What is neovascular glaucoma?
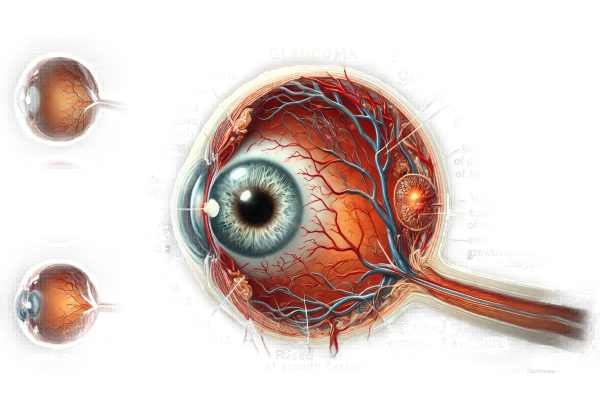
Neovascular glaucoma is a severe and vision-threatening type of secondary glaucoma characterized by the formation of abnormal new blood vessels on the iris and drainage angle of the eyeball. This abnormal neovascularization prevents the normal outflow of aqueous humor, resulting in elevated intraocular pressure (IOP). The condition is frequently associated with underlying systemic or ocular diseases such as diabetic retinopathy, central retinal vein occlusion, or other ischemic retinal disorders. Early diagnosis and treatment are critical for preventing significant vision loss and effectively managing the underlying causes.
Detailed Examination of Neovascular Glaucoma
Neovascular glaucoma is a complex and challenging condition caused by the growth of new, abnormal blood vessels in the eye. These vessels develop primarily in response to retinal ischemia, which occurs when the retina does not receive adequate blood supply, resulting in the release of vascular endothelial growth factor (VEGF). VEGF stimulates the formation of new blood vessels to compensate for a lack of oxygen, but in neovascular glaucoma, these vessels grow inappropriately on the iris and in the eye’s drainage angle, obstructing fluid outflow and raising intraocular pressure.
Pathophysiology
The pathophysiology of neovascular glaucoma consists of several key steps:
- Retinal Ischemia: Conditions such as diabetic retinopathy and retinal vein occlusion reduce blood flow to the retina, resulting in hypoxia.
- VEGF Release: Hypoxic retinal tissues secrete VEGF, which promotes the formation of new blood vessels.
- Neovascularization: New blood vessels form on the anterior segment of the eye, primarily on the iris (rubeosis iridis) and trabecular meshwork.
- Angle Closure: The abnormal blood vessels block the trabecular meshwork, resulting in decreased aqueous outflow.
- Increased IOP: A blockage in the drainage angle causes elevated intraocular pressure, which, if not controlled, can cause optic nerve damage and vision loss.
Clinical Features
Neovascular glaucoma typically has three stages: pre-glaucoma, open-angle, and angle-closure.
- Pre-Glaucoma Stage: In the early stages, patients may be asymptomatic or have minor visual disturbances. Neovascularization starts on the iris (rubeosis iridis) and the anterior chamber angle.
- Open-Angle Stage: As neovascularization advances, new vessels invade the trabecular meshwork, causing an increase in IOP. Patients may begin to notice symptoms such as eye pain, redness, decreased vision, and halos around lights.
- Angle-Closure Stage: The final stage is the formation of fibrovascular membranes, which contract and pull the peripheral iris over the trabecular meshwork, resulting in secondary angle-closure glaucoma. Severe eye pain, headache, nausea, and significant vision loss are common symptoms of this stage.
Risk Factors
Several risk factors contribute to the development of neovascular glaucoma, particularly conditions that cause retinal ischemia and subsequent VEGF release:
- Diabetic Retinopathy: Both proliferative and non-proliferative diabetic retinopathy can cause retinal ischemia, making diabetes a major risk factor.
- Retinal Vein Occlusion: A central or branch retinal vein occlusion can result in significant retinal hypoxia and neovascularization.
- Ocular Ischemic Syndrome: Reduced blood flow to the eye due to carotid artery disease can cause chronic retinal ischemia and neovascular glaucoma.
