Eales disease is a rare, vision-threatening retinal disorder characterized by inflammation, occlusion, and abnormal growth of blood vessels in the retina. Predominantly affecting healthy young adults—most commonly males aged 20 to 40—Eales disease can result in sudden vision loss due to recurrent vitreous hemorrhages. With its multifactorial origins and a clinical course that can range from mild to severe, early diagnosis and a comprehensive, personalized management plan are vital. This detailed guide explores the latest understanding of Eales disease, covering classic and emerging therapies, surgical strategies, and future directions in care to empower patients and providers.
Table of Contents
- Understanding Eales Disease: Patterns and Epidemiology
- Medical Management and Pharmacologic Options
- Interventional and Surgical Solutions for Advanced Cases
- Novel Therapies and Technological Advancements
- Research Frontiers and Upcoming Clinical Trials
- Frequently Asked Questions
Understanding Eales Disease: Patterns and Epidemiology
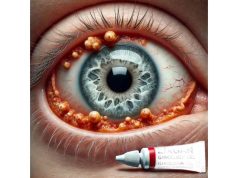
Eales disease is an idiopathic obliterative vasculopathy primarily affecting the peripheral retina. The disorder progresses through stages of venous inflammation (periphlebitis), vascular occlusion, and subsequent neovascularization, culminating in vision loss from retinal hemorrhage or tractional retinal detachment.
Key Features:
- Chronic, recurrent retinal vein inflammation (periphlebitis)
- Ischemia-induced retinal neovascularization
- Predilection for healthy, young, adult males (20-40 years)
- Recurrent or sudden painless visual loss due to vitreous hemorrhage
Epidemiology:
- Most common in South Asian populations, particularly India, but seen worldwide
- Male predominance (up to 85% of cases)
- Accounts for a significant proportion of non-diabetic retinal vasculitis in endemic regions
Etiology and Pathophysiology:
- Exact cause remains unclear; considered idiopathic, though immune-mediated mechanisms are implicated
- Proposed association with tuberculosis (latent or active), Mycobacterium tuberculosis DNA found in some retinal samples
- Other triggers: systemic inflammation, hypersensitivity to tuberculin protein, and environmental exposures
Risk Factors:
- Young age (peak in 20s–30s)
- Male gender
- South Asian ethnicity
- Possible underlying or latent tuberculosis infection
Clinical Course:
- Early stage: Periphlebitis (inflammation and sheathing of peripheral retinal veins)
- Occlusive stage: Vascular non-perfusion, ischemia
- Proliferative stage: Neovascularization and recurrent hemorrhage
- Late stage: Tractional retinal detachment, neovascular glaucoma
Diagnosis:
- Based on clinical history, examination, and characteristic fundus findings
- Fluorescein angiography reveals areas of non-perfusion, neovascularization, and leakage
- Laboratory workup to exclude other causes (sarcoidosis, lupus, Behçet’s disease)
- Chest X-ray and TB testing to assess for latent or active tuberculosis
Practical Advice:
If you notice sudden floaters, loss of vision, or visual field defects—especially if you are a young adult—seek urgent ophthalmic evaluation. Timely diagnosis is critical to prevent irreversible damage.
Medical Management and Pharmacologic Options
The foundation of Eales disease management begins with controlling retinal inflammation and preventing neovascular complications. Therapy is typically personalized based on disease stage and severity.
1. Corticosteroids
- Oral, periocular, or intravitreal corticosteroids are mainstays for acute inflammation and retinal vasculitis.
- Oral prednisone is commonly used for active periphlebitis.
- Periocular injections (e.g., triamcinolone) offer localized treatment with fewer systemic side effects.
- Intravitreal steroids can be considered for persistent macular edema or inflammation.
2. Anti-Tuberculosis Therapy (ATT)
- In regions with high TB prevalence or evidence of latent/active tuberculosis, anti-tubercular therapy is essential.
- ATT is administered in addition to corticosteroids if TB is suspected or confirmed.
