What is lattice dystrophy?
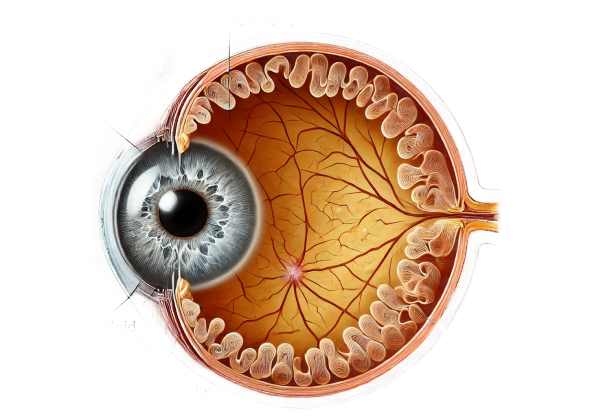
Lattice dystrophy is a genetic eye disorder that affects the cornea, the transparent, dome-shaped surface that covers the front of the eye. This condition is defined by the accumulation of abnormal protein fibers, known as amyloid deposits, within the corneal stroma. These deposits form branching, lattice-like lines that can cause clouding and blurred vision over time. Typically, lattice dystrophy appears in childhood or early adulthood and progresses gradually, necessitating medical intervention to manage symptoms and preserve vision.
Exploring Lattice Dystrophy in Detail
Lattice dystrophy is a type of corneal dystrophy, which refers to a group of inherited disorders that affect corneal clarity and function. Lattice dystrophy is classified as a stromal corneal dystrophy because it primarily affects the cornea’s stroma, which is the thick middle layer. The formation of amyloid deposits within the corneal stroma, resulting in a lattice or crisscross pattern, is the distinguishing feature of lattice dystrophy.
Pathology and Genetics
Genetic mutation is the underlying cause of lattice dystrophy. The most common cause is a mutation in the TGFBI gene (transforming growth factor beta-induced), which encodes a protein involved in cell adhesion and signaling. These mutations cause abnormal protein accumulation in the corneal stroma, known as amyloid deposits. These deposits interfere with the regular arrangement of collagen fibers in the cornea, resulting in the distinctive lattice pattern.
Lattice dystrophy is typically inherited in an autosomal dominant pattern, which means that an affected person has a 50% chance of passing the condition down to their offspring. However, even among family members carrying the same mutation, the severity and age at onset can differ.
Clinical Features and Symptoms
Lattice dystrophy usually appears in the first or second decade of life, but the exact age of onset varies. Early symptoms frequently include mild visual disturbances and light sensitivity (photophobia). As the condition progresses, the following symptoms may become more prominent:
- Blurred Vision: Amyloid deposits cause corneal opacification, resulting in a gradual reduction in visual acuity.
- Recurrent Corneal Erosions: Abnormal deposits can make the cornea’s epithelial layer unstable, resulting in recurring erosions. These erosions are painful and can cause redness, tearing, and a feeling like a foreign body in the eye.
- Decreased Contrast Sensitivity: Because of the corneal haze, people may find it difficult to distinguish objects against similar-colored backgrounds.
The rate of progression can vary greatly. In some cases, people’s vision may remain relatively stable for years, while others may see a rapid decline.
Histopathology
Lattice dystrophy is defined by the presence of amyloid deposits in the corneal stroma. These deposits are made up of abnormal protein fibers that are typically stained with Congo red dye, which produces apple-green birefringence under polarized light, indicating the presence of amyloid. During an eye exam, slit-lamp biomicroscopy can reveal the deposits as refractile, branching lines.
Variations of Lattice Dystrophy
Lattice dystrophy is not a homogenous condition; there are several variants, each with its own clinical and genetic features:
- Lattice Dystrophy Type I (Classic Type): The most common form, which typically appears in the first decade of life. It has relatively fine lattice lines and recurring erosions.
