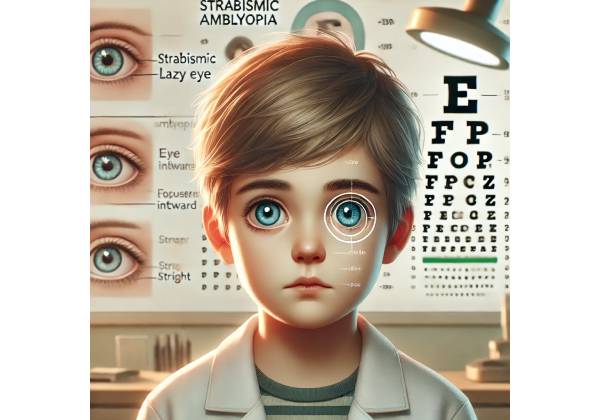
What is Strabismic Amblyopia?
Strabismic amblyopia, also known as “lazy eye,” is a type of amblyopia in which one eye is favored over the other due to strabismus, or eye misalignment. This condition causes reduced visual acuity in the misaligned eye because the brain suppresses the image from that eye in order to avoid the confusion of double vision. This suppression eventually causes underdevelopment of the visual processing associated with that eye, resulting in amblyopia.
Understanding Strabismus
Strabismus is a condition in which the eyes do not align properly, causing one eye to turn inward (esotropia), outward (exotropia), upward (hypertropia), or downward (hypotropia) while the other remains focused. This misalignment disrupts the normal binocular vision process, which allows the brain to combine images from both eyes into a single, coherent visual representation. In a child with strabismus, the brain frequently ignores input from the misaligned eye in order to avoid seeing double images, resulting in amblyopia in that eye.
Strabismus can be congenital, appearing in early infancy, or acquired later in childhood. The severity and type of strabismus vary, but any persistent misalignment can lead to amblyopia if not treated. The condition is especially concerning in children because the visual system is still developing, and early treatment is critical to preventing permanent vision loss in the affected eye.
Pathophysiology of Strabismic Amblyopia
Strabismic amblyopia causes complex interactions between the eyes and the brain’s visual processing centers. Normally, the visual cortex of the brain receives and integrates input from both eyes, resulting in a three-dimensional perception of the environment. However, strabismus can cause one eye to be consistently misaligned, resulting in conflicting visual information to the brain. To avoid the confusion of double vision, the brain suppresses visual input from the misaligned eye, resulting in a lack of use, or under-stimulation, of the neural pathways connected to that eye.
This suppression, if maintained over time, prevents the misaligned eye from developing normal visual acuity. The neural circuits responsible for processing input from the suppressed eye do not fully develop, resulting in amblyopia. The critical period for visual development typically occurs during the first few years of life, making early detection and intervention critical. Strabismic amblyopia, if not treated during this critical period, can cause permanent visual impairment in the affected eye.
Clinical Characteristics Of Strabismic Amblyopia
The clinical characteristics of strabismic amblyopia differ according to the severity and type of strabismus. Common signs include:
- Reduced Visual Acuity in One Eye: The most noticeable feature of strabismic amblyopia is a decrease in vision sharpness in the misaligned eye. This decrease in visual acuity is typically not correctable with glasses or contact lenses alone, as the problem is with the brain’s processing of visual information rather than the optical focus of the eye.
- Strabismus is defined as the misalignment of one eye. This misalignment can be constant or intermittent, affecting the same eye consistently or alternating between the two eyes.
- Suppression of the Affected Eye: To avoid double vision, the brain frequently suppresses images from the misaligned eye. This suppression can occur consciously or unconsciously, and its degree varies according to the severity of the strabismus.
- Lack of Depth Perception: Depth perception requires binocular vision, which involves the coordinated use of both eyes. Children with strabismic amblyopia frequently have poor depth perception, making it difficult to judge distances accurately.
- Squinting or Closing One Eye: Some children with strabismic amblyopia may squint or close one eye when attempting to focus, especially in bright light or while concentrating on an object.
- Head Tilting or Turning: To compensate for the misalignment and improve eye alignment, some children may tilt or turn their heads.
Causes and Risk Factors
Strabismic amblyopia can develop due to a variety of factors, including:
- Genetic Predisposition: A family history of strabismus or amblyopia increases a child’s risk of developing these conditions. Genetic factors can influence the development and control of eye muscles, resulting in strabismus and amblyopia.
- Uncorrected Refractive Errors: Some uncorrected refractive errors, such as farsightedness (hyperopia), can result in strabismus. When one eye has a significantly different refractive error from the other, the brain may favor the eye with better vision, resulting in amblyopia in the other eye.
- Prematurity and Low Birth Weight: Children born prematurely or underweight are more likely to develop strabismus and amblyopia. This is most likely due to an increased risk of developmental delays and complications affecting the vision.
- Neurological Conditions: Some neurological conditions, such as cerebral palsy or Down syndrome, can increase the likelihood of developing strabismus and amblyopia. These conditions frequently involve abnormalities in the development or function of the nervous system, which can impair eye alignment and coordination.
- Maternal Substance Use: Pregnancy exposure to alcohol or drugs can increase the risk of developmental issues in the child, such as strabismus and amblyopia.
Effect on Vision and Quality of Life
Strabismic amblyopia can significantly impair a child’s vision and overall quality of life. When one eye’s visual acuity deteriorates, the child may struggle to perform tasks that require fine visual discrimination, such as reading, writing, or recognizing faces. A lack of depth perception can also make activities like catching a ball, climbing stairs, and navigating uneven surfaces more difficult.
In addition to these practical issues, strabismic amblyopia can have psychological and social consequences. Children with visible strabismus may develop self-consciousness about their appearance, especially as they approach school age. They may also struggle with social interactions if their reduced visual acuity limits their ability to read social cues or participate in play activities with their peers.
Strabismic amblyopia can cause visual impairment that lasts into adulthood, potentially limiting educational and occupational opportunities. In severe cases, the condition can result in legal blindness in the affected eye, which may have additional implications for the individual’s ability to drive, work, or live independently.
Value of Early Detection and Intervention
The key to successfully managing strabismic amblyopia is early detection and intervention. Because the visual system is most malleable during early childhood, treating amblyopia during this critical period can result in significant visual improvements. Pediatricians, optometrists, and ophthalmologists all play an important role in screening young children for strabismus and amblyopia during routine check-ups.
Parents and caregivers should be aware of the signs of strabismus and amblyopia in their children and seek prompt medical attention if they notice any of these symptoms. Early intervention usually consists of a variety of treatments aimed at improving eye alignment, stimulating the affected eye, and retraining the brain to use both eyes simultaneously.
Strabismic amblyopia has a good prognosis if diagnosed and treated early. However, if treatment is delayed or incomplete, the chances of achieving normal visual acuity in the affected eye decrease, while the risk of permanent vision loss rises.
Diagnostic Approaches for Strabismic Amblyopia
A thorough eye examination by an eye care professional, such as an optometrist or ophthalmologist, is required to diagnose strabismic amblyopia. Several diagnostic methods are used to determine the presence and severity of strabismus and amblyopia, with each playing an important role in determining the best treatment plan.
Visual acuity testing
The first step in diagnosing amblyopia is to determine the visual acuity of each eye separately. Visual acuity testing involves using an eye chart to determine how well the child sees at different distances. For young children who do not yet know their letters, specially designed eye charts with shapes, pictures, or tumbling E’s (in which the child indicates the direction of the “E”) are used. A significant difference in visual acuity between the two eyes is characteristic of amblyopia.