3. Immunosuppressive Agents
- For corticosteroid-dependent or refractory cases, immunosuppressives like methotrexate, azathioprine, or mycophenolate mofetil may be used.
- Biologic agents (anti-TNF drugs) are being explored for select severe cases.
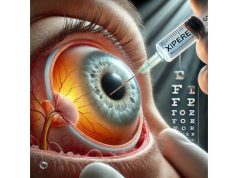
4. Anti-VEGF Injections
- Vascular endothelial growth factor (VEGF) inhibitors (e.g., bevacizumab, ranibizumab) are injected into the eye to control neovascularization and prevent or treat macular edema.
- Often combined with laser therapy in the proliferative stage.
5. Laser Photocoagulation
- Panretinal photocoagulation (PRP) to ischemic retinal areas reduces the stimulus for new vessel formation.
- Laser is highly effective in stabilizing the proliferative phase.
6. Supportive Therapies
- Oral vitamins and antioxidants may support retinal health but are not substitutes for primary therapy.
- Regular monitoring and follow-up exams are crucial.
Medication Keywords Integrated:
- corticosteroids for Eales disease
- anti-tubercular therapy for retinal vasculitis
- anti-VEGF injections for proliferative retinopathy
- immunosuppressants for retinal vasculitis
Practical Advice:
Follow your prescribed treatment plan closely and attend all follow-up appointments. Early and consistent therapy offers the best chance for preserving vision.
Interventional and Surgical Solutions for Advanced Cases
While many patients with Eales disease respond to medical management, those with persistent or advanced disease often require interventional procedures or surgery to restore or preserve vision.
1. Laser Photocoagulation
- Essential in the proliferative stage; PRP targets non-perfused retina to regress neovascularization.
- Can be performed as an outpatient procedure under topical anesthesia.
2. Intravitreal Injections
- Anti-VEGF agents and corticosteroids delivered directly into the vitreous cavity target macular edema and abnormal vessel growth.
- May require repeat treatments for sustained effect.
3. Pars Plana Vitrectomy
- Indicated for non-resolving vitreous hemorrhage, tractional retinal detachment, or epiretinal membrane formation.
- Modern microincision vitrectomy techniques enable quicker recovery and better outcomes.
- May be combined with endolaser therapy during the procedure.
4. Management of Complications
- Tractional or rhegmatogenous retinal detachments require surgical repair, often with vitrectomy and possible scleral buckle placement.
- Neovascular glaucoma is managed with anti-VEGF injections, laser, and glaucoma surgery if needed.
5. Adjunct Procedures
- Subtenon or intravitreal steroid injections for persistent inflammation
- Retinal cryotherapy or diathermy (rarely used, for select cases)
Surgical Keywords Integrated:
- vitrectomy for Eales disease
- panretinal photocoagulation for proliferative retinopathy
- management of retinal detachment in Eales disease
- intravitreal steroids for refractory retinal vasculitis
Practical Advice:
Surgical treatment is most successful when performed before extensive retinal damage occurs. If you experience sudden vision loss, floaters, or shadows, seek prompt surgical evaluation.
Novel Therapies and Technological Advancements
In the last few years, research into Eales disease and retinal vasculitis has led to promising new therapies and diagnostic approaches.
1. Biologic Agents
- Targeted monoclonal antibodies (e.g., anti-TNF agents like adalimumab, infliximab) for patients unresponsive to conventional immunosuppression.
- Case reports show promise in controlling aggressive inflammation and reducing recurrence.
2. Gene and Cell Therapy
- Gene editing and cell-based approaches for vascular repair and modulating immune response are under preclinical investigation.
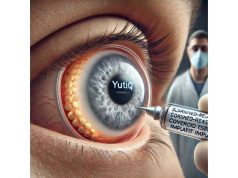
3. Long-Acting Drug Delivery Systems
- Extended-release intravitreal implants for corticosteroids and anti-VEGF agents reduce the need for frequent injections.
