What is Retinal Hemangioblastoma?
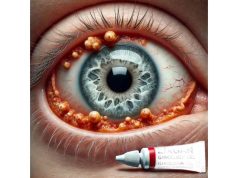
Retinal hemangioblastoma is a rare, benign vascular tumor of the retina that is frequently associated with von Hippel-Lindau (VHL) disease, a genetic condition that predisposes people to a variety of tumors and cysts throughout their bodies. These tumors are typically made up of blood vessels and can cause serious ocular complications if not treated. Retinal hemangioblastomas are most frequently diagnosed in young adults and can affect one or both eyes.
The tumor can cause a variety of symptoms, including vision loss, retinal detachment, and intraocular hemorrhage. Patients may experience blurred vision, floaters, or a visible mass in their visual field. The tumor’s effect on the retinal structure and surrounding tissues causes these symptoms, which frequently result in fluid accumulation and subsequent retinal detachment.
A comprehensive eye examination is required to diagnose retinal hemangioblastoma, which includes fundus photography, fluorescein angiography, and optical coherence tomography (OCT). These imaging techniques aid in visualizing the tumor, determining its size, location, and effect on the retina, and guiding treatment decisions. Understanding and detecting retinal hemangioblastomas early is critical for avoiding severe vision loss and effectively managing associated systemic conditions.
Traditional Retinal Hemangioblastoma Management
Managing retinal hemangioblastoma requires a multifaceted approach that takes into account both the ocular and systemic implications of the condition, particularly when it is associated with VHL disease. The primary goals of treatment are to maintain vision, avoid complications, and address any underlying systemic issues.
Observation and Monitoring
For small, asymptomatic retinal hemangioblastomas that do not pose an immediate threat to vision, a conservative approach of regular observation and monitoring is common. This includes:
- Regular Eye Examinations: Patients receive comprehensive eye exams on a regular basis to monitor tumor growth and detect changes in retinal health. This allows for more timely decisions about intervention if necessary.
- Imaging Studies: The regular use of imaging techniques such as OCT and fluorescein angiography aids in tracking the tumor’s progression and impact on the retina. These tools are critical for detecting complications such as retinal detachment or macular edema.
Laser Photocoagulation
Laser photocoagulation is a common treatment for retinal hemangioblastomas, particularly for smaller tumors located away from the macula (the retina’s central area). This procedure uses a laser to create small burns around the tumor, which help to seal off the blood vessels and reduce fluid leakage.
The Mechanism of Action:
The laser causes thermal damage to the abnormal blood vessels, causing them to coagulate and contract. This reduces the size of the tumor and helps to stabilize the retina.
Procedure:
Laser photocoagulation is usually performed as an outpatient procedure with local anesthesia. Patients may feel mild discomfort and have temporary visual disturbances, but recovery is usually quick.
Outcomes:
Laser photocoagulation can effectively slow the growth of small hemangioblastomas and prevent complications. However, it is less effective for larger tumors or those located near the macula.
Cryotherapy
Cryotherapy is another treatment option for retinal hemangioblastomas, especially for peripheral tumors that are difficult to access with laser photocoagulation. This method involves freezing the tumor with a cryoprobe placed on the eye’s external surface.
The Mechanism of Action:
Cryotherapy freezes tumors at extremely low temperatures, causing cellular damage and destruction. This causes the formation of ice crystals within tumor cells, resulting in cell death.
Procedure:
The cryoprobe is placed on the sclera (the white part of the eye) above the tumor. Depending on the size and location of the tumor, the procedure is performed with either local or general anesthesia.
Outcomes:
Cryotherapy can help reduce tumor size and prevent complications. It is especially effective for tumors in the peripheral retina. Multiple sessions may be required, and there is a risk of collateral damage to surrounding retinal tissue.
Radiotherapy
For larger or more aggressive retinal hemangioblastomas, radiotherapy may be considered. This treatment employs targeted radiation to destroy tumor cells while sparing healthy tissue.
The Mechanism of Action:
Radiation therapy damages tumor cells’ DNA, preventing them from growing and dividing. Over time, this causes tumor shrinkage and stabilization.
Procedure:
External beam radiation and brachytherapy are two techniques for delivering radiotherapy. The technique used is determined by the tumor’s size, location, and the patient’s general health.