- Retinal Detachment: Prolonged retinal detachment can result in ischemia and VEGF production.
- Inflammatory Ocular Conditions: Uveitis and other inflammatory conditions can impair normal vascular function and lead to neovascularization.
- Trauma: Ocular trauma may cause abnormal blood vessel growth and secondary glaucoma.
Complications
If not treated promptly, neovascular glaucoma can cause a number of serious complications.
- Optic Nerve Damage: High IOP can irreversibly damage the optic nerve, resulting in permanent vision loss.
- Corneal Edema: Increased pressure in the eye can cause corneal swelling and decreased vision clarity.
- Pain and Discomfort: Patients frequently experience severe eye pain, redness, and discomfort, which has a significant impact on their quality of life.
- Phthisis Bulbi: In severe cases, the eye can become shrunken and non-functional due to chronic high IOP and tissue damage.
Differential Diagnosis
Several conditions can mimic the clinical presentation of neovascular glaucoma, necessitating a comprehensive differential diagnosis.
- Primary Open-Angle Glaucoma (POAG): Unlike neovascular glaucoma, POAG does not result in neovascularization or angle closure.
- Angle-Closure Glaucoma: Anatomical abnormalities, not neovascularization, cause primary angle-closure glaucoma.
- Uveitic Glaucoma: Uveitis-related inflammatory glaucoma can cause elevated IOP but no neovascularization.
- Pseudoexfoliative Glaucoma: This condition, characterized by the deposition of pseudoexfoliative material on the lens and trabecular meshwork, causes increased IOP but no neovascularization.
Diagnostic methods
To confirm the presence of abnormal blood vessels and elevated intraocular pressure, a clinical examination and specialized tests are required to diagnose neovascular glaucoma.
Slit Lamp Examination
A slit-lamp examination is essential for detecting neovascularization of the iris (rubeosis iridis) and the anterior chamber angle. The slit lamp magnifies the eye structures, making it easier to detect early signs of neovascularization.
Gonioscopy
Gonioscopy is required to visualize the drainage angle of the eye. This procedure aids in determining the extent of angle closure due to neovascularization and fibrovascular membranes. It allows for direct observation of angle structures and can detect the presence of abnormal blood vessels.
Tonometry
Measuring intraocular pressure (IOP) is an important diagnostic step in glaucoma. Tonometry can detect elevated IOP, which is a key indicator of impaired aqueous humor outflow. To obtain accurate IOP readings, a variety of methods are used, including Goldmann applanation tonometry.
Fluorescein angiogram
Fluorescein angiography involves injecting a fluorescent dye into the bloodstream and taking images of the retinal and choroidal circulation. This test detects areas of retinal ischemia and neovascularization, which aids in the diagnosis and monitoring of neovascular glaucoma.
Optical Coherence Tomography(OCT)
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve. OCT can detect retinal thickening, edema, and optic nerve damage, which are all common in neovascular glaucoma patients. It also helps to monitor disease progression and response to treatment.
Ultrasound Biomicroscopy (UBM)
UBM provides detailed images of the anterior segment, which includes the drainage angle and the ciliary body. This imaging technique is useful in assessing structural changes like angle closure and neovascularization. UBM provides important information for diagnosing and treating neovascular glaucoma.
Effective Treatment Methods for Neovascular Glaucoma
The treatment of neovascular glaucoma focuses on lowering intraocular pressure (IOP), preventing neovascularization, and addressing the underlying causes. A combination of medical, laser, and surgical interventions is frequently required to effectively manage this complex condition.
Medical Treatment
- Anti-VEGF Therapy: Anti-VEGF agents such as bevacizumab (Avastin), ranibizumab (Lucentis), and aflibercept (Eylea) are injected into the eye to prevent the formation of new blood vessels. These medications help to reduce neovascularization and control IOP by inhibiting abnormal blood vessel proliferation.
- Corticosteroids: Intravitreal or periocular corticosteroid injections can help reduce inflammation and edema caused by neovascular glaucoma. Steroids, such as triamcinolone acetonide, can help manage the disease’s inflammatory component.
