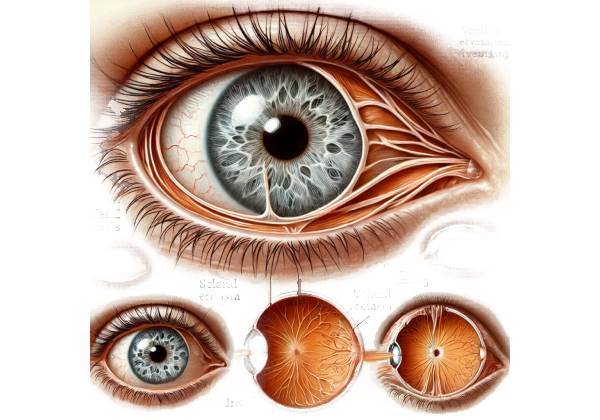
Scleral ectasia is a rare and serious ocular condition characterized by the abnormal thinning and outward bulging of the sclera, the white, tough, outer layer of the eye that provides structural support and protection. This condition can lead to significant visual impairment and, if left untreated, can progress to severe complications, including globe rupture, which can threaten vision and, in some cases, the integrity of the eye itself.
The sclera is composed primarily of collagen fibers arranged in a complex, interwoven pattern that gives it strength and rigidity. In scleral ectasia, this structural integrity is compromised due to the degeneration or weakening of the collagen matrix, leading to localized or diffuse thinning of the scleral tissue. This thinning reduces the sclera’s ability to withstand the intraocular pressure (IOP) exerted from within the eye, resulting in the outward bulging or ectasia of the sclera.
Etiology and Risk Factors
Scleral ectasia can occur as a primary condition or secondary to other underlying ocular or systemic diseases. The etiology of scleral ectasia can vary, and in many cases, it remains idiopathic, meaning the exact cause is unknown. However, several risk factors and associated conditions have been identified:
- Congenital Disorders: Some cases of scleral ectasia are associated with congenital connective tissue disorders such as Ehlers-Danlos syndrome, Marfan syndrome, and osteogenesis imperfecta. These genetic conditions are characterized by defects in collagen production or structure, leading to weakened connective tissues throughout the body, including the sclera.
- Inflammatory Conditions: Chronic inflammation of the sclera, known as scleritis, can lead to scleral ectasia. Inflammation can cause the breakdown of the collagen fibers within the sclera, resulting in thinning and weakening of the tissue. Autoimmune diseases such as rheumatoid arthritis, granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis), and systemic lupus erythematosus are often associated with scleritis and, consequently, scleral ectasia.
- Surgical Trauma: Scleral ectasia can also develop as a complication of ocular surgery, particularly procedures that involve significant manipulation of the sclera, such as scleral buckling for retinal detachment or pterygium excision. In some cases, excessive thinning of the sclera may occur at the site of the surgical intervention, leading to ectasia.
- High Myopia: Patients with high myopia (nearsightedness) are at increased risk for scleral ectasia. In high myopia, the eye is elongated, which places additional stress on the scleral tissue. Over time, this can lead to the thinning and bulging of the sclera, particularly in the posterior part of the eye, resulting in posterior staphyloma, a form of scleral ectasia.
- Infectious Causes: Although rare, certain infections can lead to scleral ectasia. Severe bacterial or fungal infections that invade the scleral tissue can cause necrosis and thinning, leading to ectasia. Conditions such as infectious scleritis or scleral abscesses are potential precursors to scleral ectasia.
- Idiopathic Cases: In many instances, scleral ectasia develops without any identifiable underlying cause or predisposing condition. These idiopathic cases are challenging to diagnose and manage, as the etiology remains unclear.
Clinical Presentation and Symptoms
The clinical presentation of scleral ectasia can vary depending on the severity of the condition, the underlying cause, and the specific location of the ectasia. In the early stages, scleral ectasia may be asymptomatic, particularly if the thinning is localized and does not affect the adjacent ocular structures. However, as the condition progresses, patients may experience a range of symptoms that can significantly impact their vision and overall eye health.
