What is Optical Disc Coloboma?
Optic disc coloboma is a congenital eye condition defined by an abnormality or defect in the optic disc, which is where the optic nerve enters the retina. This defect results from incomplete closure of the embryonic fissure during early fetal development. Optic disc colobomas can cause vision problems ranging from mild to severe, depending on their size and location. This condition can occur alone or as part of a syndrome that includes other ocular or systemic abnormalities.
Detailed Exploration of Optic Disc Coloboma
Anatomy and Development
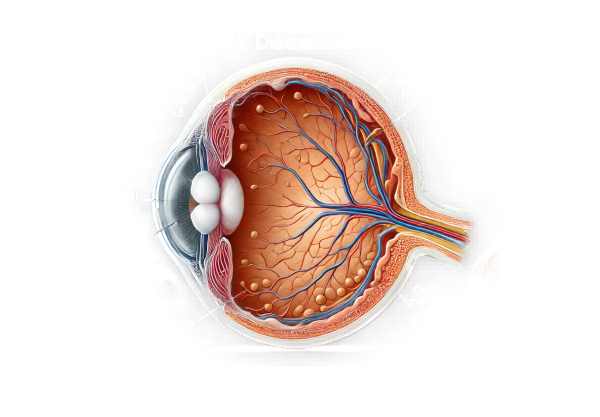
The optic disc, also known as the optic nerve head, is the area where the retinal nerve fibers meet to form the optic nerve, which transmits visual information from the retina to the brain. During normal fetal development, the embryonic fissure, a groove in the optic vesicle, closes, forming the optic cup and other eye structures. When this closure is incomplete, it causes a coloboma, which is a gap or defect in the eye structure.
Causes and Genetics
Optic disc coloboma is primarily a congenital condition, meaning it is present from birth. The exact cause of the embryonic fissure’s failure to close is not always known, but it is frequently associated with genetic factors. PAX6, SHH, and CHD7 gene mutations have all been linked to the development of colobomas. These genes are critical for eye development and the formation of ocular structures. In some cases, optic disc coloboma is associated with a syndrome, such as CHARGE syndrome, which includes a number of developmental abnormalities.
Clinical Presentation
The clinical presentation of optic disc coloboma varies greatly depending on the size of the defect. The key features include:
- Visual Impairment: The degree of vision loss varies from mild to severe. Some people may have normal vision, while others may have significant visual impairments.
- Characteristic Appearance. On ophthalmoscopic examination, the optic disc appears abnormal, with a distinct excavation or pit, also known as a “morning glory” anomaly due to its resemblance to the flower.
- Associated Ocular Anomalies Optic disc coloboma may be associated with other ocular abnormalities such as retinal detachment, microphthalmia (abnormally small eyes), or cataracts.
- Systemic Associations: When part of a syndrome, optic disc coloboma may be associated with systemic abnormalities such as heart defects, ear abnormalities, and developmental delays.
Pathophysiology
The pathophysiology of optic disc coloboma includes disruption of normal embryonic development. During early gestation, the optic vesicle invaginates to form the optic cup, and the embryonic fissure must close for the eye structures to form properly. If this fissure does not close properly, a coloboma develops, which can affect the optic disc, retina, choroid, or iris.
Complications
Optic disc coloboma can cause a variety of complications, some of which have a significant impact on vision.
- Retinal Detachment:** One of the most serious complications is retinal detachment, which occurs when the retina separates from the underlying tissue, resulting in sudden vision loss if not treated immediately.
- Maculopathy: Involvement of the macula, the central part of the retina responsible for detailed vision, can cause severe visual impairment.
- Glaucoma. The abnormal structure of the optic disc increases the risk of developing glaucoma, a condition marked by increased intraocular pressure and optic nerve damage.
- Amblyopia: Amblyopia, also known as “lazy eye,” occurs when one eye is significantly more affected than the other, resulting in impaired vision development in the affected eye.
Differential Diagnosis
Several other conditions can present with similar symptoms and should be considered during diagnosis:
- Morning Glory Syndrome: This condition appears to be a similar optic disc anomaly but has distinct features such as a funnel-shaped excavation and surrounding choroidal pigmentation.
- Optic Nerve Pit: A small, round depression on the optic disc that may indicate serous retinal detachment.
- Congenital Optic Nerve Hypoplasia is characterized by a smaller-than-normal optic disc and fewer optic nerve fibers, resulting in vision impairment.
Prognosis
Individuals with optic disc coloboma have a different prognosis depending on the severity of the defect and the presence of associated complications. Regular monitoring and early treatment of complications can help to preserve vision and improve outcomes.
Methods to Diagnose Optic Disc Coloboma
Optic disc coloboma is diagnosed using a combination of clinical examination, imaging studies, and, in some cases, genetic testing to confirm the diagnosis and determine the severity of the condition.
Clinical Examination
- ophthalmoscopy: This is the primary diagnostic tool for optic disc colobomas. During an ophthalmoscopic examination, the ophthalmologist looks for distinguishing features like a large, excavated disc with an abnormal appearance, also known as a “morning glory” anomaly.
- visual acuity test: The assessment of visual acuity aids in determining the coloboma’s effect on vision. This test assesses vision clarity and sharpness, providing useful information about the condition’s functional consequences.