Cover-Uncover Test
The cover-uncover test is a simple yet effective way to detect strabismus. During this test, the eye care professional will cover one of the child’s eyes while they concentrate on a specific object. Observing the uncovered eye allows the examiner to determine whether it moves to fixate on the object, indicating the presence of strabismus. The test is repeated on the opposite eye to determine the alignment of both eyes. This test helps to determine which eye is misaligned and what type of strabismus is present.
Refraction Assessment
A refraction test is used to determine whether refractive errors like myopia (nearsightedness), hyperopia (farsightedness), or astigmatism are contributing to the development of amblyopia. This test is typically performed after administering eye drops that temporarily paralyze the eye’s focusing muscles, allowing for a more accurate measurement of the refractive error. Identifying and correcting significant refractive errors is an important step in the overall treatment of strabismic amblyopia.
Binocular Vision Assessment
The binocular vision test assesses how well the eyes work together to form a single visual image. This assessment is critical in diagnosing amblyopia because it determines the level of suppression and binocular dysfunction. Binocular vision can be evaluated using tests such as the Worth 4 Dot test, the Bagolini Striated Lens test, and the synoptophore. These tests assist the eye care professional in determining whether the brain is effectively merging images from both eyes or if one eye is suppressed, as is typical of amblyopia.
Cycloplegic Refraction
Cycloplegic refraction is a specialized type of refraction assessment that uses cycloplegic eye drops to temporarily paralyze the ciliary muscle, which controls the eye’s ability to focus. This allows the eye care professional to measure the eye’s refractive error without interference from accommodation (the eye’s focusing mechanism). Cycloplegic refraction is especially useful in children because it provides a more accurate assessment of refractive errors that could be causing amblyopia or strabismus.
Ocular Alignment and Motility Tests
Ocular alignment and motility testing determine how well the eyes move and interact. The examiner will ask the child to follow a target with their eyes in different directions to check for any limitations in eye movement, the presence of nystagmus (involuntary eye movements), or eye alignment issues. These tests aid in diagnosing the type and severity of strabismus, which is essential for developing effective treatment strategies.
Stereopsis Testing
Stereopsis, or depth perception, is an essential part of binocular vision. Stereopsis testing assesses a child’s ability to perceive three-dimensional depth using both eyes simultaneously. The Randot Stereotest and the Titmus Fly Test are two common tools for assessing stereopsis. Strabismic amblyopia is characterized by reduced or absent stereopsis, indicating a loss of binocular vision as a result of misalignment and subsequent suppression of the weaker eye.
Fundus Examination
A fundus examination, also known as ophthalmoscopy, allows an eye care professional to examine the eye’s interior surface, which includes the retina, optic disc, and blood vessels. This examination is critical for ruling out other ocular conditions that may be causing the child’s symptoms, such as retinal diseases, optic nerve abnormalities, or structural issues. While amblyopia primarily affects the brain’s visual processing pathway, it is critical to rule out any underlying ocular pathology that may necessitate a different treatment strategy.
Neurological Examination
In some cases, especially if the strabismus is acquired rather than congenital, a neurological examination may be required to rule out neurological causes of eye misalignment, such as cranial nerve palsies, brain tumors, or other central nervous system disorders. This examination may include neuroimaging studies, such as MRI or CT scans, to provide a more detailed picture of the brain and orbits.
Electrophysiological Tests
Electrophysiological tests, such as visual evoked potentials (VEP) or electroretinography (ERG), may be used in some cases to assess the functional integrity of the visual pathway. VEP measures electrical activity in the brain in response to visual stimuli, which aids in the evaluation of the optic nerve and visual cortex. ERG measures the retina’s electrical responses to light, which provides information about retinal function. These tests are not commonly used to diagnose strabismic amblyopia, but they may be useful in complex cases or when the diagnosis is unclear.
Practical Management of Strabismic Amblyopia
The treatment of strabismic amblyopia focuses on both the underlying strabismus (eye misalignment) and the amblyopia (lazy eye). Early intervention is critical because the visual system is most adaptable during childhood, making it the ideal time to correct the condition and avoid long-term visual impairment. The treatment strategy typically consists of a combination of therapies aimed at improving eye alignment, stimulating the amblyopic eye, and improving binocular vision.
