Scleral staphyloma is a serious ocular condition marked by an outpouching or bulging of the weakened sclera, the white outer layer of the eye, which is frequently accompanied by thinning and degeneration of the underlying uveal tissue. This condition can cause severe vision impairment and is commonly associated with high myopia, trauma, inflammation, or diseases such as scleritis and keratoconus. The bulging occurs when the eye’s internal pressure exerts force on the weakened scleral wall, resulting in a localized protrusion.
Patients with scleral staphyloma commonly present with symptoms such as decreased visual acuity, distorted vision, and, in some cases, visible changes to the shape of the eye. The condition can affect any part of the eye, including the anterior (front), equatorial (mid-section), or posterior (back) sclera, with posterior staphylomas being the most common and frequently the most difficult to treat due to their proximity to the optic nerve and macula.
A thorough eye examination and imaging studies are required to diagnose scleral staphyloma. Tools such as optical coherence tomography (OCT), B-scan ultrasonography, and magnetic resonance imaging (MRI) are critical for determining the extent of scleral thinning and bulging and developing appropriate treatment strategies. Early detection and intervention are critical for avoiding further progression and managing the complications associated with this condition.
Scleral Staphyloma Care and Treatment
The goals of scleral staphyloma management and treatment are to stabilize the condition, preserve vision, and address any underlying causes or complications. Treatment options vary according to the severity of the staphyloma and the patient’s specific needs.
- Observation and Monitoring: If the staphyloma is small and does not cause significant visual impairment, regular monitoring may be adequate. Patients should have routine eye exams to monitor the progression of the condition and detect any signs of complications early on. This method aids in making timely decisions about when to start more aggressive treatments, if necessary.
- Protective Eyewear: Individuals with scleral staphyloma, particularly those with anterior staphylomas or those at risk of trauma, should wear protective eyewear to avoid injury. Trauma to an eye with a staphyloma can result in severe complications, such as sclera rupture.
- Corrective Lenses: Corrective lenses, such as glasses and contact lenses, can improve visual acuity in patients with scleral staphyloma. Specialized contact lenses, such as scleral lenses, provide a smooth refractive surface over the irregular shape of the eye, increasing vision and comfort.
- Medical Management: Treating underlying conditions that cause scleral staphyloma is critical. For example, managing high myopia with appropriate corrective lenses or refractive surgery, controlling inflammation with corticosteroids or immunosuppressive agents in cases of scleritis, and addressing any systemic diseases that may compromise scleral integrity are all critical steps in overall management.
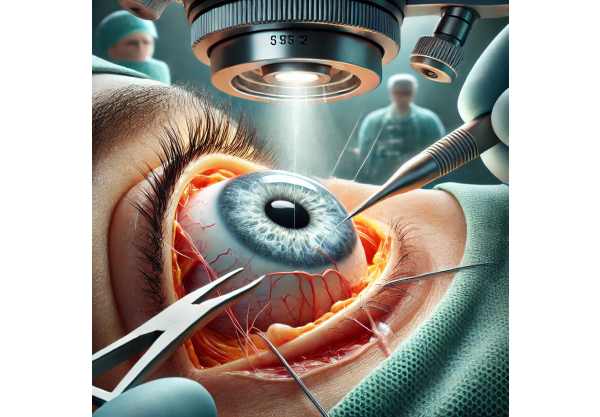
- Scleral Reinforcement Surgery: To provide structural support, graft materials such as donor sclera, fascia lata, or synthetic materials onto the thinned sclera. This procedure aims to prevent further thinning and bulging of the sclera, lowering the risk of complications. It is a complex surgery that necessitates meticulous planning and execution to ensure the best results.
- Scleral Patch Grafting: Scleral patch grafting, like scleral reinforcement, involves applying a patch to a weakened area of the sclera. This can be accomplished with autologous tissue (from the patient), allogeneic tissue (from a donor), or synthetic materials. The goal is to strengthen the scleral wall and prevent the staphyloma from progressing further.
- Vitrectomy: If scleral staphyloma is associated with retinal detachment or other vitreoretinal complications, a vitrectomy may be required. This surgical procedure consists of removing the vitreous gel from the eye and repairing any retinal tears or detachments. Vitrectomy can help stabilize the eye and improve vision in patients with complex staphylomas.
- Regular Follow-Up and Rehabilitation: Patients with scleral staphyloma require continuous follow-up to monitor their condition and adjust treatment plans as needed. Visual rehabilitation, which includes low vision aids and specialized training, can help patients maximize their remaining vision while also maintaining their quality of life.
