcoidosis, thyroid eye disease, and chronic sinusitis are all risk factors for dislocation.
- Surgical History: Previous orbital or eyelid surgeries may have weakened the lacrimal gland’s support structures.
- Congenital Factors: Anatomical variations or congenital weaknesses can contribute to the formation of dislocations.
Diagnostic Tools for Lacrimal Gland Dislocation
An eye care professional must conduct a thorough evaluation to accurately diagnose lacrimal gland dislocation. To determine the extent and cause of the dislocation, the process includes a detailed history, clinical examination, and various imaging techniques.
Clinical Examination
- Patient History: A detailed patient history is required to determine the onset, duration, and progression of symptoms. Questions about recent trauma, previous surgeries, chronic conditions, and any associated symptoms (such as pain, tearing, or dryness) are critical for a proper diagnosis.
- Physical Examination: An eye care professional will conduct a thorough physical examination of the eyes and surrounding structures. This includes:
- Visual Inspection: Examining the position and appearance of the lacrimal gland, looking for swelling, asymmetry, or visible bulging in the upper outer quadrant of the eyelid.
- Palpation: Gently palpate the orbital area to determine tenderness, firmness, and the precise location of the dislocated gland.
- Lacrimal Function Tests: Evaluate tear production and drainage using tests such as the Schirmer test (to measure tear production) and the dye disappearance test (to assess tear drainage).
Imaging Studies
- Computed Tomography (CT) Scan: CT imaging provides detailed cross-sectional images of the orbital structures, allowing for the precise location of the dislocated lacrimal gland as well as any associated injuries or abnormalities. CT scans are especially useful in cases of trauma because they can reveal fractures, soft tissue damage, and inflammation.
- Magnetic Resonance Imaging (MRI): MRI provides high-resolution images of soft tissues, making it useful for evaluating the lacrimal gland and its surrounding structures. MRI is particularly useful for detecting inflammation, tumors, and chronic gland-related conditions.
- Ultrasound: High-frequency ultrasound can reveal the lacrimal gland and its surrounding tissues. This non-invasive imaging technique aids in determining the gland’s size, position, and any cystic or solid lesions.
Additional Diagnostic Tools
- Tear Film Analysis: Examining the tear film can provide information about the functional impact of the dislocated gland on tear production and quality. Tear break-up time (TBUT) and osmolarity measurements are useful in diagnosing dry eye syndrome and related conditions.
- Lacrimal Scintigraphy: This nuclear medicine imaging technique involves injecting a radioactive tracer into the tear film and then imaging sequentially to monitor tear production and drainage. It is useful in determining the functional impact of the dislocation on tear dynamics.
- Biopsy: If an inflammatory or neoplastic condition is suspected, a biopsy of lacrimal gland tissue may be performed. A histopathological examination can make a definitive diagnosis and guide appropriate treatment.
Lacrimal Gland Dislocation Treatment
The goal of treating lacrimal gland dislocation is to return the gland to its proper position, relieve symptoms, and avoid complications like chronic inflammation and infections. The cause and severity of the dislocation, as well as the patient’s overall health, determine the course of treatment.
Conservative Treatments
- Observation and Monitoring: In cases of mild dislocation without significant symptoms, particularly in older adults with age-related changes, a conservative approach involving regular monitoring and eye hygiene may be adequate. Patients should avoid any activities that could aggravate the condition.
- Medication: Anti-inflammatory medications and antibiotics may be prescribed if there is inflammation or infection. Topical steroids can alleviate swelling and discomfort, whereas antibiotic drops can prevent or treat bacterial infections.
Surgical Treatments
- Repositioning Surgery: In more severe cases or when conservative treatments fail, surgical repositioning of the lacrimal gland may be required. This procedure involves reattaching the gland to its normal anatomical position with sutures or other fixation methods. The surgery aims to restore the gland’s function while also improving tear production and drainage.
- Orbital Decompression: When dislocation is linked to conditions such as thyroid eye disease, orbital decompression surgery may be performed. This procedure relieves pressure in the orbit, allowing the gland and other orbital contents to return to their original position.
- Canthoplasty: This surgical procedure involves tightening the lateral canthal tendon to better support the lacrimal gland and prevent further dislocation. It is frequently combined with repositioning surgery to achieve the best results.
Innovative and Emerging Therapies
- Minimally Invasive Techniques: Advances in surgical technology have resulted in the creation of minimally invasive techniques for lacrimal gland repositioning. Endoscopic approaches enable precise gland repositioning with smaller incisions, shorter recovery times, and minimal scarring.
- Regenerative Medicine: Studies into regenerative medicine and tissue engineering show promise for treating lacrimal gland dislocation. Stem cell therapy and growth factor treatments seek to repair and strengthen the supportive tissues surrounding the gland, potentially reducing the need for surgery.
- Custom Implants and Devices: Novel custom implants and devices are being developed to support the lacrimal gland and keep it in the proper position. These implants can provide structural support and prevent recurrent dislocations, improving the efficacy of surgical procedures.
- Targeted Therapies for Inflammatory Conditions: For patients suffering from inflammatory conditions such as sarcoidosis or thyroid eye disease, targeted biological therapies that modulate the immune response are being investigated. These treatments aim to reduce inflammation and prevent the secondary effects that lead to gland dislocation.
By combining established surgical techniques with emerging therapies, healthcare providers can provide comprehensive treatment options for patients with lacrimal gland dislocation, with the goal of restoring normal function, alleviating symptoms, and improving quality of life.
Effective Methods for Improving and Avoiding Lacrimal Gland Dislocation
- Protect Your Eyes: Wear protective eyewear when participating in activities that may result in facial or ocular trauma, such as sports, construction work, or any activity involving potential facial impact.
- Manage Inflammatory Conditions: If you have a chronic inflammatory condition, such as thyroid eye disease or sarcoidosis, stick to your treatment plan to reduce inflammation and the risk of lacrimal gland complications.
- Regular Eye Examinations: Schedule regular eye exams to monitor your eyes’ health and detect any early signs of lacrimal gland dislocation or other ocular problems. Early detection and intervention can halt progression.
- Avoid Excessive Eye Rubbing: Do not vigorously rub your eyes, as this can cause trauma to the delicate tissues surrounding the lacrimal gland and increase the risk of dislocation.
- Post-Surgical Care: If you have had orbital or eyelid surgery, follow your postoperative care instructions carefully to ensure proper healing and avoid complications that could result in dislocation.
- Maintain Overall Eye Health: To keep your eyes healthy, practice good eye hygiene, stay hydrated, and wear UV-protective sunglasses.
- Control Allergies: Effectively manage allergic reactions to avoid chronic eye rubbing and inflammation, both of which can weaken the lacrimal gland’s support structures.
- Use Lubricating Eye Drops: To avoid dryness and irritation, especially if you have dry eyes, use lubricating eye drops as directed by your eye care professional.
- Healthy Lifestyle Choices: Eat a well-balanced diet, exercise regularly, and avoid smoking to improve overall eye health and lower the risk of lacrimal gland dislocation.
- Prevent Unnecessary Eye Strain: Take frequent breaks from activities that strain your eyes, such as prolonged screen time, to avoid fatigue and maintain eye health.
Trusted Resources
Books
- “Diseases of the Lacrimal System” by John D. Dartt
- “Principles and Practice of Lacrimal Surgery” by Mohammad Javed Ali






