What is ocular hypertension?
Ocular hypertension is defined as elevated intraocular pressure (IOP) in the eye. Ocular hypertension, unlike glaucoma, does not cause optic nerve damage or vision loss. It is, however, regarded as a significant risk factor for glaucoma development. Monitoring and managing ocular hypertension is critical to avoiding the progression to glaucoma, the leading cause of blindness. This condition is usually detected during routine eye exams and requires ongoing monitoring to maintain eye health.
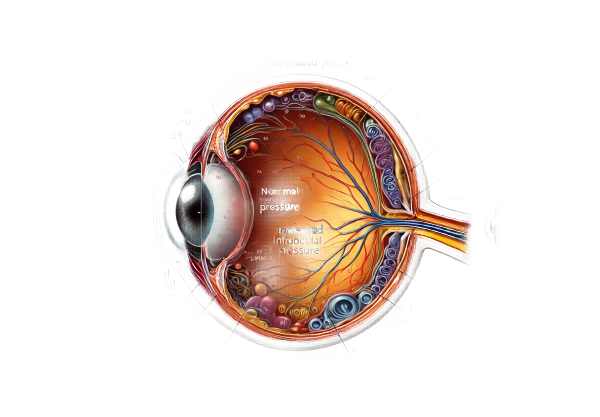
Inside Ocular Hypertension
Pathophysiology
Ocular hypertension occurs when the pressure inside the eye exceeds normal levels, as measured in millimeters of mercury (mmHg). The normal range for intraocular pressure is 10 to 21 mmHg. Pressures above this range are considered elevated and can be due to a variety of underlying mechanisms:
- Aqueous Humor Dynamics: The balance between the production and drainage of aqueous humor, or eye fluid, is critical. The ciliary body produces aqueous humor, which drains through the trabecular meshwork and the uveoscleral pathway. Disruption in this balance, whether through increased production or decreased outflow, can result in elevated IOP.
- Trabecular Meshwork Dysfunction: The trabecular meshwork is an important structure in the drainage system. Blockage or dysfunction in this meshwork can obstruct fluid outflow, resulting in elevated intraocular pressure. Aging, genetics, and certain diseases can all have an impact on the efficiency of the trabecular meshwork.
- Episcleral Venous Pressure: Elevated episcleral venous pressure can also contribute to high IOP by impeding the outflow of aqueous humor via the traditional pathway.
Risk Factors
Several factors can predispose people to ocular hypertension.
- Age: The likelihood of developing ocular hypertension rises with age, especially after the age of 40.
- Family History: A family history of ocular hypertension or glaucoma greatly increases the risk.
- Race and ethnicity: African Americans and Hispanics are more likely to develop ocular hypertension and glaucoma.
- Medical Conditions: Diabetes, hypertension, and myopia (nearsightedness) all increase the risk.
- Medications: Prolonged use of corticosteroids, whether systemic or topical, can cause increased IOP.
- Eye Trauma: Previous eye injuries or surgeries can harm the eye’s drainage system, raising the possibility of ocular hypertension.
Symptoms
Ocular hypertension is often asymptomatic, so regular eye exams are essential for detection. Unlike glaucoma, it does not cause pain, vision changes, or other obvious symptoms in the early stages. This silent nature emphasizes the importance of regular eye exams, particularly for those with risk factors.
Complications
If not treated, ocular hypertension can cause:
- Glaucoma: The most serious risk associated with ocular hypertension is the development of glaucoma, specifically primary open-angle glaucoma. Elevated IOP can cause damage to the optic nerve, resulting in vision loss.
- Optic Nerve Damage: Persistently elevated IOP can put pressure on the optic nerve, causing structural damage and functional impairment.
- Vision Loss: Chronic high IOP, if it progresses to glaucoma, can result in irreversible vision loss and blindness.
Pathogenesis of Glaucoma from Ocular Hypertension
Several pathogenic mechanisms contribute to the progression of ocular hypertension to glaucoma:
- Mechanical Theory: Elevated IOP causes mechanical stress on the optic nerve head, resulting in axonal damage and loss of retinal ganglion cells.
- Vascular Theory: High IOP can reduce blood flow to the optic nerve, causing ischemia and subsequent nerve damage.
- Neurodegenerative Theory: Chronic high IOP levels may initiate neurodegenerative processes affecting the optic nerve, similar to those seen in diseases such as Alzheimer’s.