- Refraction Test: This test detects refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism, which may be associated with optic disc coloboma.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic disc. It is useful in determining the structure of the optic nerve head, the size of the coloboma, and any other retinal abnormalities.
2) Fundus Photography: This imaging method takes detailed photographs of the eye’s interior surface, including the retina, optic disc, and macula. Fundus photography helps to document the appearance of the coloboma and track changes over time.
- Ultrasonography: B-scan ultrasonography is useful for evaluating the posterior segment of the eye, especially when media opacities obscure the view or there is retinal detachment. It aids in determining the extent of the coloboma and detecting associated complications.
Genetic Testing
When optic disc coloboma is suspected to be part of a genetic syndrome, genetic testing can be used to identify mutations in genes known to cause coloboma formation, such as PAX6, SHH, and CHD7. Affected families may also benefit from genetic counseling.
Treatment Options for Optic Disc Coloboma
Management of Vision Impairment
The primary goal of treating optic disc coloboma is to alleviate symptoms and avoid complications. Because the structural defect cannot be repaired, treatment focuses on improving the patient’s visual function and addressing underlying ocular conditions.
- Corrective Lenses:** Patients with refractive errors like myopia, hyperopia, or astigmatism can benefit from prescription glasses or contact lenses to improve their visual acuity. Regular eye exams are essential for adjusting prescriptions as needed.
- Low-Vision Aids: Patients with severe vision loss may benefit from low vision aids like magnifying glasses, specialized reading devices, and electronic visual aids. Vision rehabilitation programs can teach people how to use these aids effectively.
Management of Complications
- Retinal Detachment:** Retinal detachment is a serious complication of optic disc coloboma. To reattach the retina and prevent permanent vision loss, a surgical procedure such as scleral buckle surgery or vitrectomy may be required. Early detection and treatment are critical for successful outcomes.
2) Glaucoma: Patients with optic disc coloboma have a higher risk of developing glaucoma due to the abnormal optic disc structure. Regular monitoring of intraocular pressure (IOP) is required. If glaucoma is discovered, treatment options include medications (e.g., prostaglandin analogs, beta-blockers) to reduce IOP, laser therapy (e.g., trabeculoplasty), or surgical procedures (e.g., trabeculectomy) to improve aqueous humor drainage.
- Amblyopia: Amblyopia, also known as “lazy eye,” occurs when one eye is significantly more affected than the other. Treatment options may include patching the stronger eye to encourage use of the weaker eye, vision therapy exercises, or atropine eye drops to temporarily blur vision in the stronger eye.
Innovative and Emerging Therapies
- Gene Therapy: Studies into gene therapy for congenital eye disorders are ongoing. Although not yet widely available, gene therapy shows promise for correcting the genetic mutations that cause colobomas. Early trials have shown promise in treating other genetic ocular conditions, pointing to a future role for this approach in managing optic disc coloboma.
- stem cell therapy: Stem cell therapy is being investigated as a possible treatment for a wide range of ocular conditions, including optic nerve damage. While still in experimental stages, this approach aims to regenerate damaged optic nerve cells and restore some vision.
- Neuroprotective Agents: Current research focuses on developing neuroprotective drugs to protect optic nerve cells from further damage. These agents may help to slow the progression of vision loss in patients with optic disc coloboma.
Regular Monitoring and Follow-up
Patients with optic disc coloboma should see an ophthalmologist on a regular basis to monitor their condition and manage any complications that arise. This includes regular comprehensive eye exams, visual field testing, OCT imaging, and intraocular pressure readings. Early detection and treatment of associated complications can greatly improve long-term outcomes.
Effective Ways to Improve and Prevent Optic Disc Coloboma
- Genetic Counseling: – Families with a history of optic disc coloboma or related genetic conditions should seek genetic counseling to assess their risk and potential transmission to offspring.
- Prenatal Care: – Receiving proper prenatal care and avoiding teratogens during pregnancy can lower the risk of congenital anomalies like optic disc coloboma.
- Regular eye exams for children, especially those with a family history of ocular conditions, can aid in early detection and management of colobomas and related vision issues.
- Monitoring for Complications: Regular monitoring for potential complications like glaucoma and retinal detachment is essential. Early intervention can prevent or reduce vision loss.
- Protective Eyewear: – Wearing protective eyewear during high-risk activities can prevent trauma and exacerbate ocular conditions.
- Vision Therapy: – Vision therapy and visual aids can enhance visual function and quality of life for people with optic disc coloboma.
- Maintaining a healthy lifestyle, including a balanced diet with vitamins and minerals, can improve eye health and lower the risk of secondary complications.
- Awareness and Education: – Educating patients and families about optic disc coloboma, potential complications, and the need for regular eye care is crucial for effective management.
- Avoid smoking and alcohol during pregnancy to reduce the risk of congenital anomalies in the developing fetus.
Trusted Resources
Books
- “Genetics for Ophthalmologists: The Molecular Genetic Basis of Ophthalmic Disorders” by Graeme C. M. Black
- “Pediatric Ophthalmology: Current Thought and A Practical Guide” by Edward M. Wilson, Richard Saunders, and Trivedi Rupal
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling










