Corneal abrasions are among the most common ocular injuries, characterized by a scratch or scrape on the transparent front surface of the eye. Even minor abrasions can cause significant discomfort, tearing, light sensitivity, and temporary vision changes. While most cases heal rapidly with appropriate care, prompt recognition and proper management are essential to prevent complications such as infection or scarring. This in-depth guide covers the latest evidence-based treatments, surgical interventions for complex cases, and promising new innovations in corneal abrasion care, empowering patients and families to make informed choices for optimal eye health and recovery.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
- Disclaimer
Condition Overview and Epidemiology
Definition and Mechanism
A corneal abrasion refers to a superficial injury to the corneal epithelium, the outermost layer of the eye. It most commonly results from trauma—such as a fingernail, makeup brush, tree branch, or contact lens misuse—but can also be caused by foreign bodies, chemical exposure, or dry eyes.
Pathophysiology
The cornea is richly innervated, so even tiny abrasions can be intensely painful. Loss of the epithelial barrier increases vulnerability to infection and inflammation, emphasizing the need for swift treatment.
Prevalence and Risk Factors
- Corneal abrasions are a leading reason for emergency eye visits worldwide.
- Particularly common among children, athletes, contact lens wearers, and people with occupational exposure to dust or debris.
- Other risk factors: dry eye syndrome, ocular surface disease, recent eye surgery, and poorly fitting contact lenses.
Symptoms
- Sudden onset eye pain, foreign body sensation, tearing
- Light sensitivity (photophobia)
- Redness and blurred vision
- Excessive blinking or inability to open the eye
Complications
- Bacterial keratitis (corneal infection)
- Scarring, recurrent erosions, or vision loss if not properly treated
Practical Advice:
If you suspect a corneal abrasion, avoid rubbing your eye, do not attempt to remove an embedded object yourself, and seek prompt medical evaluation.
Conventional and Pharmacological Therapies
Most corneal abrasions heal within 24–72 hours with proper medical management. Early intervention minimizes complications and optimizes comfort.
1. Immediate First Aid and Home Care
- Irrigation: Rinse the eye with sterile saline or clean water to remove loose debris.
- Do not patch the eye without medical advice, as this may delay healing.
2. Topical Medications
- Antibiotic eye drops or ointments are standard to prevent bacterial infection. Common choices include erythromycin ointment, polymyxin B/trimethoprim drops, or fluoroquinolone drops for contact lens users.
- Lubricating artificial tears reduce irritation and support healing.
- Cycloplegic drops (like cyclopentolate) may be prescribed for severe pain by relaxing the ciliary muscle.
3. Pain Management
- Oral analgesics (acetaminophen, ibuprofen) for discomfort.
- Topical anesthetic drops are never prescribed for home use, as they can delay healing and cause serious corneal toxicity.
- Cold compresses may offer symptom relief.
4. Protective Measures
- Avoid contact lens use until the eye is fully healed and cleared by a professional.
- Wear sunglasses outdoors to reduce light sensitivity.
5. Follow-Up
- Re-examination within 24–48 hours is recommended to confirm healing and rule out infection or retained foreign bodies.
6. Special Cases
- Contact lens-related abrasions: Require antibiotics effective against Pseudomonas (e.g., ciprofloxacin).
- Recurrent corneal erosion syndrome: May need extended use of lubricants or specialized therapy.
Practical Advice:
Never use “red eye” drops or borrow someone else’s medication. Complete the full course of prescribed antibiotics, even if symptoms improve quickly.
Surgical and Interventional Procedures
Although most corneal abrasions heal without surgery, certain cases require more advanced intervention.
Indications for Advanced Treatment
- Large, deep, or non-healing abrasions
- Foreign bodies embedded in the cornea
- Suspected corneal laceration or perforation
- Recurrent corneal erosion syndrome
Key Procedures and Techniques
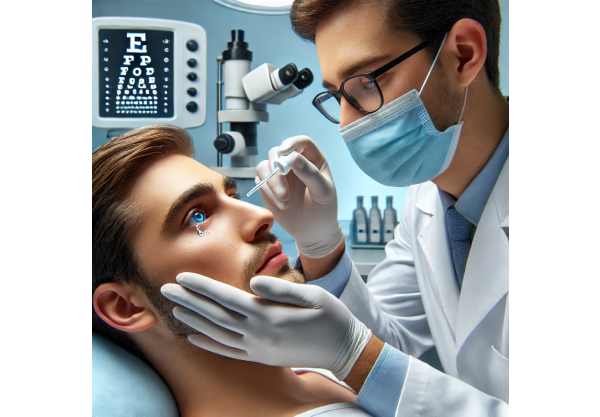
- Foreign Body Removal
- Performed with specialized instruments under topical anesthesia.
- Metallic foreign bodies may leave a “rust ring” that requires removal with an ophthalmic burr.
- Bandage Contact Lenses
- Soft, sterile lenses protect the corneal surface and relieve pain, especially in recurrent erosions or after surgical removal of a foreign body.
- Amniotic Membrane Transplantation
- Biological graft used in non-healing abrasions to promote healing and reduce inflammation.
