Uveitic macular edema (UME) is a complication of uveitis, an inflammatory condition that affects the iris, ciliary body, and choroid. UME primarily affects the macula, the central part of the retina responsible for detailed and sharp vision. When uveitis-related inflammation spreads to the macula, fluid accumulates within the retinal layers, causing swelling and thickening of the macula. This condition can result in significant visual impairment, including blurred vision, distorted central vision, and, in severe cases, vision loss.
UME is a major cause of vision loss in uveitis patients, and it can occur in any type of uveitis, including anterior, intermediate, posterior, and panuveitis. The pathogenesis involves inflammatory mediators breaking down the blood-retinal barrier, allowing fluid to leak into the macular region. Symptoms of UME include difficulty reading, decreased color perception, and blurred central vision.
UME is typically diagnosed through clinical examination and imaging techniques such as optical coherence tomography (OCT), which produces detailed cross-sectional images of the retina that highlight areas of fluid accumulation and macular thickening. Fluorescein angiography (FA) is another technique for visualizing blood flow in the retina and identifying leaks. Understanding the nature and progression of UME is critical for developing effective treatment strategies that preserve and improve vision in affected people.
How to Manage and Treat Uveitic Macular Edema?
The management and treatment of uveitic macular edema requires a multifaceted approach that addresses both the underlying uveitis and the macular edema. The primary goals are to reduce inflammation, prevent additional fluid accumulation, and restore normal macular function in order to improve visual outcomes.
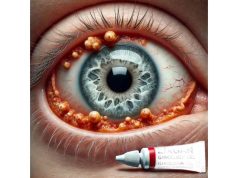
Corticosteroids: Corticosteroids are the foundation of UME treatment due to their potent anti-inflammatory properties. They are available in a variety of forms, including topical eye drops, oral tablets, periocular injections, and intravitreal injections. Topical corticosteroids are commonly used to treat anterior uveitis, whereas periocular and intravitreal injections (such as triamcinolone acetonide) are more effective for posterior segment involvement. Intravitreal corticosteroid implants, such as dexamethasone (Ozurdex) and fluocinolone acetonide (Retisert), offer long-term drug delivery and are useful for chronic conditions.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs can be used as a supplement to corticosteroids or for milder cases of uveitis. They reduce inflammation and can be used topically or systemically.
Immunosuppressive Agents: Patients with chronic or refractory uveitis frequently receive immunosuppressive medications such as methotrexate, azathioprine, mycophenolate mofetil, and cyclosporine. These drugs modulate the immune response and help control inflammation, reducing the need for long-term corticosteroid therapy.
Biologic Agents: Biologics, such as tumor necrosis factor-alpha (TNF-alpha) inhibitors (adalimumab, infliximab) and interleukin inhibitors (tocilizumab), reduce inflammation by targeting specific immune system pathways. They are especially effective in reducing UME in cases of uveitis associated with systemic autoimmune diseases.
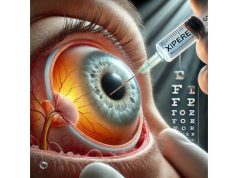
Anti-VEGF Therapy: Vascular endothelial growth factor (VEGF) promotes vascular permeability, which contributes to the development of macular edema. Anti-VEGF agents, including bevacizumab (Avastin), ranibizumab (Lucentis), and aflibercept (Eylea), are commonly used to treat macular edema caused by conditions such as diabetic retinopathy and age-related macular degeneration. These agents may also be effective in UME, reducing fluid leakage and macular thickness.
Laser Photocoagulation: Laser therapy is less commonly used for UME, but it may be considered in cases where focal leakage is visible on fluorescein angiography. Laser photocoagulation aims to seal leaking blood vessels and reduce fluid buildup.
Monitoring and Follow-Up: Regular monitoring of patients with UME is essential for assessing response to treatment and making necessary adjustments. This includes regular visual acuity tests, OCT imaging to monitor macular thickness, and an assessment of inflammation control.
Innovative Treatments for Uveitic Macular Edema
The treatment landscape for uveitic macular edema has changed dramatically with the introduction of cutting-edge innovations. These advancements give patients new hope by increasing efficacy, reducing side effects, and improving overall outcomes. Here are some of the most effective and innovative treatments that have emerged:
**1. Sustained-release intravitreal implants.
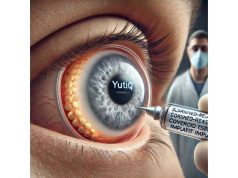
Sustained-release intravitreal implants have transformed the treatment of chronic UME by reducing the number of injections required to control inflammation and macular edema over time.
Dexamethasone Implant (Ozurdex): The Ozurdex implant gradually releases dexamethasone, a potent corticosteroid, to reduce inflammation and macular edema. Clinical trials have shown that patients with UME have significant improvements in visual acuity and macular thickness. The implant is especially useful for patients who have recurrent or chronic macular edema and require ongoing treatment.
Fluocinolone Acetonide Implant (Retisert): The Retisert implant provides fluocinolone acetonide, a corticosteroid, for up to three years. It has demonstrated efficacy in managing chronic uveitis and associated macular edema, reducing the need for frequent interventions. However, possible side effects such as increased intraocular pressure and cataract formation necessitate close monitoring.
2. Novel Biologic Agents
The development of new biologic agents that target specific inflammatory pathways has increased treatment options for UME.
Interleukin Inhibitors: Tocilizumab, an interleukin-6 (IL-6) receptor inhibitor, has shown promise for treating uveitic macular edema, particularly in patients with refractory uveitis. Tocilizumab inhibits IL-6, which reduces inflammation and fluid accumulation in the macula. Clinical trials have shown that tocilizumab therapy improves visual acuity and macular thickness significantly.
Janus Kinase (JAK) Inhibitors: Tofacitinib and ruxolitinib are JAK inhibitors that target intracellular signaling pathways associated with inflammation. These agents have shown efficacy in treating a variety of autoimmune conditions and are being studied for their potential in treating uveitic macular edema. Early research indicates that JAK inhibitors can reduce macular edema and improve visual outcomes in patients with uveitis.
**3. **Advanced Imaging and Diagnostic Tools
Advances in imaging technologies improve UME diagnosis and monitoring, resulting in more precise and personalized treatment strategies.
Optical Coherence Tomography Angiography (OCTA): OCTA generates non-invasive, high-resolution images of the retina and choroidal blood vessels, allowing clinicians to detect and monitor macular edema and associated vascular changes. OCTA can detect areas of capillary non-perfusion, neovascularization, and leakage, allowing for more targeted treatment and disease management.
Ultra-Widefield Imaging: Ultra-widefield imaging captures detailed images of the retina, including peripheral regions that conventional imaging techniques frequently overlook. This technology aids in detecting peripheral retinal inflammation and vascular changes that may contribute to UME, allowing for a more thorough evaluation and management.
**4. *Gene Therapy*
Gene therapy is a promising approach to treating uveitic macular edema because it addresses the underlying genetic causes of inflammation and fluid accumulation.
AAV-Based Gene Therapy: Adeno-associated virus (AAV)-based gene therapy is the process of delivering therapeutic genes to the retina in order to modulate the inflammatory response and reduce macular edema. AAV-based therapies that target specific genes implicated in uveitis and macular edema are currently under development. Preclinical studies have yielded promising results, and clinical trials are currently underway to determine the safety and efficacy of these gene therapies.
CRISPR-Cas9 Gene Editing: CRISPR-Cas9 technology allows for precise genome editing to correct genetic mutations that cause uveitis and macular edema. This cutting-edge approach has the potential to provide long-term control and even cure UME by addressing the underlying cause of inflammation. While still in its early stages, CRISPR-Cas9 gene editing represents a promising frontier in ocular therapy.
5. Combination therapies
Combining different treatment modalities can improve the effectiveness of UME management and provide synergistic advantages.
Anti-VEGF and Steroid Combination: Combining anti-VEGF agents with corticosteroids has demonstrated greater efficacy in reducing macular edema than either treatment alone. This approach takes advantage of anti-VEGF therapy’s anti-permeability effects as well as corticosteroids’ anti-inflammatory properties to provide comprehensive control of UME. Clinical trials have shown that combination therapy improves visual outcomes and reduces macular thickness.