Outcomes:
Radiotherapy can effectively shrink larger hemangioblastomas and prevent future growth. However, it is associated with potential side effects such as radiation retinopathy and cataract formation, which must be carefully considered and treated.
Vitreoretinal Surgery
If retinal hemangioblastomas cause complications such as retinal detachment or significant vitreous hemorrhage, vitreoretinal surgery may be required. This involves complex surgical procedures to repair the retina and, if possible, remove the tumor.
The Mechanism of Action:
Vitreoretinal surgery aims to reattach the retina, remove any hemorrhage, and treat the tumor directly if it is causing structural issues.
Procedure:
Surgical techniques used include vitrectomy (removal of the vitreous gel) and scleral buckling (placing a band around the eye to push the retina back into place). The specific approach is determined by the type of detachment and the location of the tumor.
Outcomes:
Vitreoretinal surgery can effectively treat severe complications while restoring retinal structure and function. However, it carries a higher risk of complications and necessitates the expertise of a skilled surgeon with extensive experience in complex retinal cases.
Systematic Management
Given the link between retinal hemangioblastomas and von Hippel-Lindau (VHL) disease, systemic management is an essential component of treatment. This involves:
- Genetic Counseling and Testing: Patients with retinal hemangioblastomas, particularly those who have a family history of VHL disease, should receive genetic counseling and testing. Identifying the VHL gene mutation can aid in the early detection and management of other possible tumors and cysts in the body.
- Regular Systemic Screening: Patients with VHL disease must undergo regular screening for tumors in other organs such as the kidneys, pancreas, and central nervous system. Early detection and treatment of these tumors is critical to improving overall prognosis and quality of life.
- Targeted Therapies: Progress in molecular biology has resulted in the development of targeted therapies for VHL-related tumors. Drugs that inhibit tumor growth pathways, such as VEGF inhibitors, are being studied for their potential use in the treatment of retinal hemangioblastomas and other VHL-associated tumors.
Innovative Retinal Hemangioblastoma Treatment Options
Recent advances in medical research and technology have resulted in several novel treatments for retinal hemangioblastoma, significantly improving patient outcomes and expanding the therapeutic options. These cutting-edge innovations aim to improve treatment precision, efficacy, and safety.
Anti-VEGF Therapies
Anti-VEGF (vascular endothelial growth factor) therapy has emerged as a potentially effective treatment for retinal hemangioblastomas. Overexpression of the protein VEGF, which promotes blood vessel growth, has been linked to the development and progression of these tumors.
The Mechanism of Action:
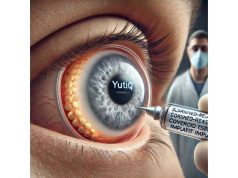
Anti-VEGF drugs, such as bevacizumab (Avastin) and ranibizumab (Lucentis), inhibit VEGF activity, reducing abnormal blood vessel growth and permeability. This helps to stabilize the tumor and reduces complications such as macular edema.
Clinical Applications:
Anti-VEGF therapy is administered via intravitreal injections, in which the drug is injected directly into the eye. The tumor’s response and the presence of complications determine the frequency and duration of treatment.
Outcomes:
Clinical trials have demonstrated that anti-VEGF therapy can effectively reduce tumor size, fluid leakage, and improve visual outcomes in patients with retinal hemangioblastomas. This treatment is especially effective for tumors that are difficult to reach with laser or cryotherapy.
Photodynamic therapy (PDT)
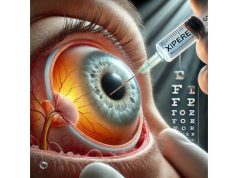
Photodynamic therapy (PDT) is a minimally invasive treatment that uses a photosensitizing agent and light exposure to kill tumor cells.
The Mechanism of Action:
PDT entails administering a photosensitizing agent, such as verteporfin, into the bloodstream. The agent accumulates specifically in the tumor’s blood vessels. When exposed to a specific wavelength of light, the agent produces reactive oxygen species, which damage and destroy tumor cells.
Clinical Applications:
PDT is an outpatient procedure. Following the injection of the photosensitizing agent, the dilated pupil directs a laser light at the tumor. The entire process usually takes around 30 minutes.
