What is vitreous neovascularization?
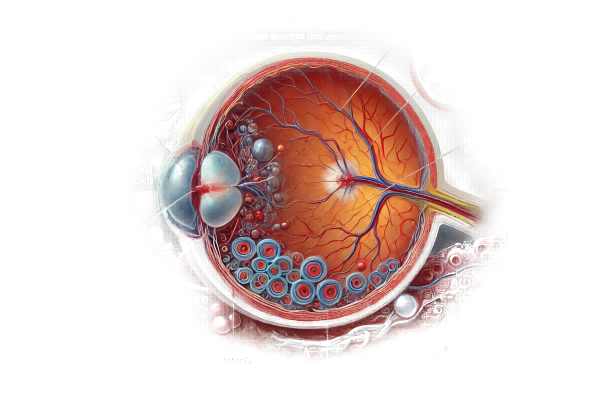
Neovascularization of the vitreous is the abnormal formation of new blood vessels within the vitreous body, which is a gel-like substance that fills the eye between the lens and the retina. This condition is frequently the result of underlying retinal ischemia or other pathological conditions that cause vascular endothelial growth factor (VEGF) release. The newly formed vessels are fragile and prone to bleeding, resulting in vitreous hemorrhage and possible vision loss. Understanding the causes, mechanisms, and consequences of vitreous neovascularization is critical for proper diagnosis and treatment.
A Closer Look at Vitreous Neovascularization
Neovascularization of the vitreous is a serious eye condition that is frequently associated with systemic and ocular diseases that impair retinal blood flow. This pathological process involves the development of new, abnormal blood vessels from the retina into the vitreous cavity. The primary cause of this neovascularization is retinal ischemia, which stimulates the production of angiogenic factors such as VEGF, promoting the formation of new vessels in an attempt to restore adequate blood supply.
Pathophysiology
The pathophysiology of vitreous neovascularization consists of several key steps:
- Retinal Ischemia: Diabetic retinopathy, retinal vein occlusion, and sickle cell retinopathy cause decreased blood flow and oxygen deprivation in the retina.
- VEGF Release: Hypoxic retinal tissues secrete VEGF and other pro-angiogenic factors to promote the formation of new blood vessels.
- Neovascularization: Newly formed vessels extend from the retinal surface to the vitreous cavity. These vessels are structurally abnormal, lacking typical supporting tissue and more susceptible to leakage and rupture.
- Complications: The fragile new vessels may bleed into the vitreous, resulting in vitreous hemorrhage. Furthermore, fibrovascular tissue proliferation can result in tractional retinal detachment, which impairs vision.
Clinical Features
Patients with vitreous neovascularization may experience a variety of symptoms, depending on the severity and activity of the neovascular process. Common clinical characteristics include:
- Floaters: Patients commonly report an increase in floaters, which are shadows cast by new blood vessels or small vitreous hemorrhages.
- Blurred Vision: As neovascularization progresses and vitreous hemorrhage occurs, patients may notice blurred or distorted vision.
- Sudden Vision Loss: A large vitreous hemorrhage can cause unexpected and severe vision loss, necessitating immediate medical attention.
During clinical examination, healthcare providers may notice:
- Neovascular Tufts: Small clusters of new vessels extending from the retina into the vitreous, visible under ophthalmoscopy.
- Vitreous Hemorrhage: Blood in the vitreous cavity can obscure the retina and complicate diagnosis.
- Fibrovascular Proliferation: Advanced cases may exhibit fibrovascular tissue, which can cause traction on the retina, resulting in detachment.
Associated Conditions
Neovascularization of the vitreous is commonly associated with a number of underlying conditions that cause retinal ischemia:
- Diabetic Retinopathy: Diabetic retinopathy is one of the most common causes, and it occurs when high blood sugar levels damage retinal blood vessels. Proliferative diabetic retinopathy (PDR) is defined by extensive neovascularization.
- Retinal Vein Occlusion: Blockage of the retinal veins can result in ischemia and neovascularization. Central retinal vein occlusion (CRVO) and branch retinal vein occlusion (BRVO) are common examples.