Immunosuppressive and Biologic Combination: Combining traditional immunosuppressive agents with biologic therapies can improve control of uveitis and macular edema. This strategy allows for lower doses of each medication, lowering the risk of adverse effects while maintaining therapeutic efficacy. For example, combining methotrexate and adalimumab has improved outcomes in patients with refractory uveitis and macular edema.
6. Novel Drug Delivery Systems
Drug delivery system innovations are improving UME treatment precision and duration.
Suprachoroidal Drug Delivery: Delivering drugs to the suprachoroidal space, located
between the sclera and choroid, provides targeted therapy with minimal systemic exposure. Suprachoroidal delivery of corticosteroids and other anti-inflammatory agents has shown promise in treating uveitic macular edema due to its sustained drug release and increased bioavailability. Early studies show that this approach can effectively reduce macular edema and improve visual outcomes while causing fewer side effects.
Nanoparticle-Based Delivery: Nanoparticles can encapsulate therapeutic agents and deliver them directly to the retina, thereby increasing drug penetration and retention. This technology enables controlled drug release, reducing the number of injections required and increasing patient compliance. To treat UME, researchers are developing nanoparticle-based delivery systems for corticosteroids, anti-VEGF agents, and immunosuppressive drugs.
**7. *Stem Cell Therapy*
Stem cell therapy is a regenerative approach to treating uveitic macular edema that repairs damaged retinal tissues and restores normal functionality.
Mesenchymal Stem Cells (MSCs): MSCs are anti-inflammatory and immunomodulatory, which can help reduce inflammation and promote tissue repair in the retina. According to research, intravitreal injections of MSCs can reduce macular edema and improve visual acuity in uveitis patients. The ongoing research aims to improve the delivery and efficacy of MSC therapy for UME.
Retinal Pigment Epithelium (RPE) Cells: RPE cells are critical to maintaining retinal health and function. Transplanting RPE cells derived from stem cells can help restore the blood-retinal barrier and reduce fluid accumulation in the macula. Early clinical trials have shown that RPE cell therapy can improve visual outcomes in patients with retinal diseases, including UME.
8. AI and Machine Learning
AI and machine learning are revolutionizing the diagnosis and treatment of uveitic macular edema by providing advanced analytical tools and predictive models.
AI-Powered Diagnostics: AI algorithms can examine OCT and other imaging data to detect subtle changes in the retina and predict the progression of macular edema. These tools help clinicians make accurate diagnoses and create personalized treatment plans. AI can also help identify patients at high risk of developing UME, allowing for early intervention and better outcomes.
Predictive Analytics: Machine learning models can predict patient responses to various treatments using a variety of clinical and imaging data. This information enables clinicians to choose the most effective therapies and adjust treatment plans as needed. Predictive analytics can also detect potential side effects and complications, which improves patient safety and treatment.
**9. *Personalized Medicine*
Personalized medicine entails developing treatment plans based on a patient’s genetic, molecular, and clinical profile.
Genetic Testing: Genetic testing can detect specific mutations and biomarkers linked to uveitis and macular edema, guiding the choice of targeted therapies. For example, identifying patients with specific HLA genotypes can aid in predicting their response to immunosuppressive agents and biologics, allowing for more effective and personalized treatment.
Biomarker-Guided Therapy: The use of biomarkers to track disease activity and treatment response is becoming more important in UME management. Biomarkers such as cytokine levels, vascular permeability factors, and genetic markers can help to understand the underlying causes of macular edema and guide treatment adjustments.
10. Integrated Medicine
Integrative medicine combines conventional and alternative therapies to provide comprehensive care for patients suffering from uveitic macular edema.
Nutritional Interventions: Consuming anti-inflammatory foods and antioxidants can help improve overall eye health and reduce inflammation. Omega-3 fatty acids, vitamins C and E, and lutein are all supplements that may help manage macular edema and improve vision. Nutritional counseling can be an important component of an overall treatment plan for UME.
Mind-Body Practices: Yoga, meditation, and Tai Chi can help manage stress and improve overall well-being, potentially benefiting uveitic macular edema. These mind-body techniques can be combined with an integrative treatment plan to improve both mental and physical health.
Herbal and Complementary Therapies: Herbal remedies and complementary therapies, such as acupuncture and homeopathy, may have additional benefits for UME management. While the scientific evidence for some of these therapies is still evolving, they can provide patients with supportive care and improve their quality of life.