- Lattice Dystrophy Type II (Meretoja Syndrome): This variant is characterized by systemic amyloidosis, which affects not only the cornea but also the skin, cranial nerves, and other organs. Mutations in the GSN gene (gelsolin) cause this condition.
- Lattice Dystrophy Type III and IIIA: These variants appear later in life, often in the fourth decade, and have thicker lattice lines. They may progress more slowly and experience fewer erosions than Type I.
Effects on Quality of Life
Lattice dystrophy can have a significant impact on quality of life. Recurrent corneal erosions can cause chronic pain, necessitating frequent medical visits and possible absences from work or school. Progressive vision loss can impair daily activities such as reading, driving, and recognizing faces. Emotional and psychological effects, such as anxiety and depression, are common, especially when the condition has a significant impact on visual function.
Differential Diagnosis
Several other corneal dystrophies and ocular conditions can present with similar symptoms, so an accurate diagnosis is critical. Conditions to consider in the differential diagnosis are:
- Granular Corneal Dystrophy: Identified by discrete, crumb-like opacities in the stroma that appear as white, snowflake-like spots.
- Macular Corneal Dystrophy is characterized by diffuse stromal opacification and gray-white spots, with the central cornea typically spared.
- Meesmann Corneal Dystrophy is characterized by small, round, gray-white epithelial cysts that cause mild visual impairment and recurrent erosions.
Diagnostic methods
Lattice dystrophy is diagnosed using a combination of clinical examination, imaging studies, and genetic tests. The primary goal is to identify the distinctive corneal changes and confirm the presence of amyloid deposits, while distinguishing lattice dystrophy from other corneal conditions with similar symptoms.
Clinical Examination
An ophthalmologist performs a thorough clinical examination to diagnose lattice dystrophy. The key components of the examination are:
- Slit-Lamp Biomicroscopy: This is the most important tool for identifying the distinctive lattice lines in the corneal stroma. The slit lamp allows the ophthalmologist to examine the cornea with high magnification and illumination, revealing branching, refractile lines, and any associated corneal opacities.
- Corneal Sensitivity Test: Recurrent corneal erosions may cause decreased corneal sensitivity, which can be measured with a cotton swab or specialized esthesiometers.
Imaging Studies
Several imaging techniques can provide more information about the corneal structure and the extent of amyloid deposits:
- Corneal Topography: This technique maps the cornea’s surface curvature, which aids in the identification of any irregularities caused by amyloid deposits. It can also track changes over time.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT generates high-resolution cross-sectional images of the cornea, allowing for precise visualization of the depth and distribution of amyloid deposits. This non-invasive imaging technique is especially useful for monitoring disease progression and planning surgical interventions.
Genetic Testing
Given the hereditary nature of lattice dystrophy, genetic testing is critical for confirming the diagnosis and identifying specific mutations. Genetic testing typically includes:
- DNA Sequencing: This method examines the TGFBI gene (and other relevant genes) for known mutations linked to lattice dystrophy. Identifying the specific mutation can reveal information about the subtype of lattice dystrophy and its expected clinical course.
- Family Screening: Genetic testing can also be provided to family members of affected individuals in order to identify carriers and potentially diagnose asymptomatic individuals early.
Ancillary tests
Ancillary tests may be used when the diagnosis is unclear or more information is required.
- Confocal Microscopy: This technique produces detailed images of the corneal cells as well as the structure of amyloid deposits at the cellular level.
- Histopathological Examination: In some cases, a corneal biopsy may be necessary to obtain a tissue sample for histopathological examination. Staining with Congo red dye and examining under polarized light can reveal the presence of amyloid deposits.
Management and Treatment of Lattice Dystrophy
The treatment for lattice dystrophy focuses on symptom management, preventing complications, and preserving vision. The approach varies based on the severity of the condition and the patient’s specific symptoms. Here are some important treatment options:
Medical Management
- Lubricating Eye Drops and Ointments: For people who have recurring corneal erosions, artificial tears and lubricating ointments can help keep the cornea hydrated, reduce discomfort, and promote healing.