Outcomes:
PDT has shown promising results in treating retinal hemangioblastomas, particularly those near the macula. It has the advantage of being less invasive than traditional surgical methods and carries a lower risk of complications. However, multiple treatment sessions may be required for the best results.
Gene and Molecular Therapies
Advances in genetic and molecular therapies open up new avenues for treating retinal hemangioblastomas, particularly in VHL patients.
Genetic Therapy:
Gene therapy is the process of introducing, removing, or changing genetic material within a patient’s cells to treat or prevent disease. Gene therapy for retinal hemangioblastomas aims to correct genetic mutations that cause tumor development.
The Mechanism of Action:
Gene therapy can take many forms, including using viral vectors to deliver healthy copies of the VHL gene to retinal cells, silencing mutant genes, and using CRISPR-Cas9 technology to directly edit defective genes. These techniques have the potential to target the underlying cause of tumor formation, providing a long-term solution for patients with VHL-associated retinal hemangioblastomas.
Clinical Applications:
Gene therapy for retinal hemangioblastomas is still in the experimental stage. However, clinical trials are currently underway to determine the safety and efficacy of these approaches. If successful, gene therapy could revolutionize medicine, providing hope for a permanent cure.
Outcomes:
Early results from gene therapy trials for other retinal diseases are promising, with improved vision and retinal function. As research advances, gene therapy may become a viable treatment option for retinal hemangioblastomas, especially in patients with genetic predispositions.
Nanotechnology-Based Treatments
Nanotechnology is being investigated for its ability to deliver targeted therapies to retinal tumors with high precision and few side effects.
The Mechanism of Action:
Nanoparticles can be designed to deliver therapeutic agents such as chemotherapy drugs, anti-VEGF agents, and gene editing tools directly to the tumor site. Specific stimuli, such as pH changes or light exposure, can cause these nanoparticles to release their payload.
Clinical Applications:
Intravitreal injections or systemic delivery are both options for nanoparticle administration. Once inside the body, they travel to the tumor site and release therapeutic agents, which target tumor cells while sparing healthy tissue.
Outcomes:
Preclinical research has demonstrated that nanotechnology-based treatments can effectively reduce tumor size and improve visual outcomes in animal models of retinal hemangioblastomas. These treatments have the potential for precise and controlled therapy with fewer side effects than traditional methods.
Immunotherapy
Immunotherapy, which uses the immune system to fight cancer, is being studied as a possible treatment for retinal hemangioblastomas.
The Mechanism of Action:
Immunotherapy stimulates the immune system to recognize and attack tumor cells. Immune checkpoint inhibitors, adoptive cell transfer, and cancer vaccines are all options for achieving this goal.
Clinical Applications:
While immunotherapy has been used successfully to treat a variety of cancers, its application in retinal tumors is still in the early stages of development. Clinical trials are required to determine the safety and efficacy of immunotherapy for retinal hemangioblastomas.
Outcomes:
Immunotherapy has shown promise in treating other types of tumors by strengthening the body’s natural defenses. If effective for retinal hemangioblastomas, it could offer a non-invasive treatment option with long-term results.
Artificial Intelligence, Machine Learning
AI and machine learning (ML) are being used to diagnose and plan treatments for retinal hemangioblastomas.
The Mechanism of Action:
AI and machine learning algorithms can identify patterns and predict tumour behavior in large datasets of retinal images. These technologies can help ophthalmologists make more accurate diagnoses and create personalized treatment plans.
Clinical Applications:
AI-powered diagnostic tools can help detect retinal hemangioblastomas earlier, resulting in better treatment outcomes. In addition, AI can be used to monitor disease progression and treatment response, allowing for timely therapy adjustments.
Outcomes:
AI and machine learning have the potential to transform the treatment of retinal hemangioblastomas by providing precise, data-driven insights. These technologies can improve diagnostic accuracy, treatment strategies, and patient outcomes.
Future Directions
The future of retinal hemangioblastoma treatment appears bright, thanks to ongoing research and technological advancements. Continued research into genetic and molecular therapies, nanotechnology, immunotherapy, and AI integration is likely to yield new breakthroughs. As our understanding of the underlying mechanisms of retinal hemangioblastomas grows, targeted treatments that address the underlying causes of the disease will become more feasible, providing hope for long-term improvements in patient outcomes.