- Devices such as the dexamethasone implant offer sustained effect.
4. AI-Based Diagnostics and Digital Monitoring
- Artificial intelligence for fundus image analysis enhances early detection and monitoring of neovascular changes.
- Remote retinal imaging and tele-ophthalmology platforms allow for more accessible ongoing care.
5. Laser Innovations
- Pattern scanning laser photocoagulation and subthreshold laser offer precise, less damaging treatments.
- Navigated laser systems enable highly targeted therapy with improved safety.
6. Advanced Imaging Techniques
- Optical coherence tomography angiography (OCTA) allows for detailed, noninvasive visualization of retinal vasculature.
- Fluorescein angiography innovations aid in monitoring treatment response.
Innovation Keywords Integrated:
- AI diagnostics for retinal vasculitis
- gene therapy for retinal disease
- long-acting intravitreal implants for Eales disease
- advanced laser treatments for retinal neovascularization
Practical Advice:
Stay informed about clinical trial opportunities, and ask your specialist about access to the latest technologies. Personalized care is the future for complex retinal diseases like Eales.
Research Frontiers and Upcoming Clinical Trials
The field of retinal vasculitis is evolving, and ongoing research continues to improve outcomes for Eales disease. Clinical trials and new research initiatives are paving the way for more effective and less invasive treatments.
1. Novel Anti-Inflammatory Agents
- New small molecules and biologics targeting specific immune pathways are under clinical investigation.
- Potential for fewer side effects and more tailored therapy.
2. Regenerative Medicine
- Stem cell–based therapies for repairing retinal vasculature and supporting neural survival are advancing in early-phase trials.
3. Personalized Immunosuppression
- Genetic and biomarker-guided approaches may help identify patients most likely to respond to targeted therapies, minimizing unnecessary side effects.
4. Digital and Home-Based Monitoring
- Smartphone-enabled retinal imaging and remote patient monitoring are being tested to improve early detection of recurrences and optimize follow-up.
5. Multicenter Clinical Trials
- International collaboration is expanding the pool of research subjects, helping accelerate the discovery of new treatments.
Current and Future Directions:
- Early identification of high-risk patients using advanced imaging and biomarkers
- Integration of telemedicine for better access and continuity of care
- Expanding awareness among non-ophthalmic providers for timely referral
Research Keywords Integrated:
- clinical trials for Eales disease
- regenerative medicine for retinal vasculitis
- future therapies for retinal neovascularization
- remote monitoring for vision disorders
Practical Advice:
If you are interested in participating in research, consult your ophthalmologist or visit clinical trial registries online. Participation can offer access to cutting-edge care and contribute to scientific advancement.
Frequently Asked Questions
What is Eales disease?
Eales disease is a rare inflammatory retinal vasculitis that leads to blood vessel blockage, abnormal vessel growth, and potential vision loss, usually in young adults.
How is Eales disease diagnosed?
Diagnosis relies on clinical eye examination, fundus imaging, fluorescein angiography, and ruling out other causes of retinal vasculitis or infectious disease.
What are the treatment options for Eales disease?
Treatment includes corticosteroids, laser therapy, anti-VEGF injections, immunosuppressants, and in advanced cases, retinal surgery like vitrectomy.
Can Eales disease cause permanent vision loss?
Yes, if not managed promptly, recurrent hemorrhages and retinal detachment can result in irreversible vision loss, emphasizing the importance of early intervention.
Is there a cure for Eales disease?
There is no known cure, but proper medical and surgical management can control inflammation, prevent complications, and preserve vision for many patients.
What is the link between Eales disease and tuberculosis?
Eales disease has a strong association with latent or active tuberculosis, especially in endemic regions. Anti-tuberculosis therapy is recommended if TB is confirmed.
Disclaimer:
This article is for informational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions about your health or vision.
If you found this article useful, please share it on Facebook, X (formerly Twitter), or any platform you like. Follow us on social media and support our work by sharing to help others stay informed and healthy.