What is a Penetrating Eye Injury?
A penetrating eye injury is a severe type of ocular trauma in which an object pierces the cornea or sclera and enters the eye’s internal structures. This type of injury can cause significant damage to the eye, potentially leading to vision loss or blindness if not treated promptly and appropriately. Penetrating eye injuries are medical emergencies that require immediate attention from an ophthalmologist or emergency medical personnel in order to prevent complications and preserve vision.
Causes and Risk Factors
Penetrating eye injuries can occur from a variety of sources, including sharp objects or high-velocity projectiles. Common causes include:
Accidents and Falls: Falls or accidents involving sharp objects such as knives, scissors, or tools can result in penetrating eye injuries for both children and adults.
Workplace Incidents: People who work in construction, manufacturing, or other industries where they may come into contact with sharp or fast-moving objects are more vulnerable. Safety protocols and protective eyewear are essential in these environments.
Sports and Recreational Activities: Without proper protective equipment, activities like archery, airsoft, paintball, and certain contact sports can result in penetrating eye injuries.
Assaults: Physical fights with weapons or sharp objects can cause serious ocular trauma, including penetrating injuries.
Household Accidents: Common household items such as gardening tools, kitchen utensils, and even broken glass can result in penetrating eye injuries.
Pathophysiology
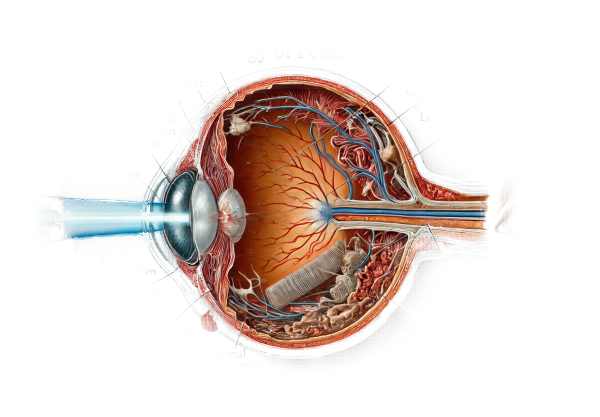
The pathophysiology of penetrating eye injuries involves direct mechanical disruption of ocular structures, which can result in a variety of complications depending on the severity of the injury and its location. When an object enters the eye, it may cause:
Corneal and Scleral Lacerations: A penetrating object can cut through the cornea or sclera, compromising eye integrity and allowing pathogens to enter, resulting in infection.
Intraocular Damage: The object may injure intraocular structures such as the lens, iris, retina, or optic nerve, causing vision loss. The size, speed, and trajectory of the object determine the extent of the damage.
Hemorrhage: Penetrating injuries can result in internal bleeding of the eye, such as hyphema (blood in the anterior chamber) or vitreous hemorrhage, which can impair vision and complicate treatment.
Inflammation and Infection: The introduction of foreign material and bacteria can cause serious inflammation and infection, such as endophthalmitis, necessitating immediate medical attention.
Symptoms
The symptoms of penetrating eye injuries can vary greatly depending on the type and severity of the injury. Common symptoms include:
Severe Pain: Penetrating eye injuries frequently cause excruciating pain due to the disruption of sensitive ocular tissues and nerves.
Vision Loss: Depending on the structures involved, partial or complete vision loss may occur immediately after the injury. It is common to experience blurred vision, double vision, or loss of specific visual fields.
Visible Foreign Body: A foreign object protruding from the eye or embedded in ocular structures indicates a penetrating injury.
Bleeding: External bleeding from the eye or blood pooling within the eye (hyphema) may be visible.
Photophobia: Because of the damage and inflammation caused by a penetrating eye injury, there is often an increase in light sensitivity.
Swelling and Redness: Trauma and subsequent inflammation can cause the eye and surrounding tissues to swell and turn red.
Complications
Penetrating eye injuries can result in a variety of complications, some of which may have long-term effects on vision and ocular health. The complications include:
Infection: One of the most serious complications of penetrating eye injuries is infection, such as endophthalmitis, which can quickly progress and result in severe vision loss or loss of the eye if not treated immediately.
Retinal Detachment: Trauma from a penetrating injury can cause the retina to separate from the underlying supportive tissues, resulting in severe vision impairment or blindness.
Cataract Formation: Lens damage can lead to cataract development, which causes clouding and vision impairment.
Glaucoma: Trauma, bleeding, or inflammation can cause increased intraocular pressure, resulting in secondary glaucoma and progressive vision loss.
Sympathetic Ophthalmia: This uncommon but serious condition occurs when the immune response to the injured eye affects the uninjured eye, potentially resulting in bilateral vision loss if not treated.
Scarring and Structural Damage: The healing process after a penetrating injury can cause scar tissue formation, distorting ocular structures and impairing vision.