- Bandage Contact Lenses: These specialized lenses can protect the cornea, alleviate pain from recurring erosions, and aid in epithelial healing.
- Antibiotic Eye Drops: Erosions pose a risk of secondary bacterial infection. Prophylactic antibiotic drops can help prevent infections and promote healing.
Surgical Interventions
When conservative treatments do not effectively manage symptoms or when vision is significantly impaired, surgical options may be considered.
- Phototherapeutic Keratectomy (PTK): This laser procedure removes superficial corneal layers, smoothing the surface and removing amyloid deposits. PTK can improve vision and reduce the number of recurring erosions.
- Lamellar Keratoplasty: This technique involves selectively removing and replacing the affected corneal layers while preserving healthy tissue. It is especially beneficial for patients with advanced disease that has only affected the superficial corneal layers.
- Penetrating Keratoplasty (Corneal Transplant): In severe cases with extensive corneal stroma damage, a full-thickness corneal transplant may be required. This procedure involves replacing the damaged cornea with a donor cornea, which greatly improves vision.
Innovative and Emerging Therapies
Recent advances in medical research have opened up new possibilities for treating lattice dystrophy.
- Gene Therapy: Investigative therapies seek to correct the underlying genetic mutations that cause lattice dystrophy. Researchers hope that delivering functional copies of the TGFBI gene to corneal cells will prevent or slow the accumulation of amyloid deposits.
- Nanomedicine: The use of nanoparticles to deliver therapeutic agents directly to the corneal stroma is a developing field. This approach has the potential to improve drug delivery efficiency while also reducing treatment frequency.
- CRISPR-Cas9: Gene editing technologies such as CRISPR-Cas9 show promise for directly repairing the genetic mutations that cause lattice dystrophy. While still in the experimental phase, these techniques may provide a long-term solution for managing the condition.
Effective Ways to Improve and Prevent Lattice Dystrophy
Preventive measures and lifestyle changes can help manage and even delay the progression of lattice dystrophy. Here are some key steps to consider:
- Regular Eye Examinations: Schedule comprehensive eye exams with an ophthalmologist to monitor your condition and detect any changes early.
- Genetic Counseling: For families with a history of lattice dystrophy, genetic counseling can provide valuable information about the risk of passing the condition to offspring, allowing them to make informed reproductive decisions.
- Protective Eyewear: Wear sunglasses with UV protection to protect your eyes from harmful ultraviolet rays, which can worsen corneal damage.
- Avoid Eye Trauma: Take precautions to avoid eye injuries, as they can aggravate corneal erosions and hasten the progression of lattice dystrophy.
- Maintain Good Eye Hygiene: Practice proper eye care routines to avoid infections and complications from corneal erosions.
- Use Lubricating Eye Drops: Using artificial tears on a regular basis can help keep the cornea hydrated and relieve dry eye discomfort.
- Healthy Diet: Eat a well-balanced diet high in vitamins A, C, and E, as well as omega-3 fatty acids, which are necessary for overall eye health.
- Avoid Smoking: Smoking can cause a variety of eye conditions, including corneal damage. Quitting smoking can benefit your vision and overall health.
Trusted Resources
Books
- “Corneal Dystrophies and Degenerations” by Jay H. Krachmer and Mark J. Mannis
- “Cornea: Fundamentals, Diagnosis and Management” by Jay H. Krachmer, Mark J. Mannis, and Edward J. Holland
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
Online Resources
- National Eye Institute (NEI) – nei.nih.gov
- American Academy of Ophthalmology (AAO) – aao.org
- Genetics Home Reference – Lattice Corneal Dystrophy – ghr.nlm.nih.gov
- Orphanet – Lattice Dystrophy – orpha.net