Effects on Quality of Life
While ocular hypertension does not cause symptoms, the anxiety and stress that comes with the possibility of developing glaucoma can have an impact on a person’s quality of life. The requirement for regular monitoring and possible treatment can also be burdensome.
Prevalence
Ocular hypertension is fairly common, especially in older adults. According to studies, approximately 4-7% of people over the age of 40 have elevated IOP but no glaucoma. The prevalence rises with age, making regular eye exams critical for early detection and treatment.
Genetic Factors
Genetic predisposition is an important factor in the development of ocular hypertension. Variations in genes regulating aqueous humor production, drainage, and overall eye structure can increase susceptibility. Research is currently underway to identify specific genetic markers that contribute to this condition, which could lead to more personalized approaches to risk assessment and management.
Environmental and Lifestyle Factors
Certain lifestyle factors and environmental exposures can affect IOP levels:
- Physical Activity: Studies have shown that regular aerobic exercise can lower IOP in some people, potentially lowering the risk of ocular hypertension.
- Diet: Consuming antioxidant-rich foods, particularly green leafy vegetables and fruits, may benefit eye health and influence IOP levels.
- Caffeine and Alcohol: High caffeine intake can temporarily increase IOP, whereas moderate alcohol consumption has been associated with lower IOP in some studies. The effects of these substances on long-term IOP regulation are still being investigated.
Diagnostic Techniques for Ocular Hypertension
Clinical Examination
- Tonometry is the primary method for diagnosing ocular hypertension. The most common type is Goldmann applanation tonometry, which involves numbing the eye with drops and flattening a small section of the cornea with a device. Non-contact tonometry (air-puff test) and digital tonometry are two additional types.
- Gonioscopy: This procedure uses a special lens to examine the eye’s drainage angle (the angle between the iris and cornea through which the aqueous humor drains). It aids in determining whether the angle is open or closed, which is critical for diagnosing various types of glaucoma and understanding the underlying cause of high IOP.
- Pachymetry: Measuring corneal thickness with pachymetry is critical because corneal thickness can influence IOP readings. A thicker cornea can produce falsely high IOP readings, whereas a thinner cornea can cause an underestimation of IOP.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT can produce detailed cross-sectional images of the retina and optic nerve head. It aids in the early detection of glaucoma by measuring the thickness of the retinal nerve fiber layer and ganglion cell complex.
- Confocal Scanning Laser Ophthalmoscopy: This imaging technique examines the optic nerve head and retinal nerve fiber layer, providing quantitative data that can aid in the monitoring of changes over time.
- Retinal Photography: Taking high-resolution photographs of the retina can help document the appearance of the optic nerve head and surrounding retinal structures. This is useful for monitoring changes over time and detecting early signs of glaucoma.
Functional Tests
- Visual Field Testing: Also called perimetry, this test assesses the entire field of vision. It can detect subtle vision changes and blind spots that may indicate optic nerve damage. Automated visual field tests, such as the Humphrey Field Analyzer, are popular.
- Electrophysiological Tests: Tests such as pattern electroretinography (PERG) and visual evoked potentials (VEP) can evaluate the function of the retinal ganglion cells and optic nerve, providing additional information about the visual pathway’s health.
Blood Flow Analysis
- Doppler Ultrasonography: This technique measures blood flow in the ocular vessels, which aids in determining the vascular component of ocular hypertension and its potential effect on the optic nerve.
- Laser Doppler Flowmetry: This method assesses microcirculation in the optic nerve head, providing information about the vascular health of the eye.
Ocular Hypertension Treatment
Medical Management
- Topical Medications: The first line of treatment for ocular hypertension is usually topical eye drops that reduce intraocular pressure (IOP). These medications include:
- Prostaglandin Analogues: Drugs such as latanoprost, bimatoprost, and travoprost increase the flow of aqueous humor, effectively lowering IOP.
- Beta-blockers: Timolol and betaxolol inhibit the production of aqueous humor.
- Alpha Agonists: Brimonidine and apraclonidine reduce aqueous humor production while increasing outflow.
- Carbonic Anhydrase Inhibitors: Dorzolamide and brinzolamide lower aqueous humor production.
- Rho Kinase Inhibitors: Netarsudil promotes aqueous humor outflow via the trabecular meshwork.
