What is PseudoPapilledema?
Pseudopapilledema is a condition characterized by the appearance of optic disc swelling that resembles true papilledema but does not cause increased intracranial pressure. Unlike papilledema, which can indicate potentially fatal conditions such as brain tumors or intracranial hypertension, pseudopapilledema is usually benign. Congenital anomalies such as optic nerve head drusen, hyperopia, or crowded optic discs are frequently the cause of swelling in pseudopapilledema.
One of the most common causes of pseudopapilledema is the presence of calcified deposits in the optic nerve head. These drusen can make the optic disc appear elevated and swollen during a fundoscopic examination. Pseudopapilledema can be difficult to diagnose because it can mimic true papilledema on clinical examination, resulting in unnecessary and extensive neurological evaluations.
Patients with pseudopapilledema frequently don’t have the same symptoms as those with true papilledema. If symptoms exist, they may include temporary visual obscurations or a mild decrease in visual acuity. However, many patients are asymptomatic. Accurate differentiation between pseudopapilledema and true papilledema is critical for avoiding misdiagnosis and unnecessary interventions.
Pseudopapilledema: Management and Treatment
Managing pseudopapilledema is primarily concerned with accurate diagnosis and monitoring to ensure that the condition does not progress to true optic nerve damage. Because pseudopapilledema is usually benign, the treatment approach is generally conservative, with regular monitoring rather than aggressive interventions.
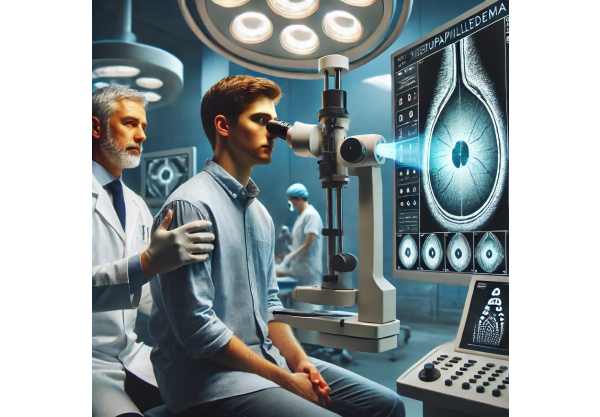
Diagnostic Techniques
A clinical examination and advanced imaging techniques are required to make an accurate diagnosis of pseudopapilledema. The key diagnostic methods are:
- Fundoscopic Examination: The initial assessment frequently includes a thorough examination of the optic disc to detect signs of drusen or other abnormalities.
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the optic nerve head, enabling the detection of drusen and other structural changes.
- B-Scan Ultrasonography: This imaging technique can detect buried optic nerve head drusen by capturing detailed images of the optic nerve.
- Fluorescein Angiography: This test measures blood flow in the retina and optic nerve to distinguish true papilledema from pseudopapilledema.
Regular monitoring
Patients with pseudopapilledema require regular follow-up visits to monitor for any changes in the optic nerve head or visual function. These visits typically include:
- Visual Field Testing: Regular visual field tests can detect changes in peripheral vision that may indicate progression.
- Repeat OCT Scans: Periodic OCT scans assess the stability of the optic nerve head drusen and detect any new changes.
- Patient Education: Educating patients about the benign nature of pseudopapilledema and the importance of regular monitoring reduces anxiety and improves compliance with follow-up visits.
Symptomatic Treatment
While pseudopapilledema frequently does not require direct treatment, associated symptoms or complications may be managed as follows:
- Managing Visual Symptoms: If patients have vision problems, they may benefit from optical aids or changes to their current corrective lenses.
- Treating Underlying Conditions: If hyperopia causes pseudopapilledema, correcting the refractive error with appropriate glasses or contact lenses can help relieve symptoms.
Reducing unnecessary interventions
One of the most important aspects of managing pseudopapilledema is avoiding unnecessary and potentially invasive diagnostic procedures that are commonly used for true papilledema. Accurate diagnosis using non-invasive imaging helps to avoid extensive neurological evaluations and the resulting stress for the patient.
Breakthrough Innovations in Pseudopapilledema Treatment
Recent advances in medical research and technology have resulted in significant improvements in the diagnosis and treatment of pseudopapilledema. These cutting-edge approaches give patients new hope by providing more effective, safer, and less invasive ways to manage this condition.
Advanced Imaging Techniques
Imaging technology advancements have significantly improved the ability to accurately diagnose and monitor pseudopapilledema. These advances include:
- Enhanced Optical Coherence Tomography (OCT): High-resolution OCT, specifically enhanced depth imaging OCT (EDI-OCT), allows for more detailed visualization of the optic nerve head and drusen. This allows for more accurate differentiation between pseudopapilledema and true papilledema, as well as precise monitoring of drusen over time.
