Orbital hemorrhage is the accumulation of blood within the orbit, the bony cavity that houses the eye. This condition can be caused by trauma, such as blunt or penetrating injuries, surgical complications, vascular abnormalities, or spontaneous bleeding disorders. The presence of blood in the orbital space can cause increased pressure, resulting in pain, swelling, bruising, and, in severe cases, vision impairment due to optic nerve compression or eye displacement.
The clinical presentation of orbital hemorrhage varies according to its severity and underlying cause. Symptoms typically include sudden onset of pain, proptosis (eye protrusion), ecchymosis (bruising around the eye), decreased visual acuity, and limited eye movement. Clinical examination and imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), are typically used to confirm the diagnosis and determine the extent of the hemorrhage and its impact on orbital structures.
Prompt recognition and treatment of orbital hemorrhage are critical for avoiding long-term complications, including permanent vision loss. Understanding the nature and implications of this condition is critical to effective treatment and better patient outcomes.
Orbital Hemorrhage Management and Treatment
The management and treatment of orbital hemorrhage necessitates a comprehensive approach that addresses the underlying cause, relieves symptoms, and prevents complications. Here are the standard treatments for managing orbital hemorrhage:
- Observation and Monitoring: If the hemorrhage is small and does not cause significant symptoms, a conservative approach may be used. This entails closely monitoring the patient’s condition with routine clinical examinations and imaging studies. Minor hemorrhages that are expected to resolve spontaneously without intervention are best treated with observation.
- Medical Therapy: Medications may be prescribed to alleviate symptoms and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help to reduce pain and swelling. If the hemorrhage is caused by an underlying bleeding disorder, specific coagulopathy treatments, such as vitamin K or clotting factor replacement, may be required.
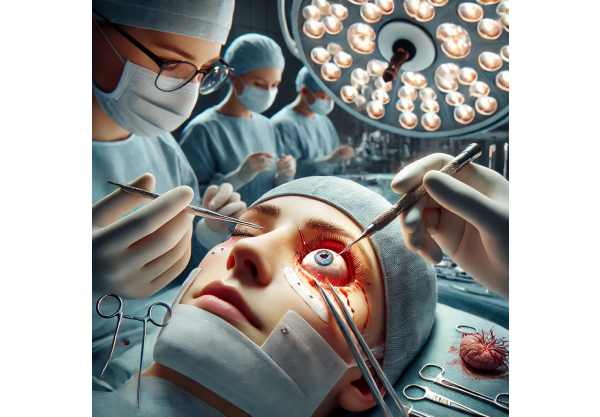
- Orbital Decompression: Orbital decompression surgery is recommended in severe cases where hemorrhage causes significant proptosis or optic nerve compression, resulting in vision loss. This procedure involves making an opening in the orbital walls to relieve pressure and allow blood to drain, thereby lowering the risk of permanent damage to the optic nerve and other structures.
- Drainage Procedures: For moderate to large hemorrhages, particularly those resulting in significant proptosis or impaired ocular function, surgical drainage may be required. To remove the accumulated blood, an incision is made in the conjunctiva or on the skin. Drainage reduces pressure, restores normal eye position, and enhances visual outcomes.
- Management of Complications: In addition to treating the hemorrhage, it is critical to manage any complications that may arise. These can include corneal exposure caused by severe proptosis, which may necessitate protective measures such as lubricating eye drops or temporary tarsorrhaphy (partial eyelid closure) to avoid corneal damage.
- Rehabilitation and Follow-Up Care: Post-treatment rehabilitation and regular follow-up care are essential for assessing progress and addressing any remaining issues. This could include visual rehabilitation services, physical therapy to improve eye movement, and routine ophthalmologic exams to detect any late complications.
Latest Breakthrough Innovations in Orbital Hemorrhage Treatment
Recent advances in medical research and technology have resulted in novel approaches that give patients suffering from orbital hemorrhage renewed hope. These cutting-edge innovations include advanced imaging techniques, new surgical methods, regenerative medicine, and integrative care models. Each of these innovations offers distinct advantages and has the potential to improve orbital hemorrhage management.
Advanced Imaging Techniques
Imaging technology advancements have significantly improved the accuracy and efficiency with which orbital hemorrhage is diagnosed and monitored.
High-Resolution Imaging: High-resolution imaging modalities, such as enhanced CT and MRI scans, allow for detailed visualization of orbital structures and the extent of hemorrhage. These advanced imaging techniques enable early and precise diagnosis, which aids in treatment decision-making and therapy response monitoring.