- Visual Disturbances: One of the most common symptoms of scleral ectasia is a gradual decline in visual acuity. This is often due to the distortion of the eye’s normal shape, which can lead to irregular astigmatism and refractive errors. Patients may experience blurred vision, double vision (diplopia), or difficulty focusing on objects at various distances. In cases where scleral ectasia is associated with high myopia or posterior staphyloma, patients may also report symptoms related to myopic degeneration, such as floaters or flashes of light.
- Ocular Discomfort: As scleral ectasia progresses, patients may experience ocular discomfort or pain, particularly if the ectasia is associated with an inflammatory condition such as scleritis. The pain can range from mild to severe and may be exacerbated by eye movements or changes in lighting conditions. In some cases, the sclera may become visibly red or inflamed, further contributing to discomfort.
- Globe Deformation: In advanced cases of scleral ectasia, the affected eye may develop a visible deformation or bulging of the globe. This can be particularly pronounced in cases of posterior staphyloma, where the posterior segment of the eye becomes elongated and protrudes outward. This abnormal globe shape can lead to significant cosmetic concerns and may interfere with the proper function of the eyelids.
- Increased Risk of Globe Rupture: One of the most serious complications of scleral ectasia is the increased risk of globe rupture. As the sclera thins, it becomes more susceptible to rupture, particularly in response to trauma or elevated intraocular pressure. Globe rupture is a medical emergency that can lead to irreversible vision loss and may require immediate surgical intervention to repair the damage.
- Secondary Glaucoma: In some cases, scleral ectasia can lead to secondary glaucoma, a condition characterized by increased intraocular pressure that damages the optic nerve. This can occur if the deformation of the globe disrupts the normal drainage of aqueous humor, leading to a buildup of fluid within the eye. Glaucoma associated with scleral ectasia can further exacerbate visual loss and may be challenging to manage.
Anatomical Locations of Scleral Ectasia
Scleral ectasia can occur in different regions of the sclera, and the location of the ectasia can influence the clinical presentation and associated complications:
- Anterior Scleral Ectasia: This form of scleral ectasia involves the thinning and bulging of the anterior sclera, which is the part of the sclera visible when looking directly at the eye. Anterior scleral ectasia may be associated with a history of scleritis or surgical trauma. In some cases, it may also involve the adjacent cornea, leading to a condition known as keratoglobus, where both the cornea and sclera become abnormally thin and bulge outward.
- Posterior Scleral Ectasia: Posterior scleral ectasia, also known as posterior staphyloma, occurs in the back of the eye and is often associated with high myopia. This form of ectasia is particularly concerning because it can affect the macula, the central part of the retina responsible for detailed vision. Posterior scleral ectasia can lead to significant visual impairment and may be associated with other complications, such as retinal detachment or myopic degeneration.
- Circumferential Scleral Ectasia: In some cases, scleral ectasia may occur circumferentially, affecting a broad region of the sclera. This can lead to a generalized weakening of the scleral tissue and may be associated with systemic connective tissue disorders.
Epidemiology and Risk Factors
Scleral ectasia is a rare condition, and its exact prevalence is not well established. It can occur at any age but is more commonly diagnosed in middle-aged to older adults. The condition is often associated with underlying systemic or ocular conditions, particularly connective tissue disorders, inflammatory diseases, and high myopia.
Patients with a history of scleritis, particularly necrotizing scleritis, are at increased risk for developing scleral ectasia. Additionally, individuals with congenital connective tissue disorders such as Ehlers-Danlos syndrome or Marfan syndrome are more prone to scleral thinning and ectasia due to the inherent weakness of their collagen fibers.
High myopia is a significant risk factor for posterior scleral ectasia, as the elongated shape of the eye in myopic patients places additional stress on the scleral tissue. This is particularly true in cases of degenerative myopia, where the risk of posterior staphyloma is elevated.