- Corneal Debridement
- Removal of loose or irregular epithelium to encourage healthy regrowth in chronic or recurrent erosions.
- Suturing or Surgical Repair
- Rarely, deep wounds or lacerations may need surgical closure and repair.
- Adjunctive Measures
- Autologous serum eye drops, rich in growth factors, for persistent defects.
- Oral doxycycline or topical corticosteroids (with close supervision) may be used for chronic inflammation or non-healing cases.
Risks and Recovery
- Procedures are generally safe but carry small risks of infection, delayed healing, or scarring.
- Follow all post-procedure instructions for best outcomes.
Practical Advice:
If symptoms worsen, vision declines, or you notice pus or excessive redness, contact your eye doctor immediately as these may signal infection or more severe injury.
Emerging Innovations and Advanced Technologies
Advances in corneal abrasion care continue to improve healing, comfort, and patient outcomes. Recent innovations blend biotechnology, digital health, and personalized approaches.
1. Regenerative Therapies
- Growth factor–enriched eye drops: Biologic or stem-cell derived drops accelerate healing in persistent abrasions.
- Amniotic membrane devices: Single-use contact lenses infused with amniotic tissue are now available for office-based use.
2. Nanotechnology-Based Eye Drops
- Nano-carriers for antibiotics or lubricants provide longer-lasting relief and targeted drug delivery.
3. Smart Bandage Lenses
- Next-generation lenses release medications or healing agents directly onto the cornea, minimizing the need for frequent drops.
4. Point-of-Care Diagnostics
- Rapid, portable testing for infectious agents helps tailor antibiotic therapy for complex or non-healing abrasions.
5. Teleophthalmology and Remote Monitoring
- Digital platforms allow patients to share images or videos with specialists, ensuring early identification of complications or the need for urgent care.
6. Artificial Intelligence (AI) for Triage
- AI-based tools in emergency and urgent care settings help triage eye injuries and identify patients at risk for complications.
7. Personalized Care Algorithms
- Data-driven risk models optimize treatment plans based on age, health status, abrasion size, and healing speed.
Practical Advice:
Ask your provider about the availability of novel therapies or digital follow-up options, especially if you have a history of slow healing or recurrent abrasions.
Clinical Trials and Future Directions
The field of corneal injury management is advancing through robust research aimed at better therapies, faster recovery, and complication prevention.
Current Research and Key Focus Areas
- New Antibiotic Formulations:
- Trials on slow-release, broad-spectrum eye drops to reduce dosing frequency and resistance.
- Biologic and Stem Cell Therapies:
- Clinical trials on amniotic membrane–based and stem cell–derived treatments for persistent or severe abrasions.
- Innovative Drug Delivery Devices:
- Investigating smart contact lenses that can deliver medications or healing factors on a programmed schedule.
- Digital Health and AI Applications:
- Studies on the effectiveness of telehealth, smartphone apps for symptom tracking, and AI-based diagnostic support.
- Personalized Risk Prediction:
- Machine learning models to predict which patients are most at risk for complications or recurrent erosions.
- Preventive Strategies in At-Risk Groups:
- Evaluating new approaches to protect high-risk populations (contact lens users, athletes, industrial workers).
How to Participate in Research
Patients with persistent or recurrent abrasions may be eligible for studies evaluating new therapies. Talk to your eye care provider or check clinicaltrials.gov for opportunities.
Practical Advice:
Participation in clinical trials not only gives access to cutting-edge care but also helps improve outcomes for others facing similar challenges in the future.
Frequently Asked Questions
What is a corneal abrasion and how is it caused?
A corneal abrasion is a scratch or scrape on the eye’s clear surface, usually from trauma like fingernails, dust, or contact lenses. It causes pain, tearing, and light sensitivity.
How is a corneal abrasion treated?
Most heal with antibiotic eye drops or ointments to prevent infection, lubricating drops for comfort, and avoidance of contact lenses until fully healed. Severe cases may require advanced interventions.
How long does it take for a corneal abrasion to heal?
Small abrasions typically heal within 24 to 72 hours, while larger or complicated injuries may take longer and require close follow-up.
When should I see a doctor for a corneal abrasion?
Seek care if you have severe pain, vision loss, signs of infection (pus, redness), or if the injury was caused by chemicals or a foreign object that cannot be removed easily.
Can I wear contact lenses with a corneal abrasion?
No, contact lenses should not be worn until your eye doctor confirms full healing. Wearing them too soon increases the risk of infection and complications.
Are there any complications of corneal abrasions?
Yes, complications can include infection (keratitis), scarring, recurrent erosions, and, rarely, permanent vision loss if not properly managed.
What should I avoid after a corneal abrasion?
Avoid rubbing your eye, using non-prescribed drops, or wearing contacts until healed. Protect your eye from further injury and follow your doctor’s instructions.
Disclaimer
The information in this article is for educational purposes only and should not replace professional medical advice, diagnosis, or treatment. Always consult your eye care provider for guidance specific to your condition.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or any platform you prefer. Your support helps our team continue providing reliable health information to the community!