- Sickle Cell Retinopathy: Sickle cell disease can occlude retinal vessels, resulting in ischemic changes and neovascularization.
- Retinal Artery Occlusion: Although less common, occlusion of the retinal arteries can cause ischemia and promote neovascularization.
- Ocular Ischemic Syndrome: Reduced blood flow to the eye due to carotid artery disease can result in chronic retinal ischemia and neovascularization.
- Inflammatory Retinal Diseases: Conditions such as uveitis can cause retinal inflammation and subsequent ischemic changes, resulting in neovascularization.
Complications
Complications from vitreous neovascularization can be severe and vision-threatening.
- Vitreous Hemorrhage: The delicate neovascular vessels are prone to bleeding, resulting in blood accumulation in the vitreous cavity. This can result in sudden vision loss and obscure the retina, complicating future treatment.
- Tractional Retinal Detachment: The fibrovascular tissue associated with neovascularization can contract and pull on the retina, causing tractional detachment. This condition necessitates surgical intervention and, if not treated promptly, can lead to permanent vision loss.
- Rubeosis Iridis: Neovascularization can spread to the iris, resulting in rubeosis iridis. This can result in neovascular glaucoma, a severe type of glaucoma caused by the occlusion of the eye’s drainage angle with new blood vessels.
- Neovascular Glaucoma: When neovascularization spreads to the anterior segment, it can block aqueous outflow, resulting in increased intraocular pressure and secondary glaucoma.
Diagnostic methods
To accurately assess the extent and impact of vitreous neovascularization, several advanced diagnostic techniques are required.
Fundus Examination
Diagnosing vitreous neovascularization requires a thorough fundus examination with ophthalmoscopy. This examination provides direct visualization of the retina and vitreous cavity, revealing abnormal new vessels and potential vitreous hemorrhage. Ophthalmologists can detect neovascular tufts, fibrovascular proliferation, and associated hemorrhages in the posterior segment of the eye, indicating the presence of neovascularization.
Fluorescein angiogram
Fluorescein angiography is a valuable diagnostic tool for detecting and mapping areas of retinal ischemia and neovascularization. During this procedure, a fluorescent dye is injected into the patient’s bloodstream and then transported to the retinal blood vessels. As the dye travels through the retinal vasculature, a specialized camera captures images. This imaging technique reveals areas of leakage, ischemia, and the formation of new blood vessels, giving a clear picture of the retinal and choroidal circulation.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and vitreous. OCT is useful for visualizing the retina’s structure and detecting abnormalities such as neovascular tufts, vitreous hemorrhage, and retinal detachment. It is especially useful for determining the extent of neovascularization and its effects on the retinal architecture. OCT angiography, a variation of OCT, can improve the visualization of blood flow in the retinal and choroidal vessels, assisting in the diagnosis and monitoring of neovascularization.
B-Scan Ultrasound
When vitreous hemorrhage obscures the view of the retina, it is difficult to diagnose with standard ophthalmoscopy. This ultrasound technique generates detailed images of the posterior segment, allowing for the detection of vitreous hemorrhage, retinal detachment, and other structural changes. B-scan ultrasound is especially useful in cases where dense vitreous hemorrhage precludes other imaging methods.
Differential Diagnosis
It is critical to distinguish between vitreous neovascularization and other ocular conditions with similar presentations in order to make an accurate diagnosis and treatment. Proliferative diabetic retinopathy, central retinal vein occlusion, sickle cell retinopathy, and retinal detachment with vitreous hemorrhage can all have clinical characteristics similar to vitreous neovascularization. A thorough diagnostic workup, including detailed imaging and clinical evaluation, is required to distinguish between these conditions and make an accurate diagnosis.
Neovascularization of the Vitreous Treatment
To treat vitreous neovascularization, a multifaceted approach is required that focuses on reducing neovascularization, controlling underlying causes, and addressing complications. This condition is effectively managed using both established and emerging therapies.