- IOP-Lowering Medications: Topical medications such as beta-blockers (timolol), alpha agonists (brimonidine), carbonic anhydrase inhibitors (dorzolamide, brinzolamide), and prostaglandin analogs (latanoprost, bimatoprost) are commonly used to reduce IOP. Acetazolamide, an oral carbonic anhydrase inhibitor, may also be used to reduce pressure.
Laser Treatment
- Panretinal Photocoagulation (PRP): PRP is a laser procedure that treats ischemic retinas by reducing VEGF production and neovascularization. By ablating peripheral retinal tissue, PRP reduces the stimulus for new blood vessel growth, stabilizing the condition.
- Cyclophotocoagulation: This laser treatment targets the ciliary body, reducing aqueous humor production and thus lowering IOP. Cyclophotocoagulation can be performed with a variety of laser modalities, including diode lasers and Nd:YAG lasers.
Surgical Treatment
- Trabeculectomy: This surgical procedure creates a new drainage pathway for aqueous humor, which helps to reduce IOP. Trabeculectomy is frequently combined with anti-fibrotic agents such as mitomycin-C to improve success rates and minimize scarring.
- Drainage Implants: Glaucoma drainage devices, such as the Ahmed valve or Baerveldt implant, provide an alternate route for aqueous humor outflow. These implants help control IOP in situations where traditional surgery may be ineffective.
- Endocyclophotocoagulation (ECP): ECP is a minimally invasive procedure in which an endoscope delivers laser energy directly to the ciliary body, reducing aqueous humor production and IOP.
Emerging Therapies
- Gene Therapy: Research into gene therapy seeks to target the underlying mechanisms of neovascular glaucoma. Experimental approaches include delivering genes that inhibit VEGF production or enhance natural anti-angiogenic factors, which could provide long-term solutions.
- Nanoparticle-Based Delivery Systems: Novel drug delivery systems that use nanoparticles are being developed to provide sustained release of anti-VEGF agents or corticosteroids, potentially reducing the need for frequent injections and improving patient compliance.
- Stem Cell Therapy: Researchers are looking into how stem cells can regenerate damaged ocular tissues and restore normal eye function. While still in the experimental stages, this approach may provide novel treatment options for neovascular glaucoma in the future.
Effective Ways to Improve and Prevent Neovascular Glaucoma
Preventing and treating neovascular glaucoma requires a combination of proactive measures and timely medical intervention. Here are a few effective methods:
- Regular Eye Examinations: Get regular eye exams, especially if you have diabetes or other risk factors. Early detection of retinal ischemia and neovascularization is critical.
- Control Systemic Conditions: Effectively manage chronic diseases like diabetes and hypertension. Proper control can lower the risk of retinal ischemia and neovascular glaucoma.
- Monitor Vision Changes: Be aware of any changes in vision, such as increased floaters, flashes of light, or sudden loss of vision. If you notice any of these symptoms, contact your doctor right away.
- Adhere to Treatment Plans: Carefully follow the prescribed treatments for underlying ocular or systemic conditions. Compliance with anti-VEGF injections and other therapies can help prevent progression.
- Healthy Lifestyle: Eat a well-balanced diet, exercise regularly, and quit smoking to improve overall vascular health and lower the risk of ischemic conditions.
- Manage Blood Sugar Levels: If you have diabetes, keep your blood sugar levels within the recommended range to avoid diabetic retinopathy and other complications.
- Educate Yourself: Be aware of the symptoms and risk factors of neovascular glaucoma. Knowledge enables you to take prompt action and seek appropriate treatment.
- Protect Your Eyes: Wear protective eyewear to avoid trauma, which can worsen or trigger neovascularization in susceptible individuals.
Trusted Resources
Books
- “Glaucoma: A Patient’s Guide to the Disease” by Graham E. Trope
- “Clinical Pathways in Glaucoma” by Thom J. Zimmerman
- “Glaucoma: Science and Practice” by John C. Morrison and Irvin P. Pollack