- Ultra-Widefield Imaging: This imaging technique captures a wider view of the retina and optic nerve head, providing detailed documentation of the optic disc appearance and peripheral retina. Ultra-widefield imaging can help detect subtle changes in the optic nerve head that may not be visible with traditional fundus photography.
- Adaptive Optics: Adaptive optics imaging systems compensate for optical aberrations in real time, resulting in ultra-high-resolution images of the retina and optic nerve head. This technology enables the visualization of individual drusen and other fine structural details, which improves diagnostic accuracy.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning (ML) are revolutionizing ophthalmology, particularly in the diagnosis and treatment of pseudopapilledema. AI algorithms can identify patterns in large datasets from imaging studies and clinical records, improving diagnostic accuracy. Key advances in AI and machine learning include:
- AI-Based Diagnostic Tools: AI algorithms can analyze OCT and fundus images to identify optic nerve head drusen and distinguish between pseudopapilledema and true papilledema. These tools help ophthalmologists make more accurate and timely diagnoses.
- Predictive Modeling: Using individual patient characteristics, machine learning models can predict whether pseudopapilledema will progress to true papilledema. This enables clinicians to create personalized monitoring and treatment plans.
Gene Therapy and Genetic Research
Ongoing genetic research seeks to identify the underlying genetic factors that contribute to pseudopapilledema. Understanding the genetic basis of this condition can lead to more targeted therapies and personalized treatment options. The current research focuses on:
- Identifying Genetic Markers: Researchers are attempting to identify specific genetic mutations linked to the development of optic nerve head drusen and pseudopapilledema. Genetic testing can help identify at-risk individuals and inform monitoring strategies.
- Gene Therapy: Gene therapy techniques seek to correct genetic defects that contribute to the development of optic nerve head drusen. Although still in its early stages of development, gene therapy shows promise for preventing or reducing drusen accumulation and alleviating associated symptoms.
Advanced Diagnostic Algorithms
The development of advanced diagnostic algorithms has increased the accuracy and efficiency of diagnosing pseudopapilledema. These algorithms combine data from various imaging modalities and clinical parameters to provide a thorough evaluation. Innovative diagnostic algorithms include:
- Multimodal Imaging Analysis: Combining data from OCT, B-scan ultrasonography, and fundus photography enables a more comprehensive evaluation of the optic nerve head. Advanced algorithms use this data to distinguish between pseudopapilledema and true papilledema with high accuracy.
- Automated Drusen Detection: Automated software tools can detect and quantify optic nerve head drusen in OCT images, resulting in objective and repeatable measurements. These tools help clinicians monitor drusen progression and determine treatment efficacy.
Telemedicine & Remote Monitoring
Telemedicine and remote monitoring technologies have become increasingly important in the management of pseudopapilledema, especially during the COVID-19 pandemic. These tools improve patient access to care and enable continuous monitoring. Significant advances in telemedicine and remote monitoring include:
- Virtual Consultations: Telemedicine platforms allow patients to communicate with ophthalmologists from the comfort of their own homes. Virtual consultations allow you to discuss symptoms, review imaging results, and develop treatment plans without the need for in-person visits.
- Home Monitoring Devices: Portable devices and smartphone apps enable patients to monitor their visual function and take images of their optic nerve head. These devices can send data to healthcare providers for remote assessment and early detection of changes.
Personalized Medicine
Personalized medicine tailors treatment strategies to individual patient characteristics, resulting in more effective and targeted interventions. Advances in personalized medicine for pseudopapilledema include the following:
- Customized Monitoring Plans: Genetic and biomarker analysis identifies patients who are at a higher risk of progression, allowing for the creation of personalized monitoring schedules. This approach ensures that patients receive prompt and appropriate follow-up care.
- Individualized Treatment Approaches: Personalized treatment plans take into account the patient’s genetics, lifestyle, and comorbidities. Interventions tailored to the individual patient improve treatment efficacy while lowering the risk of adverse effects.
Collaborative Research Networks
Collaborative research networks are critical to improving understanding and management of pseudopapilledema. These networks bring together researchers, clinicians, and patients to speed up the development of novel diagnostic and therapeutic approaches. Major initiatives include:
- International Research Collaborations: Collaborative networks, such as the Optic Disc Drusen Research Network, enable multicenter studies into the genetic and clinical aspects of pseudopapilledema. These collaborations improve data sharing and encourage the creation of evidence-based guidelines.
- Patient Registries: Patient registries collect detailed information on people with pseudopapilledema, which aids research and provides valuable insights into disease patterns and treatment outcomes.