Dynamic Contrast-Enhanced Imaging: Techniques like contrast-enhanced MRI or CT angiography can help identify active bleeding sites and vascular abnormalities that are causing the hemorrhage. These imaging methods provide useful information for planning surgical interventions and determining treatment efficacy.
Novel Surgical Methods
Innovative surgical techniques have been developed to improve the outcomes for patients with orbital hemorrhage. These methods aim to improve the precision, safety, and efficacy of surgical interventions.
Minimally Invasive Surgery: Endoscopic orbital decompression and drainage are two minimally invasive surgical techniques that have several advantages over traditional open surgery. These methods use small incisions and specialized instruments to access and treat the hemorrhage, lowering the risk of complications, minimizing scarring, and promoting faster healing.
Image-Guided Surgery: Image-guided surgical systems use real-time imaging to help surgeons navigate and perform precise procedures. These systems improve the accuracy of procedures such as orbital decompression and drainage by ensuring proper alignment and minimizing damage to surrounding tissues. Image-guided surgery improves surgical outcomes while lowering the risk of postoperative complications.
Regenerative Medicine
Regenerative medicine provides novel approaches to repairing and restoring damaged orbital tissues, opening up new possibilities for patients with orbital hemorrhage.
Stem Cell Therapy: Stem cells are used to regenerate damaged bones and soft tissues in the orbit. Recent advances in stem cell technology have allowed for the creation of induced pluripotent stem cells (iPSCs), which can be generated from the patient’s own cells, lowering the likelihood of immune rejection. Researchers are investigating the potential of iPSCs in regenerating orbital tissues and improving outcomes in patients with orbital hemorrhage.
Biomaterials and Tissue Engineering: Techniques are being developed to create scaffolds that aid in tissue regeneration. These scaffolds can be implanted into the orbit to promote the growth of new bone and soft tissues, thereby accelerating healing and restoring the orbit is structural integrity. Biomaterial advancements, such as biocompatible polymers and hydrogels, are accelerating the development of novel orbital reconstruction solutions.
Integrative and Complementary Approaches
Integrative approaches combine conventional medical treatments with complementary therapies to provide comprehensive care for patients suffering from orbital hemorrhage.
Nutritional Support: Adequate nutrition is critical for promoting healing and preventing hemorrhage. Nutritional interventions, such as the administration of specific vitamins and minerals that promote vascular health, can supplement surgical and medical treatments and improve patient outcomes.
Physical Therapy and Rehabilitation: Physical therapy and rehabilitation are critical for restoring function and mobility following an orbital hemorrhage. Specialized exercises and therapies can assist patients in regaining strength, improving eye movement, and reducing pain and stiffness. Physical therapy programs are tailored to each patient’s specific needs, resulting in optimal recovery and functional outcomes.
Pain Management: Effective pain management is an essential part of treating patients with orbital hemorrhage. Complementary therapies, such as acupuncture and mindfulness meditation, can help relieve pain and reduce the need for opioids. Integrative pain management approaches offer holistic relief and promote overall health.
Personalized Medicine
Personalized medicine tailors treatment plans to each patient’s unique characteristics, including genetic profile, lifestyle, and specific injury manifestations.
Genomic Testing: Advances in genomic testing have enabled the identification of genetic factors that may influence a patient’s healing process and response to treatment. Understanding these genetic factors can help guide personalized treatment strategies, ensuring that patients receive the most effective therapies based on their individual genetic makeup.
Lifestyle and Environmental Modifications: Personalized medicine emphasizes the importance of lifestyle and environmental factors in managing orbital hemorrhage. Patients can benefit from personalized recommendations for nutrition, exercise, and environmental changes that promote healing and prevent future injuries.
Artificial Intelligence, Machine Learning
The use of artificial intelligence (AI) and machine learning (ML) in healthcare has the potential to transform the treatment of orbital hemorrhage.
AI-Powered Diagnostics: Artificial intelligence algorithms can analyze large datasets of imaging and clinical data to identify patterns and predict disease progression. AI-powered diagnostics can improve the accuracy and efficiency of detecting orbital hemorrhage, allowing for earlier intervention and personalized treatment strategies.
Predictive Modeling: Machine learning models can forecast the likelihood of complications and guide treatment decisions based on individual patient data. Predictive modeling assists clinicians in developing proactive management plans, which improves long-term outcomes for patients with orbital hemorrhage.






