What is Nasolacrimal Duct Obstruction?
Nasolacrimal duct obstruction (NLDO) is when the nasolacrimal duct, which drains tears from the eye into the nasal cavity, becomes clogged. This causes excessive tearing (epiphora), which can result in recurring eye infections or inflammation. NLDO can affect people of all ages, but it is most common in infants and older adults. Understanding the underlying causes, symptoms, and diagnostic methods is critical for successful management and treatment of this condition.
Detailed Investigation of Nasolacrimal Duct Obstruction
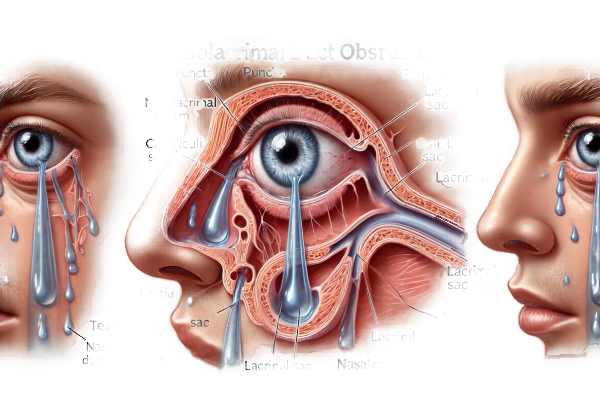
Nasolacrimal duct obstruction refers to a blockage in the tear drainage system, specifically the nasolacrimal duct. This obstruction prevents tears from properly draining through the puncta (small openings in the corners of the eyelids), canaliculi, lacrimal sac, and nasal cavity. As a result, tears overflow onto the face, causing persistent tearing and discomfort.
Anatomy and Physiology
The lacrimal apparatus consists of the lacrimal glands, which produce tears, and the tear drainage system, which includes:
- Puncta: Small openings on the inner corners of the upper and lower eyelids.
- Canaliculi are narrow channels that transport tears from the puncta to the lacrimal sac.
- Lacrimal Sac: A reservoir at the inner corner of the eye that collects tears from the canaliculi.
- Nasolacrimal Duct: A duct that carries tears from the lacrimal sac to the nasal cavity.
Causes of Nasolacrimal Duct Obstruction
Obstruction of the nasolacrimal duct can be either congenital or acquired.
Congenital NLDO
Congenital NLDO is present from birth and is a common cause of excessive tearing in infants. It results from incomplete canalization of the nasolacrimal duct during fetal development. The blockage usually occurs at the Hasner valve, which is located at the duct’s distal end. The majority of cases resolve spontaneously within the first year of life, as the duct matures.
Acquired NLDO
Acquired NLDO can develop at any age for a variety of reasons, including:
- Infections: Chronic infections like dacryocystitis (inflammation of the lacrimal sac) can cause scarring and obstruction.
- Trauma: Injuries to the face or nose can harm the nasolacrimal duct.
- Inflammatory Conditions: Sarcoidosis and Wegener’s granulomatosis can cause granulomatous inflammation, resulting in duct obstruction.
- Tumors: Benign or malignant tumors in the nasal cavity or lacrimal apparatus can obstruct the ducts.
- Aging: Degenerative changes caused by aging can narrow or block the duct.
Symptoms
The main symptom of NLDO is epiphora, or excessive tearing. Additional symptoms may include:
- Recurrent Eye Infections: Blockage can cause stagnant tears, providing a breeding ground for bacteria and resulting in recurrent conjunctivitis or dacryocystitis.
- Swelling and Redness: Inflammation or infection of the lacrimal sac can result in swelling, redness, and tenderness near the inner corner of the eye.
- Discharge: The discharge of mucus or pus from the puncta, particularly when pressing on the lacrimal sac, indicates infection.
- Blurred Vision: Excessive tearing can impair vision and cause discomfort.
Pathophysiology
In NLDO, the normal drainage of tears is impaired, resulting in tear stagnation. This stagnation creates an environment that encourages bacterial growth, increasing the risk of infection and inflammation. Chronic obstruction can cause distention of the lacrimal sac (dacryocystocele), complicating the condition.
Epidemiology
NLDO is fairly common in infants, accounting for approximately 6% of all newborns. The majority of cases resolve spontaneously within the first year. In adults, the incidence rises with age and affects more women than men, most likely due to anatomical differences and hormonal influences.