- Oral Medications: When topical medications are insufficient, oral carbonic anhydrase inhibitors such as acetazolamide can be used to lower IOP even further.
Laser Treatments
- Laser Trabeculoplasty: This procedure employs a laser to improve drainage through the trabecular meshwork. Types include:
- Argon Laser Trabeculoplasty (ALT): Creates microscopic burns in the trabecular meshwork to improve fluid outflow.
- Selective Laser Trabeculoplasty (SLT): Uses a lower-energy laser to target pigmented cells in the trabecular meshwork, reducing side effects and tissue damage.
- Laser Iridotomy: This procedure, which is most commonly used for angle-closure glaucoma, creates a small hole in the iris to improve fluid drainage.
Surgical Treatments
- Trabeculectomy: This surgical procedure creates a new drainage pathway for aqueous humor to exit the eye, which lowers IOP. It is usually reserved for situations where medications and laser treatments are ineffective.
- Glaucoma Drainage Devices: Implants such as the Ahmed, Baerveldt, or Molteno valves can be used to regulate aqueous humor outflow and IOP.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures are less invasive than traditional surgeries, resulting in fewer complications and shorter recovery times. Examples include the iStent, Hydrus Microstent, and Xen Gel Stent.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy seeks to correct genetic factors that contribute to ocular hypertension and glaucoma. Early research focuses on modifying genes that regulate aqueous humor production and outflow.
- Neuroprotective Agents: These medications aim to protect the optic nerve from damage regardless of IOP levels. Agents that can provide additional protection to optic nerve cells are currently under investigation.
- Cannabinoid-Based Therapies: Researchers are looking into the potential of cannabinoids to lower IOP. While some preliminary findings are promising, more research is required to determine their efficacy and safety.
- Novel Drug Delivery Systems: Advances in drug delivery, such as sustained-release implants and nanoparticles, aim to improve medication adherence and efficacy by delivering IOP-lowering drugs consistently and over time.
Monitoring and Follow-up
Regular follow-up appointments are critical for monitoring IOP, assessing treatment effectiveness, and making necessary adjustments to the treatment plan. Comprehensive eye exams, which include visual field testing and optic nerve imaging, aid in disease progression and prevention.
Effective Ways to Improve and Prevent Ocular Hypertension
- Regular Eye Exams: Get routine eye exams, especially if you have risk factors for ocular hypertension. Early detection is critical to avoiding complications.
- Maintain a Healthy Diet: A diet high in antioxidants like vitamins A, C, and E can benefit overall eye health. Include plenty of green leafy vegetables, fruits, and omega-3-rich fish.
- Exercise Regularly: Regular physical activity can improve overall health and possibly lower IOP. Aerobic activities such as walking, swimming, and cycling are beneficial.
- Monitor Medication Use: Be aware that certain medications, such as corticosteroids, can raise IOP. If necessary, discuss alternative treatments with your healthcare provider.
- Control Systemic Conditions: Manage conditions such as diabetes and hypertension, both of which can have an impact on eye health and contribute to ocular hypertension.
- Avoid Excessive Caffeine: Excess caffeine consumption can temporarily raise IOP. To avoid eye pressure spikes, use moderation.
- Stay Hydrated: Adequate hydration promotes overall health, including eye health. Drink plenty of water during the day.
- Protect Your Eyes: Wear protective eyewear to avoid trauma that could cause elevated IOP.
- Avoid Smoking: Smoking is bad for your overall health and can worsen eye conditions. Quitting smoking can improve your overall health and lower your risk of ocular hypertension.
- Follow Treatment Plans: If you have ocular hypertension, strictly adhere to the prescribed treatments and attend all follow-up appointments to monitor your condition and adjust treatments as needed.
Trusted Resources
Books
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care” by Paul N. Schacknow and John R. Samples
- “Ophthalmology” by Myron Yanoff and Jay S. Duker
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
Online Resources
- American Academy of Ophthalmology: AAO.org
- National Eye Institute: NEI.nih.gov
- Glaucoma Research Foundation: Glaucoma.org
- Mayo Clinic: MayoClinic.org
- All About Vision: AllAboutVision.com
- MedlinePlus: MedlinePlus.gov
- American Glaucoma Society: AmericanGlaucomaSociety.net
- PubMed: PubMed.gov