New Breakthrough Therapies for Scleral Staphyloma
Ophthalmology has made significant advances in the diagnosis and treatment of scleral staphyloma. Cutting-edge innovations are improving our understanding of the condition and opening up new avenues for treatment and monitoring. These innovations seek to improve patient outcomes and quality of life by providing more effective and minimally invasive treatments.
Advanced Imaging Technology
Scleral staphyloma management requires accurate and early diagnosis. Imaging technology advancements are improving our ability to visualize and assess the extent of scleral thinning and bulging, as well as any associated ocular abnormalities.
- Enhanced Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the sclera and other ocular structures. Advanced OCT technologies, such as swept-source OCT and OCT angiography, provide detailed visualization of scleral staphylomas, allowing for accurate assessment of the extent and depth of scleral thinning. These tools are extremely useful for diagnosing and monitoring the condition, guiding treatment decisions, and detecting complications early.
- Ultrasound Biomicroscopy (UBM): UBM is a high-frequency ultrasound technique that produces detailed images of the eye’s anterior segment, which includes the sclera. UBM is especially useful for determining the extent of scleral thinning and planning surgical interventions as needed. Advances in UBM technology improve image resolution and diagnostic accuracy, allowing for more effective scleral staphyloma management.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of the eye and orbit, allowing you to assess the extent of scleral thinning and the involvement of surrounding tissues. MRI is especially useful in assessing posterior staphylomas and planning complex surgical procedures.
Innovative Surgical Techniques
New surgical techniques are opening up new options for treating scleral staphyloma, improving the safety and efficacy of existing procedures.
- Minimally Invasive Surgery: Advances in minimally invasive surgical techniques are improving the safety and efficacy of treatments for scleral staphyloma. These techniques use smaller incisions and less trauma to the eye, which promotes faster recovery and lowers the risk of complications. Minimally invasive scleral patch grafting and reinforcement techniques are being developed and refined to improve patient outcomes.
- Robotic-Assisted Surgery: Robotic systems are being investigated for use in delicate ocular surgeries, such as those to treat scleral staphylomas. Robotic-assisted surgery improves precision and control, allowing surgeons to perform intricate maneuvers with high accuracy. This technology has the potential to increase the success rate of complex surgical procedures for scleral staphyloma, lower the risk of complications, and improve visual outcomes.
- Scleral Crosslinking: Scleral cross-linking, like corneal cross-linking for keratoconus, seeks to strengthen the scleral collagen fibers and increase tissue rigidity. This procedure involves putting riboflavin (vitamin B2) on the sclera and activating it with UV light. Early research suggests that scleral cross-linking can effectively stabilize the sclera while preventing further thinning and bulging, providing a less invasive alternative to traditional surgical techniques.
Pharmaceutical Innovations
The goal of pharmacological treatments for scleral staphyloma is to develop drugs that can strengthen the sclera and prevent progression.
- Collagen Cross-Linking Agents: In addition to scleral cross-linking, researchers are looking into pharmaceutical agents that can cause collagen cross-linking in the sclera. These agents aim to strengthen scleral collagen fibers, thereby increasing tissue rigidity and stability. Various compounds, including riboflavin and other photosensitizers, are being studied for their potential role in scleral cross-linking.
- Anti-Inflammatory and Anti-Fibrotic Agents: Inflammation and fibrosis can cause scleral thinning and weakening. Anti-inflammatory and anti-fibrotic medications are being tested for their ability to reduce these processes and maintain scleral integrity. Corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and novel anti-fibrotic agents are all being studied for their potential benefits in the treatment of scleral staphyloma.
Personalized Medicine
Personalized medicine involves tailoring treatment strategies to each patient’s unique characteristics, such as genetic makeup, disease profile, and response to therapy. Advances in genomics and molecular diagnostics allow for more precise and targeted approaches to scleral staphyloma treatment.
- Genetic Testing: Genetic testing can identify specific mutations linked to conditions that increase the risk of scleral staphyloma, such as connective tissue disorders. Understanding a patient’s genetic profile enables personalized treatment plans that target the underlying cause of scleral thinning and bulging.
- Biomarker-Guided Therapy: Biomarkers are quantifiable indicators of disease status or treatment outcome. Identifying biomarkers associated with scleral staphyloma progression and treatment efficacy can aid in tailoring therapies to individual patients, improving outcomes while minimizing side effects.
- Precision Therapeutics: Advances in data analytics and machine learning improve the ability to integrate and interpret large datasets, resulting in more precise and effective treatment strategies. Precision therapeutics is the use of detailed patient data to create personalized treatment plans that address each patient’s specific needs.