Corrective Lenses
One of the first steps in treating strabismic amblyopia is to prescribe corrective lenses to address any underlying refractive errors, such as myopia, hyperopia, or astigmatism. Glasses or contact lenses help to ensure that both eyes see clearly, which is critical for encouraging the use of the amblyopic eye. In some cases, correcting the refractive error alone can improve eye alignment and reduce the severity of amblyopia, especially if accommodative esotropia is present.
Occlusion Therapy (Patching
Occlusion therapy, also known as patching, is a key component of amblyopia treatment. This method entails covering the stronger (non-amblyopic) eye with an eye patch for several hours each day, forcing the brain to use the weaker eye. Patching promotes the development of visual acuity in the amblyopic eye by stimulating previously underutilized neural pathways. The severity of the amblyopia and the child’s age determine the duration and frequency of patching. Consistent and monitored use of the patch is required for best results, as irregular use may reduce the treatment’s effectiveness.
Penalization Therapy
Penalization therapy, which is an alternative to patching, involves blurring the vision of the stronger eye in order to encourage the use of the amblyotic eye. This can be accomplished by applying atropine eye drops, which dilate the pupil and blur near vision in the stronger eye, or by wearing a lens that slightly defocuses the stronger eye. Penalization therapy is frequently recommended for children who are resistant to wearing eye patches or who struggle to comply with patching. This method has proven to be effective, particularly in mild to moderate amblyopia.
Vision Therapy
Vision therapy is a series of structured visual activities and exercises that aim to improve eye coordination and function. These exercises aim to improve binocular vision, depth perception, and the ability to focus and track objects. An optometrist or ophthalmologist may supervise vision therapy, which may include activities such as eye tracking exercises, focusing exercises, and the use of specialized equipment such as prisms or computer programs. Vision therapy works best when combined with other treatments, such as patching or corrective lenses.
Surgical Intervention
When strabismus is severe or does not respond to conservative treatments, surgery may be required. Strabismus surgery involves repositioning the eye muscles to align the eyes. The goal of surgery is to improve eye alignment, which can help reduce or eliminate amblyopia suppression. While surgery can effectively align the eyes, it does not directly treat amblyopia; thus, it is frequently combined with other therapies, such as patching or vision therapy, to achieve the best visual results.
Maintenance and Follow-up
Strabismic amblyopia is not a one-time treatment; it requires ongoing monitoring and maintenance. Regular eye exams are essential for tracking progress and adjusting treatment as needed. As the child’s visual system matures, the treatment plan may need to be adjusted to ensure continued improvement and avoid regression. Even after successful treatment, some children may require ongoing therapy, such as part-time patching, to maintain the visual gains made.
In addition to medical treatments, parental and caregiver support is essential for the successful management of strabismic amblyopia. Ensuring that the child follows the prescribed treatment regimen, whether it is wearing an eye patch, using corrective lenses, or participating in vision therapy, is critical for achieving the best possible results.
Trusted Resources and Support
Books
- “Amblyopia: A Comprehensive Guide” by Dr. Stuart Dankner: This book offers an in-depth look at amblyopia, including causes, treatment options, and management strategies, making it a valuable resource for parents and healthcare professionals.
- “The Eye Patch Kids” by A.D. Largie: A children’s book designed to help young children understand and cope with wearing an eye patch. It provides comfort and encouragement to children undergoing treatment for amblyopia.
Organizations
- The American Association for Pediatric Ophthalmology and Strabismus (AAPOS): AAPOS provides extensive resources for understanding and managing pediatric eye conditions, including amblyopia. The organization also offers a directory of specialists and educational materials for parents.
- The Amblyopia Foundation of America (AFA): AFA is dedicated to raising awareness about amblyopia and providing support to families affected by the condition. The foundation offers resources, support groups, and information on the latest treatment options.