Medical Treatment
- Anti-VEGF Therapy: Anti-VEGF (vascular endothelial growth factor) agents are the primary treatment for vitreous neovascularization. Intravitreal injections of bevacizumab (Avastin), ranibizumab (Lucentis), and aflibercept (Eylea) inhibit VEGF, reducing the formation of abnormal blood vessels and vascular permeability. These treatments are extremely effective at managing neovascularization and improving visual outcomes.
- Corticosteroids: Intravitreal or periocular corticosteroids, like triamcinolone acetonide, can be used to reduce inflammation and vascular leakage. These are frequently used in combination with anti-VEGF therapy to improve treatment outcomes.
Laser Treatment
- Panretinal Photocoagulation (PRP) is a laser treatment that targets the peripheral retina, reducing ischemia and VEGF production. PRP reduces neovascularization by ablating ischemic areas. This treatment is particularly effective for proliferative diabetic retinopathy and retinal vein occlusion.
- Focal Laser Therapy: When neovascularization is localized, focal laser therapy can be used to directly target and coagulate abnormal blood vessels, reducing their activity and the risk of hemorrhaging.
Surgical Treatment
- Vitrectomy: Pars plana vitrectomy is a surgical procedure that removes vitreous hemorrhage and fibrovascular tissue that can lead to tractional retinal detachment. Vitrectomy is recommended when hemorrhage impairs vision or there is a risk of retinal detachment. This procedure allows the surgeon to clear the vitreous cavity and treat retinal traction, resulting in better visual outcomes.
- Membrane Peeling: During vitrectomy, membrane peeling can be used to remove fibrovascular membranes that cause traction and neovascularization. This step is critical in avoiding recurrent detachment and subsequent complications.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy aims to provide long-term solutions by addressing the underlying genetic mechanisms that cause neovascularization. Experimental approaches include delivering genes that inhibit VEGF or enhance anti-angiogenic factors, which may reduce the need for repeat injections.
- Nanoparticle-Based Drug Delivery: Novel drug delivery systems based on nanoparticles are being developed to provide long-term release of anti-VEGF agents or corticosteroids. These systems can increase treatment efficacy while decreasing the frequency of intravitreal injections, thereby improving patient compliance.
- Stem Cell Therapy: Researchers are investigating stem cell therapy’s potential to regenerate damaged retinal tissues and restore normal vascular function. While still experimental, this approach has the potential to improve future treatment options for vitreous neovascularization.
Effective Methods to Improve and Avoid Neovascularization of the Vitreous
Lifestyle changes, early detection, and proactive medical management are all necessary to prevent and manage vitreous neovascularization. Here are a few effective methods:
- Regular Eye Exams: Get routine eye exams, especially if you have diabetes, hypertension, or other risk factors. Early detection of retinal ischemia and neovascularization is critical for timely treatment.
- Control Systemic Conditions: Manage systemic diseases like diabetes and hypertension. Proper management of these conditions can lower the risk of retinal ischemia and neovascularization.
- Monitor Vision Changes: Be aware of any changes in vision, such as increased floaters, flashes of light, or sudden loss of vision. If you notice any of these symptoms, contact your doctor right away.
- Adhere to Treatment Plans: Carefully follow the prescribed treatments for underlying ocular or systemic conditions. Compliance with anti-VEGF injections and other therapies can help prevent progression.
- Healthy Lifestyle: Eat a balanced diet, exercise regularly, and avoid smoking to improve overall vascular health and lower the risk of ischemic conditions.
- Manage Blood Sugar Levels: If you have diabetes, keep your blood sugar levels within the recommended range to avoid diabetic retinopathy and related complications.
- Educate Yourself: Be aware of the symptoms and risk factors associated with vitreous neovascularization. Knowledge enables you to take prompt action and seek appropriate treatment.
- Protect Your Eyes: Wear protective eyewear to avoid trauma, which can worsen or trigger neovascularization in susceptible individuals.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “Diabetic Retinopathy” by David J. Browning
- “Vitreous Microsurgery” by Steve Charles