Understanding the underlying risk factors and early signs of scleral ectasia is crucial for timely diagnosis and intervention. As the condition can lead to serious complications, including vision loss and globe rupture, early detection and management are essential for preserving eye health.
Diagnostic Methods
Diagnosing scleral ectasia involves a combination of clinical evaluation, imaging studies, and, in some cases, specialized tests to assess the extent of scleral thinning and the risk of associated complications. The following diagnostic methods are commonly used to evaluate scleral ectasia:
Clinical Examination
A thorough clinical examination by an ophthalmologist is the first step in diagnosing scleral ectasia. The examination typically includes:
- Visual Acuity Test: This test measures the patient’s ability to see at various distances and helps assess the impact of scleral ectasia on vision. Changes in visual acuity, particularly if associated with irregular astigmatism or myopia, may indicate the presence of scleral ectasia.
- Slit-Lamp Biomicroscopy: The slit-lamp examination allows the ophthalmologist to closely examine the anterior segment of the eye, including the sclera, cornea, and anterior chamber. This examination can reveal signs of scleral thinning, inflammation, or bulging. In cases of anterior scleral ectasia, the affected area may appear thinned or translucent under slit-lamp illumination.
- Fundoscopy: Fundoscopy involves examining the back of the eye, including the retina, optic disc, and posterior sclera. Fundoscopy is particularly useful in assessing posterior scleral ectasia (posterior staphyloma), where the back of the eye may appear elongated or bulging. This examination can also help detect associated retinal abnormalities, such as retinal detachment or myopic degeneration, which are common in high myopia with posterior scleral ectasia.
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) is a non-invasive imaging technique that provides high-resolution cross-sectional images of the retina and the posterior segment of the eye. OCT is particularly valuable in diagnosing and monitoring scleral ectasia, especially posterior scleral ectasia, as it allows for detailed visualization of the retinal layers and the underlying scleral tissue.
- Macular OCT: In cases of posterior scleral ectasia, macular OCT can reveal the extent of scleral thinning and the presence of staphyloma. It can also detect any associated complications, such as macular holes, epiretinal membranes, or retinal detachment. The information obtained from macular OCT is crucial for assessing the severity of the condition and planning appropriate management strategies.
- Anterior Segment OCT: Anterior segment OCT is used to evaluate the anterior sclera and cornea in cases of anterior scleral ectasia. This imaging modality can help assess the depth and extent of scleral thinning and identify any involvement of the cornea, particularly in conditions like keratoglobus.
Ultrasound Biomicroscopy (UBM)
Ultrasound Biomicroscopy (UBM) is an imaging technique that uses high-frequency sound waves to create detailed images of the anterior segment of the eye, including the sclera, ciliary body, and anterior chamber angle. UBM is particularly useful for evaluating anterior scleral ectasia, as it provides detailed information about the thickness and structure of the sclera.
- Scleral Thickness Measurement: UBM can measure scleral thickness in various regions of the eye, allowing the ophthalmologist to assess the extent of scleral thinning and identify areas at risk for ectasia. This measurement is critical for determining the severity of the condition and the potential risk of complications such as globe rupture.
- Assessment of Ciliary Body and Anterior Chamber: UBM can also evaluate the ciliary body and anterior chamber, helping to identify any abnormalities that may be associated with scleral ectasia, such as anterior uveitis or secondary glaucoma.
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is a non-invasive imaging technique that provides detailed images of the eye and orbit. MRI is particularly useful for evaluating posterior scleral ectasia, as it allows for a comprehensive assessment of the posterior segment and the surrounding orbital structures.
- Assessment of Posterior Staphyloma: MRI can provide detailed images of the posterior sclera, helping to assess the size and extent of posterior staphyloma. It can also identify any associated abnormalities in the optic nerve or surrounding orbital tissues.
- Evaluation of Extraocular Structures: MRI is also useful for evaluating the extraocular muscles, optic nerve, and orbital fat, particularly in cases where scleral ectasia is associated with other ocular or orbital conditions.