Psychological and Social Impact
Penetrating eye injuries can have a significant psychological and social impact on people. Anxiety, depression, and post-traumatic stress disorder can result from the injury’s sudden and traumatic nature, as well as the possibility of vision loss. Patients may struggle to adjust to vision changes, which affects their daily activities, work, and quality of life.
Prevention
Prevention of penetrating eye injuries requires awareness and the use of appropriate protective measures in high-risk environments. The key preventive strategies are:
Protective Eyewear: Wearing safety goggles or face shields during work, sports, and recreational activities can significantly reduce the risk of ocular trauma.
Safe Handling of Sharp Objects: Teaching people how to use and store sharp tools and household items safely can help them avoid accidents.
Workplace Safety Protocols: Implementing and following safety guidelines in workplaces with potential hazards can help workers avoid eye injuries.
Supervision and Education: Supervising children when they use sharp objects and teaching them about eye safety can help to prevent accidents.
Penetrating Eye Injury: Diagnostic Approaches
Diagnosing penetrating eye injuries necessitates a thorough and systematic approach to determining the extent of damage and planning appropriate treatment. Here are the main diagnostic methods used:
Initial Assessment
History and Symptoms: A detailed history of the injury, including the nature of the object, the circumstances of the incident, and the amount of time since the injury, is critical. Assessing symptoms such as pain, vision changes, and the presence of a foreign body can aid in the diagnostic process.
Visual Acuity Testing: Determining the patient’s visual acuity is an important first step in the diagnostic process. It establishes a baseline for the severity of vision impairment and aids in monitoring changes over time.
Clinical Examination
External Examination: Inspecting the eye and surrounding tissues for signs of trauma, such as swelling, redness, and the presence of a foreign object, can provide an early indication of the severity of the injury.
Slit Lamp Examination: A slit lamp microscope enables a thorough examination of the anterior segment of the eye, including the cornea, anterior chamber, iris, and lens. This examination may reveal corneal lacerations, hyphema, or other anterior segment abnormalities.
Ophthalmoscopy: Direct or indirect ophthalmoscopy allows for visualization of the retina and optic nerve. It aids in the identification of retinal tears, detachments, and vitreous hemorrhage, providing critical information for diagnosis and treatment planning.
Imaging Techniques
X-Rays: Plain X-rays can reveal radiopaque foreign bodies in the eye or orbit. They are useful for identifying metallic or dense objects, but have low sensitivity for nonmetallic materials.
Computed Tomography (CT) Scan: A CT scan generates detailed cross-sectional images of the eye and orbit. It is extremely effective at detecting foreign bodies, bone fractures, and intraocular hemorrhages. CT scans are especially useful for determining the extent of the injury and planning surgical procedures.
Ultrasound: Ocular ultrasound, also known as B-scan ultrasonography, is a noninvasive imaging technique that produces real-time images of the eye’s internal structures. It is useful for detecting retinal detachment, vitreous hemorrhage, and the presence of intraocular foreign bodies when direct visualization is difficult.
Specialized Tests
Fluorescein Staining: Applying fluorescein dye to the ocular surface aids in detecting corneal abrasions, lacerations, and other epithelial defects. Under blue light, the dye highlights areas of damage, assisting with diagnosis and treatment planning.
Tonometry: Measuring intraocular pressure is critical in determining the risk of secondary glaucoma. Elevated intraocular pressure after trauma could indicate complications like hyphema or intraocular inflammation.
Magnetic Resonance Imaging (MRI): MRI is typically avoided in cases of penetrating eye injury due to the possibility of metallic foreign body movement. However, it may be used in limited situations where detailed imaging of soft tissues is required and no metallic foreign bodies are present.
Penetrating Eye Injury Treatment
Penetrating eye injuries require immediate and comprehensive care to avoid complications and preserve vision. The treatment approach varies depending on the severity and specifics of the injury, but usually includes the following steps:
Initial Management
Emergency Care: Immediate medical attention is required. Emergency medical personnel will evaluate the injury, stabilize the patient, and prevent further damage. Protective shields can be placed over the injured eye to prevent further trauma.
Pain Management: Giving pain relievers helps manage severe pain and discomfort. Commonly used are analgesics or systemic nonsteroidal anti-inflammatory drugs (NSAIDs).
Medical Treatment
To prevent infection, systemic antibiotics are given. Antibiotics applied topically can also help to prevent bacterial contamination and endophthalmitis.
Tetanus Prophylaxis: If the injury is caused by a contaminated object, the patient is given tetanus prophylaxis based on their immunization history.
Anti-inflammatory Medications: Corticosteroids may be used to reduce inflammation and lower the risk of scarring and other complications.
Surgical Intervention
Foreign Body Removal: Surgical removal of the foreign body is frequently required, especially when it is embedded in sensitive structures. This procedure is typically done under general anesthesia.
Wound Repair: Suturing corneal or scleral lacerations is critical for restoring the structural integrity of the eye. Microsurgical techniques and specialized sutures are used to achieve the best results.