Complications
If left untreated, NLDO can cause a variety of complications:
- Chronic Dacryocystitis: A persistent infection of the lacrimal sac resulting in pain, redness, and swelling.
- Abscess Formation: Severe infections can result in abscess formation, necessitating surgical treatment.
- Cellulitis: The infection can spread to the surrounding tissues, resulting in preseptal or orbital cellulitis, which is a serious condition that requires immediate treatment.
- Vision Impairment: Chronic tearing and infections can disrupt daily activities and quality of life.
Effects on Quality of Life
NLDO has a significant impact on quality of life, causing chronic discomfort, social embarrassment due to tearing, and the burden of recurring infections. Prompt diagnosis and treatment are critical for relieving symptoms and preventing complications.
Diagnostic Techniques for Nasolacrimal Duct Obstruction
The clinical evaluation, diagnostic tests, and imaging studies used to diagnose nasolacrimal duct obstruction are all involved. These methods aid in determining the location and cause of the obstruction, allowing for more appropriate treatment.
Clinical Evaluation
The first step in diagnosing NLDO is a comprehensive clinical evaluation by an ophthalmologist. This involves gathering patient history, including symptom onset, duration, severity, and any history of trauma, infections, or systemic conditions.
- Physical Examination: Examine the eyelids, puncta, and surrounding structures for signs of swelling, redness, or discharge. Gentle pressure on the lacrimal sac may result in discharge, which indicates infection.
Dye Disappearance Test (DDT)
The dye disappearance test is a simple and non-invasive method for evaluating tear drainage. A drop of fluorescein dye is placed in the conjunctival sac, and the tear film is examined under a blue light. Normally, the dye should drain through the nasolacrimal system in 5 minutes or less. A prolonged retention of the dye indicates an obstruction.
Lacrimal Irrigation
Lacrimal irrigation involves flushing the nasolacrimal system with saline via a cannula inserted into the puncta. This test determines the patency of the tear drainage system. If fluid flows freely into the nose, the system is open. Fluid resistance or regurgitation indicates the presence of an obstruction.
Probing and Syringing
Probing entails inserting a thin metal probe through the puncta and nasolacrimal duct to locate and potentially relieve the obstruction. This procedure is commonly used on infants with congenital NLDO. Syringing with saline can be used concurrently to confirm the duct’s patency.
Imaging Studies
Imaging studies provide detailed visualization of the nasolacrimal system, which aids in determining the location and cause of the obstruction.
- Dacryocystography: This X-ray imaging technique involves injecting a contrast dye into the nasolacrimal duct and then taking radiographs. It shows detailed images of the tear drainage system, highlighting any blockages or anatomical abnormalities.
- Computed Tomography (CT) Scan: A CT scan of the orbits and sinuses can aid in determining the structural causes of NLDO, such as tumors, trauma, or inflammatory conditions. It can produce high-resolution images of the bones and soft tissues.
- Magnetic Resonance Imaging (MRI): MRI can assess soft tissue structures and detect inflammatory or neoplastic conditions affecting the nasolacrimal system. It produces detailed images with no radiation exposure.
- Nuclear Scintigraphy: This method involves injecting a radioactive tracer into the tear film and tracking its movement through the nasolacrimal system with a gamma camera. It aids in determining the functional status of the tear drainage system.
Endoscopy
Nasolacrimal endoscopy is the process of inserting a small, flexible endoscope through the puncta and nasolacrimal duct to directly visualize the tear drainage system. This technique enables precise identification of the obstruction site and can help plan surgical interventions.
Nasolacrimal Duct Obstruction Treatment Options
Treatment for nasolacrimal duct obstruction (NLDO) aims to restore normal tear drainage, alleviate symptoms, and prevent complications. The cause, severity, and age of the patient all influence treatment decisions. We investigate various conventional treatments and highlight innovative and emerging therapies.
Conventional Treatments
- Conservative Management: For infants with congenital NLDO, conservative management is frequently the first line of treatment. This includes:
- Massage (Crigler Technique): Parents are instructed to massage the lacrimal sac on a daily basis in order to help open the Hasner valve obstruction. This technique can aid in the drainage and removal of the obstruction.
- Observation: Many cases of congenital NLDO resolve spontaneously before the age of one year. Regular monitoring is essential for assessing progress.
- Probing: When conservative management fails, probing is the next step, especially in infants and young children. To remove the obstruction, a thin, blunt probe is passed through the puncta and the nasolacrimal duct. This procedure is typically performed in infants under local anesthesia and has a high success rate.