Corneal Topography
Corneal topography is a non-invasive imaging technique that maps the surface curvature of the cornea. While it is primarily used to diagnose and monitor corneal ectatic disorders such as keratoconus, it can also be useful in cases of scleral ectasia that involve the anterior segment of the eye.
- Detection of Irregular Astigmatism: Corneal topography can detect irregular astigmatism, which is a common finding in patients with scleral ectasia. This information can help guide refractive correction and monitor the progression of the condition.
- Evaluation of Corneal Involvement: In cases where scleral ectasia is associated with corneal involvement, such as keratoglobus, corneal topography can provide detailed information about the shape and thickness of the cornea.
B-Scan Ultrasonography
B-scan ultrasonography is a diagnostic imaging technique that uses sound waves to create cross-sectional images of the eye. It is particularly useful in cases where the view of the posterior segment is obscured by media opacities, such as cataracts or vitreous hemorrhage.
- Evaluation of Posterior Segment: B-scan ultrasonography can assess the posterior segment of the eye, including the sclera, retina, and choroid. It is useful for detecting posterior scleral ectasia, retinal detachment, and other associated abnormalities.
- Detection of Intraocular Masses: B-scan ultrasonography can also detect intraocular masses or lesions that may be associated with scleral ectasia, such as scleral tumors or choroidal neoplasms.
Scleral Ectasia Management
The management of scleral ectasia is multifaceted and depends on the severity of the condition, the underlying cause, and the presence of any associated complications. The primary goals of treatment are to stabilize the sclera, prevent further thinning and bulging, manage symptoms, and protect against potential complications such as globe rupture or vision loss. The treatment approach can vary from conservative management and monitoring to more invasive surgical interventions, depending on the individual case.
Observation and Monitoring
In cases of mild scleral ectasia, particularly when the condition is asymptomatic and not associated with significant risk factors, a conservative approach with regular monitoring may be appropriate. Patients are typically advised to undergo routine ophthalmic examinations, including visual acuity tests, slit-lamp biomicroscopy, and imaging studies such as OCT or UBM, to monitor the progression of scleral thinning and detect any early signs of complications.
Regular monitoring is crucial for detecting changes in scleral thickness, globe shape, or the development of associated conditions such as secondary glaucoma or retinal detachment. In patients with stable or slowly progressing ectasia, this approach can help avoid unnecessary interventions while ensuring timely treatment if the condition worsens.
Medical Management
Medical management of scleral ectasia primarily focuses on treating any underlying inflammatory or infectious conditions that may be contributing to scleral thinning. In cases where scleral ectasia is associated with scleritis or other inflammatory disorders, systemic corticosteroids or immunosuppressive agents may be prescribed to reduce inflammation and prevent further damage to the sclera.
- Corticosteroids: Oral or topical corticosteroids are often the first-line treatment for scleritis-associated scleral ectasia. These medications help to control inflammation and reduce the risk of scleral thinning and ectasia progression. The dosage and duration of corticosteroid therapy are tailored to the severity of the inflammation and the patient’s response to treatment.
- Immunosuppressive Agents: In cases of chronic or refractory inflammation, where corticosteroids alone are insufficient, immunosuppressive agents such as methotrexate, azathioprine, or cyclosporine may be used. These medications help to modulate the immune response and reduce inflammation, thereby protecting the sclera from further thinning.
- Antibiotics or Antifungals: If scleral ectasia is associated with an infectious cause, such as bacterial or fungal scleritis, appropriate antimicrobial therapy is essential. Antibiotics or antifungal agents may be administered systemically or topically, depending on the severity of the infection.