Vitrectomy: When the vitreous humor is compromised or there is significant intraocular hemorrhage, a vitrectomy may be performed. This procedure involves the removal of the vitreous gel and any blood, followed by the introduction of a clear solution to keep the eye shape.
Retinal Repair: If the injury resulted in retinal detachment or tears, retinal repair surgery is required. Laser photocoagulation, cryotherapy, and scleral buckling are some of the techniques used to reattach and secure the retina.
Post-operative Care
Follow-Up Appointments: Regular visits to an ophthalmologist are required to monitor healing, assess intraocular pressure, and detect any signs of infection or complications.
Visual Rehabilitation: Patients may need visual rehabilitation, such as corrective lenses, low vision aids, or occupational therapy, to help them adjust to any residual visual impairment.
Psychological Support: Treating the psychological impact of the injury is critical. Counseling and support groups can assist patients and their families in coping with trauma and adapting to vision changes.
Long-Term Management
Complication Monitoring: Long-term follow-up is required to detect potential complications such as glaucoma, cataracts, and recurrent retinal detachment. Regular eye exams and imaging studies are part of ongoing treatment.
Secondary Interventions: Additional surgical procedures may be required to resolve complications or improve visual outcomes.
Frequently Asked Questions Concerning Penetrating Eye Injury
What should I do if I suspect a penetrating eye injury?
If you suspect you have sustained a penetrating eye injury, seek medical attention right away. Avoid attempting to remove any foreign objects or applying pressure to the injured eye. To avoid further damage, cover the eye with a protective shield or the bottom of a paper cup before heading to the nearest emergency room.
How are penetrating eye injuries diagnosed?
A penetrating eye injury is identified using a combination of clinical examination, imaging techniques, and specialized tests. Ophthalmologists use slit lamp microscopy, ophthalmoscopy, and imaging studies such as CT scans and ultrasound to determine the extent of the injury and plan appropriate treatment.
Can a penetrating eye injury lead to permanent vision loss?
Yes, a penetrating eye injury can result in permanent vision loss if not treated quickly and properly. The severity and location of the injury, as well as the timing of medical intervention, all influence the extent of vision loss.
What are the most common complications from a penetrating eye injury?
Infections (such as endophthalmitis), retinal detachment, cataracts, glaucoma, and scarring are among the most common complications. If not properly managed, these complications can cause significant vision impairment or loss.
Is surgery always necessary for penetrating eye injuries?
Surgery is frequently required to remove foreign bodies, repair lacerations, and treat intraocular damage. The nature and severity of the injury determine the specific surgical approach required. In some cases, less invasive treatments may suffice, but severe injuries usually necessitate surgical intervention.
How long does recovery take from a penetrating eye injury?
The recovery time varies according to the severity of the injury and the type of treatment required. Initial healing may take a few weeks, but complete recovery and rehabilitation can take months. Regular follow-up appointments are essential for tracking progress and addressing any complications.
Are penetrating eye injuries preventable?
While not all penetrating eye injuries are preventable, many can be avoided by wearing appropriate protective eyewear in high-risk environments such as the workplace, sports, and certain recreational activities. Adherence to safety guidelines and careful handling of sharp objects can also help to reduce the risk.
How do antibiotics help treat penetrating eye injuries?
Antibiotics are critical for preventing and treating infections caused by penetrating eye injuries. They are used both systemically and topically to lower the risk of endophthalmitis and other bacterial infections.
Will my vision return to normal following a penetrating eye injury?
The extent and location of the injury, as well as the timeliness of treatment, all influence the prognosis for vision recovery. Some patients may recover completely, while others may still have vision impairment. Early and effective treatment increases the likelihood of a favorable visual outcome.
Are there any resources for people who have suffered penetrating eye injuries?
Yes, several organizations and support groups offer resources and assistance to people who have sustained penetrating eye injuries. These resources provide information, emotional support, and practical advice for managing the condition and adapting to vision changes.
Trusted Resources and Support
Books and Organizations
Books:
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling.
- “Trauma and Emergency Care for the Eye”, Robert J. Cionni and Robert J. Derick.
Organizations:
- The American Academy of Ophthalmology (AAO): Offers comprehensive information on eye health, including trauma care and treatment recommendations.
- Prevent Blindness: Provides resources for preventing eye injuries and maintaining vision health.
- Eye Trauma Registry: Gathers information and offers resources for managing and preventing eye injuries.
Financial Aid Options
Insurance Coverage: Most health insurance policies provide emergency care and treatment for penetrating eye injuries. It is critical to consult with your insurance provider to determine the specifics of your coverage.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations may provide financial assistance for medications and treatments related to eye injuries. RxAssist and other programs provide information about these resources.
Non-Profit Organizations: Organizations such as the HealthWell Foundation and the EyeCare America program provide financial assistance and support to people who require eye care and surgery.
Government Programs: Medicaid and Medicare cover emergency care and treatment of eye injuries for eligible individuals. Additionally, programs such as the Children’s Health Insurance Program (CHIP) help children in need of medical care.