- Lacrimal Irrigation: This procedure entails flushing the nasolacrimal duct with saline to remove any debris or mucus that may be causing the obstruction. It is frequently combined with probing to increase its effectiveness.
- Dacryocystorhinostomy (DCR) is the gold standard surgical treatment for acquired NLDO in adults. It opens up a new drainage pathway between the lacrimal sac and the nasal cavity. There are two primary approaches:
- External DCR: An incision is made on the side of the nose to gain access to the lacrimal sac. The success rate is high, but it leaves a minor scar.
- Endoscopic DCR: This minimally invasive procedure involves inserting an endoscope through the nasal cavity. It avoids external scarring and has similar success rates to external DCR.
- Balloon Catheter Dilation: This procedure entails inserting and inflating a balloon catheter through the nasolacrimal duct to widen it and clear the obstruction. It is less invasive than DCR and can effectively treat both congenital and acquired NLDO.
Innovative and Emerging Therapies
- Lacrimal Stenting and Intubation: Silicone tubes or stents are inserted into the nasolacrimal duct to keep it open and allow drainage. This method is frequently used in conjunction with DCR, or as an alternative to probing in recurrent cases.
- Laser-Assisted Dacryocystorhinostomy: This procedure uses laser technology to create a new drainage pathway. It provides precise tissue removal, minimal bleeding, and faster recovery times.
- Mitomycin C Application: Mitomycin C, an anti-fibrotic agent, can be used during DCR surgery to reduce scar formation and increase success rates. It inhibits fibroblast proliferation, lowering the chances of re-obstruction.
- Minimally Invasive Endoscopic Techniques: Advances in endoscopic technology are improving the precision and outcomes of endoscopic DCR. Enhanced visualization and specialized instruments make surgeries more effective and safer.
- Gene Therapy and Regenerative Medicine: While still in the experimental stage, research into gene therapy and regenerative medicine shows promise for treating NLDO. These treatments aim to repair or regenerate the nasolacrimal duct tissues, which could provide a long-term solution.
Healthcare providers can provide personalized and effective NLDO management by combining traditional treatments with innovative therapies, thereby improving patient outcomes and quality of life.
Effective Ways to Improve and Avoid Nasolacrimal Duct Obstruction
- Maintain Good Hygiene: To avoid infections that can cause NLDO, clean the eyelids and surrounding areas on a regular basis. To prevent irritation, use gentle, hypoallergenic cleansers.
- Manage Allergies: Treat allergic conditions that cause chronic nasal inflammation and congestion, as these can contribute to NLDO. Follow your healthcare provider’s recommendations for antihistamines and nasal sprays.
- Avoid Nasal Trauma: Wear appropriate safety gear when participating in activities that may result in facial trauma. Avoid inserting objects into the nose that may harm the nasolacrimal duct.
- Treat Infections Right Away: Seek immediate treatment for any eye or nasal infections to keep them from spreading to the nasolacrimal duct. To ensure complete resolution, follow the prescribed medication regimen.
- Stay Hydrated: Drink plenty of water to keep your body hydrated and support healthy mucous membranes. Proper hydration can help prevent mucus from thickening and blocking the duct.
- Regular Eye Check-ups: Schedule regular eye exams to detect any early symptoms of NLDO or other eye conditions. Early diagnosis and treatment can help to avoid complications.
- Gentle Eye Care for Infants: Infants should receive gentle eye care and cleaning to avoid congenital NLDO. If you suspect NLDO, follow your pediatrician’s massage technique recommendations.
- Avoid Environmental Irritants: Limit your exposure to smoke, pollutants, and other environmental irritants, which can cause chronic nasal and sinus inflammation and contribute to NLDO.
- Monitor Symptoms: Be on the lookout for symptoms like excessive tearing, recurring eye infections, or nasal discharge. Early identification of symptoms enables prompt medical intervention.
- Follow Post-Surgical Care Instructions: If you have had surgery for NLDO, strictly follow the post-operative care instructions to avoid complications and ensure a successful recovery.
Trusted Resources
Books
- “Oculoplastics and Orbit: Aesthetic and Functional Oculofacial Plastic Surgery” by William P. Chen
- “The Lacrimal System: Diagnosis, Management, and Surgery” by Adam J. Cohen and Michael Mercandetti
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling










