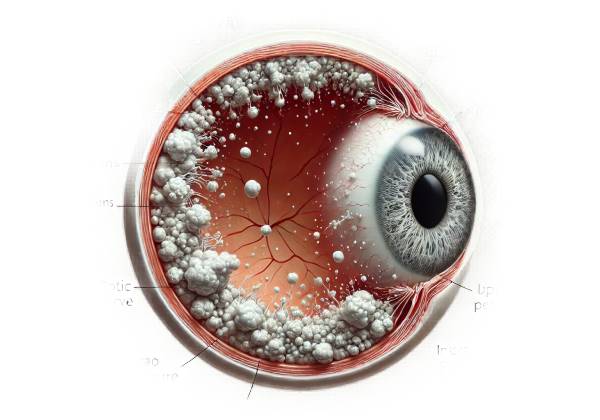
Pseudoexfoliation glaucoma (PXG) is a type of secondary open-angle glaucoma associated with pseudoexfoliation syndrome (PXF or PEX). PXF is a systemic condition characterized by the accumulation of abnormal extracellular fibrillar material in various tissues throughout the body, most notably the anterior segment of the eye. The lens, iris, ciliary body, and trabecular meshwork are all common locations for this material. PXG occurs when this material obstructs the trabecular meshwork, causing increased intraocular pressure (IOP) and subsequent optic nerve damage.
Pathophysiology
PXG’s pathogenesis is complex, involving both genetic and environmental factors. The primary abnormality in PXF is the production and accumulation of fibrillar extracellular material, which preferentially targets the anterior segment of the eye. This pseudoexfoliative material’s exact molecular composition is unknown, but it is thought to be made up of basement membrane components, elastic microfibrils, and other proteins.
- Genetic Factors: Several genetic loci have been linked to the development of PXF, the most significant being the LOXL1 gene. Variants in this gene are strongly associated with PXF and PXG, but the presence of these genetic variations does not ensure disease development, implying a multifactorial etiology.
- Environmental Factors: Geographic location, ultraviolet light exposure, and dietary habits may all contribute to the risk of developing PXF and PXG. Studies have found higher prevalence rates in certain populations, such as those in Scandinavian countries, implying that environmental factors play a role.
- Trabecular Meshwork Dysfunction: An accumulation of pseudoexfoliative material in the trabecular meshwork obstructs aqueous humor outflow, resulting in elevated IOP. Over time, the elevated pressure damages the optic nerve, resulting in the characteristic glaucomatous changes seen in PXG.
- Oxidative Stress and Inflammation: Both oxidative stress and inflammation are thought to play a role in the development of PXG. These factors may increase the production of pseudoexfoliative material and promote cellular dysfunction within the trabecular meshwork.
Epidemiology
Pseudoexfoliation glaucoma is a major cause of secondary open-angle glaucoma worldwide, with different prevalence rates depending on geography and ethnicity. PXF is the most commonly identified cause of secondary open-angle glaucoma.
- Prevalence: PXF becomes more common in people over the age of 60. In some populations, up to 30% of people over the age of 60 have PXF, with approximately 30% developing PXG.
- Geographic Variation: The condition is more common in certain geographic regions, particularly Scandinavian countries, where the prevalence can be as high as 20% in elderly people. In contrast, it is less common among African and Asian populations.
- Gender Differences: PXF and PXG are slightly more common in women than in men, but the reason for this gender disparity is unclear.
Clinical Presentation
PXG can have a wide range of clinical manifestations, and the condition frequently progresses gradually. Many patients with PXF are asymptomatic until significant glaucoma develops. Key clinical characteristics include:
- Elevated Intraocular Pressure: One of the most common symptoms of PXG is high IOP, which can fluctuate significantly. Spikes in IOP are common and can cause rapid progression of optic nerve damage.
- Characteristic Ocular Findings: The presence of pseudoexfoliative material on ocular structures is an important diagnostic indicator. This material is usually visible as flaky, white deposits on the lens capsule, pupil margin, and other anterior segment structures. Gonioscopy frequently detects similar material in the trabecular meshwork and angle structures.
- Optic Nerve Damage: As with other types of glaucoma, PXG causes progressive optic neuropathy. Patients may present with visual field defects, particularly in peripheral vision, which can progress to central vision loss if not treated.
- Iris Changes: The iris may show signs of atrophy, and transillumination defects are frequently visible. These changes may help distinguish PXG from other types of glaucoma.
- Zonular Weakness: Pseudoexfoliative material can build up on the lens zonules, weakening them and increasing the likelihood of lens subluxation or dislocation. This can cause complications with cataract surgery and other intraocular procedures.
Differential Diagnosis
Distinguishing PXG from other types of glaucoma is critical for effective treatment. Differential diagnosis includes:
- Primary Open-Angle Glaucoma (POAG): Both PXG and POAG exhibit open angles and optic nerve damage. PXG, on the other hand, is defined by the presence of pseudoexfoliative material, fluctuating IOP, and faster disease progression.
- Normal-Tension Glaucoma (NTG) causes optic nerve damage at normal IOP levels. While NTG can coexist with PXF, it lacks the elevated IOP and pseudoexfoliative material found in PXG.
- Pigmentary Glaucoma is characterized by the dispersion of pigment granules from the iris, which can obstruct the trabecular meshwork. Pigmentary glaucoma is more common in younger people and is associated with a different pattern of trabecular meshwork pigmentation than PXG.
- Angle-Closure Glaucoma: Unlike PXG, angle-closure glaucoma causes a narrow or closed anterior chamber angle, resulting in sudden increases in IOP. PXF may coexist with angle-closure mechanisms, particularly in hyperopic eyes, complicating the clinical picture.
- Secondary Open-Angle Glaucomas: Other causes of secondary open-angle glaucoma, such as trauma, inflammation, or neovascularization, should be considered. Each has unique clinical characteristics and underlying causes that distinguish it from PXG.
Complications
If not managed properly, PXG can cause a number of serious complications:
- Progressive Vision Loss: Irreversible vision loss due to optic nerve damage is the most serious complication of PXG. This usually starts with peripheral vision loss and can progress to central vision loss if not treated.
- Cataract Formation: Patients with PXG have a higher risk of developing cataracts, possibly due to the associated oxidative stress and inflammation. Cataract surgery in these patients can be difficult due to zonular weakness.
- Lens Subluxation/Dislocation: The buildup of pseudoexfoliative material on the lens zonules can weaken them, increasing the risk of lens subluxation or dislocation, which can cause acute visual disturbances and complications during cataract surgery.
- Intraocular Surgery Complications: The presence of pseudoexfoliative material can cause complications during intraocular surgeries such as cataract extraction or glaucoma filtration surgery. Surgeons should be aware of the increased risk of zonular instability and the possibility of postoperative complications.
Prognosis
The prognosis for patients with PXG varies according to the stage of the disease, the effectiveness of IOP control, and the patient’s adherence to treatment. Early detection and rigorous management of intraocular pressure (IOP) are critical for maintaining vision. However, PXG is generally more aggressive than primary open-angle glaucoma, necessitating surgical intervention and posing a higher risk of visual impairment.
Diagnostic methods
A comprehensive clinical evaluation, imaging studies, and specialized tests to accurately assess intraocular pressure (IOP), optic nerve health, and the presence of pseudoexfoliative material are required to diagnose pseudoexfoliation glaucoma (PXG). Early and accurate diagnosis is critical for successful management and prevention of vision loss.
Clinical Examination
The first step in diagnosing PXG is a comprehensive clinical examination by an ophthalmologist. The key components of the clinical assessment are:
- Visual Acuity Testing: Measuring visual acuity determines the extent of vision loss and serves as a baseline for tracking disease progression and treatment response.
- Slit-Lamp Biomicroscopy: This examination provides a detailed view of the anterior segment of the eye. Pseudoexfoliative material is visible as flaky white deposits on the lens capsule, pupil margin, and other anterior segment structures. This is a defining characteristic of PXF and PXG.
- Intraocular Pressure Measurement: IOP measurement is critical in diagnosing glaucoma. Several methods are available, including Goldmann applanation tonometry, which is considered the gold standard. PXG is characterized by elevated IOP, which can fluctuate significantly.
- Gonioscopy: Gonioscopy is a procedure that examines the eye’s anterior chamber angle. It distinguishes open-angle glaucoma from angle-closure glaucoma and detects pseudoexfoliative material in the trabecular meshwork and angle structures.
- Fundoscopic Examination: Direct or indirect ophthalmoscopy of the optic nerve head can reveal glaucomatous changes such as increased cupping, thinning of the neuroretinal rim, and other signs of optic neuropathy.
Imaging Studies
Imaging studies provide detailed information on the structural changes associated with PXG and can help monitor disease progression.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve head. It aids in determining the thickness of the retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC), both of which are typically thinner in glaucoma.
- Heidelberg Retinal Tomography (HRT) is a laser imaging technique that produces a three-dimensional topographic map of the optic nerve head. It measures optic disc parameters like cup-to-disc ratio and rim area, which are important for diagnosing and monitoring glaucomatous changes in PXG.
- Scanning Laser Polarimetry (SLP): SLP determines the thickness of the RNFL by measuring changes in the polarization of reflected laser light. This technique is useful for detecting early structural changes in the optic nerve.
Specialized Tests
Additional tests to further evaluate and support the diagnosis of PXG:
- Visual Field Testing: Automated perimetry, such as the Humphrey Visual Field Analyzer, maps the patient’s visual field by presenting light stimuli in different locations and recording the responses. This test detects common glaucomatous visual field defects like arcuate scotomas, nasal steps, and paracentral defects.
- Electroretinography (ERG): ERG assesses retinal cells’ electrical responses to light stimuli. It provides information on retinal function and aids in distinguishing PXG from other retinal conditions that present similar symptoms.