Surgical Interventions
In more advanced cases of scleral ectasia, where there is significant thinning, globe deformation, or a high risk of complications such as globe rupture, surgical intervention may be necessary. Several surgical techniques can be employed to reinforce the sclera and stabilize the globe:
- Scleral Patch Grafting: Scleral patch grafting involves placing a graft, usually made from donor sclera or synthetic material, over the area of thinning to reinforce the sclera and prevent further bulging. This procedure is particularly useful in cases of localized scleral ectasia or where there is an imminent risk of rupture. The graft is typically sutured into place and covered with conjunctiva to ensure proper healing.
- Scleral Reinforcement Surgery: Scleral reinforcement surgery involves placing a reinforcing material, such as a band or strip, around the circumference of the globe to provide additional support to the sclera. This technique is often used in cases of posterior scleral ectasia (posterior staphyloma) associated with high myopia. The reinforcing material helps to stabilize the posterior segment and reduce the risk of further deformation or complications.
- Lamellar Scleral Grafting: In cases where the scleral thinning is more extensive, lamellar scleral grafting may be performed. This procedure involves replacing the thinned scleral tissue with a thicker graft, which is sutured into place to restore the integrity of the sclera. Lamellar grafting is a more invasive procedure and is typically reserved for severe cases where other surgical options are insufficient.
- Amniotic Membrane Transplantation: In some cases, amniotic membrane transplantation may be used as an adjunctive treatment to promote healing and reduce inflammation after scleral surgery. The amniotic membrane is placed over the surgical site and helps to support tissue regeneration and reduce the risk of postoperative complications.
Management of Associated Complications
Scleral ectasia can lead to several complications that require specific management strategies:
- Globe Rupture: Globe rupture is a medical emergency that requires immediate surgical repair to prevent permanent vision loss. The surgical approach depends on the extent and location of the rupture, but typically involves suturing the ruptured area, reinforcing the sclera, and managing any associated intraocular damage.
- Secondary Glaucoma: Secondary glaucoma can develop in patients with scleral ectasia, particularly if the deformation of the globe affects the normal drainage of aqueous humor. Management of secondary glaucoma may involve medications to reduce intraocular pressure, laser therapy, or surgical procedures such as trabeculectomy or tube shunt surgery.
- Retinal Detachment: Retinal detachment is a potential complication of posterior scleral ectasia. Treatment typically involves surgical reattachment of the retina, which may include procedures such as scleral buckling, vitrectomy, or pneumatic retinopexy.
Visual Rehabilitation
For patients with significant visual impairment due to scleral ectasia, visual rehabilitation is an important aspect of management. This may include the use of corrective lenses, contact lenses, or low vision aids to optimize remaining vision. In cases where irregular astigmatism is present, rigid gas-permeable contact lenses or custom scleral lenses may be recommended to improve visual acuity.
Patients may also benefit from low vision services, including occupational therapy and assistive devices, to help them adapt to their visual limitations and maintain independence in daily activities.
Trusted Resources and Support
Books
- “Ocular Surgery: Scleral Surgery and Related Procedures” by Jeffrey S. Cohen and Peter J. Dolman: This book provides an in-depth overview of surgical techniques and management strategies for conditions affecting the sclera, including scleral ectasia. It is a valuable resource for ophthalmologists and surgeons.
- “Diseases of the Sclera and Episclera” by Christopher J. Rapuano: This book covers a wide range of scleral diseases, offering insights into their diagnosis, treatment, and management, making it a comprehensive resource for understanding conditions like scleral ectasia.
Organizations
- American Academy of Ophthalmology (AAO): The AAO provides extensive resources and guidelines for the diagnosis and management of ocular conditions, including scleral ectasia. It offers educational materials for both healthcare professionals and patients.
- National Eye Institute (NEI): Part of the National Institutes of Health (NIH), the NEI provides reliable information on eye diseases, including scleral ectasia, and supports research aimed at improving the understanding and treatment of ocular conditions.
- Foundation Fighting Blindness: This organization offers resources and support for patients with various ocular conditions that can lead to vision loss, including scleral ectasia. It provides access to clinical trials, research updates, and patient support networks.