- Ultrasound Biomicroscopy (UBM): UBM captures high-resolution images of the anterior segment structures, such as the iris, ciliary body, and lens zonules. It aids in determining zonular integrity and detecting any abnormalities associated with pseudoexfoliative material accumulation.
Effective Pseudoexfoliation Glaucoma Therapies
Managing pseudoexfoliation glaucoma (PXG) entails a combination of medical, laser, and surgical interventions to reduce intraocular pressure (IOP) and prevent further optic nerve damage. The severity of the condition, the patient’s response to therapies, and individual patient factors all influence treatment decisions.
Medical Management
Medications are frequently the first line of treatment for PXG, and they aim to lower IOP by decreasing aqueous humor production or increasing its outflow. The main classes of medications are:
- Prostaglandin Analogues: Drugs like latanoprost, bimatoprost, and travoprost stimulate uveoscleral outflow and are extremely effective at lowering IOP. They are usually given once a day and are generally well tolerated.
- Beta-Blockers: Timolol and betaxolol inhibit aqueous humor production by blocking beta-adrenergic receptors in the ciliary body. They are typically given twice daily and can be used alone or in conjunction with other medications.
- Alpha Agonists: Drugs like brimonidine reduce aqueous humor production while increasing uveoscleral outflow. They are given twice a day and can be combined with other IOP-lowering drugs.
- Carbonic Anhydrase Inhibitors: These medications, which include dorzolamide and brinzolamide, suppress aqueous humor production by inhibiting the enzyme carbonic anhydrase. They can be used topically or systemically, with topical administration being more common due to fewer systemic side effects.
- Rho Kinase Inhibitors: A relatively new class of medications, such as netarsudil, that increase trabecular outflow while decreasing IOP. These can be used separately or in conjunction with other treatments.
Combination therapies involving two or more classes of medications are frequently required to achieve adequate IOP control in PXG patients.
Laser Therapy
Laser treatments can be an effective alternative or adjunct to medical therapy, especially for patients who have inadequate IOP control or medication intolerance. The main laser treatments for PXG are:
- Selective Laser Trabeculoplasty (SLT) uses a low-energy laser to target the trabecular meshwork and improve aqueous outflow. It is a minimally invasive procedure that can be repeated as needed and is commonly used when medications are insufficient.
- Argon Laser Trabeculoplasty (ALT): ALT, like SLT, uses an argon laser to treat the trabecular meshwork, but with more thermal energy. It can effectively lower IOP, but it is more likely to cause thermal damage than SLT.
Surgical Interventions
Surgery is considered for PXG patients who do not achieve adequate IOP control with medications or laser therapy. The most common surgical procedures are:
- Trabeculectomy: This procedure creates a new drainage pathway for aqueous humor by removing a portion of the trabecular meshwork and forming a filtration bleb. Trabeculectomy is highly effective in lowering IOP, but it has risks such as infection, scarring, and vision changes.
- Glaucoma Drainage Devices (GDDs): Also referred to as aqueous shunts, these devices allow aqueous humor to drain through an implanted tube. Examples include the Ahmed, Baerveldt, and Molteno implants. GDDs are frequently used in patients who have failed trabeculectomy or have a specific type of glaucoma.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures, including the iStent, XEN Gel Stent, and Hydrus Microstent, provide less invasive options with shorter recovery times and fewer complications. They are usually considered for patients with mild to moderate PXG.
Supportive Measures
In addition to direct IOP-lowering treatments, supportive measures play an important role in managing PXG.
- Regular Monitoring: Frequent follow-up appointments are required to monitor IOP, optic nerve health, and visual fields. Early detection of disease progression enables timely treatment adjustments.
- Patient Education: Educating patients about the nature of PXG, the importance of treatment adherence, and recognizing symptoms of disease progression is critical for successful management.
- Lifestyle Modifications: Promoting a healthy lifestyle, such as regular exercise, a balanced diet, and quitting smoking, can improve overall eye health and potentially lower the risk of glaucoma progression.
Trusted Resources and Support
Books
- “Glaucoma: A Patient’s Guide to the Disease” by Graham E. Trope: This book provides comprehensive information on glaucoma, including its diagnosis, treatment options, and patient management strategies, with insights into secondary glaucomas like PXG.
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care” by Paul N. Schacknow and John R. Samples: This detailed resource covers various aspects of glaucoma, offering practical advice for clinicians and valuable information for patients.
Organizations
- Glaucoma Research Foundation (GRF): The GRF provides extensive information on glaucoma research, treatment options, and patient support. They offer resources specifically addressing secondary glaucomas like PXG. GRF Website
- American Academy of Ophthalmology (AAO): The AAO offers a wealth of resources, guidelines, and continuing education for ophthalmologists and patients dealing with glaucoma, including PXG. AAO Website
- National Eye Institute (NEI): The NEI conducts and supports research on eye diseases and provides comprehensive educational resources on various forms of glaucoma, including pseudoexfoliation glaucoma. NEI Website










