The fallopian tubes are an essential part of the female reproductive system, acting as the bridge between the ovaries and the uterus. They play a pivotal role in fertilization by capturing the ovum released during ovulation, providing a nurturing environment for sperm and facilitating the meeting of gametes. Beyond fertilization, the fallopian tubes are involved in transporting the zygote into the uterus for implantation and early embryonic development. Their complex structure—divided into the infundibulum, ampulla, isthmus, and intramural segment—supports a range of functions that are critical for fertility. This guide offers an in-depth exploration of fallopian tube anatomy, physiology, common disorders, diagnostic methods, treatment options, and lifestyle tips to maintain reproductive health.
Table of Contents
- Structural Anatomy & Composition
- Functional Dynamics & Role in Fertilization
- Vascular Supply, Innervation & Microenvironment
- Physiological Insights & Hormonal Influence
- Common Fallopian Tube Disorders
- Diagnostic Techniques & Evaluation Methods
- Therapeutic Options & Interventions
- Nutritional Strategies & Supplementation
- Lifestyle Practices for Reproductive Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
Structural Anatomy & Composition
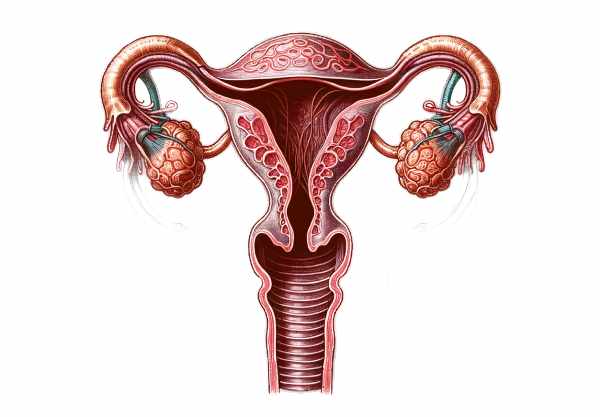
The fallopian tubes, also known as uterine tubes or oviducts, are slender, muscular tubes approximately 10 to 12 centimeters long. They extend laterally from the upper corners of the uterus to the vicinity of the ovaries. Anatomically, each tube is subdivided into four regions: the infundibulum, ampulla, isthmus, and the intramural (or interstitial) segment.
Regions of the Fallopian Tube
- Infundibulum:
The funnel-shaped distal end of the tube is adorned with delicate, finger-like projections called fimbriae. These structures sweep over the ovary during ovulation to capture the released egg and guide it into the tube. - Ampulla:
This is the widest and longest segment of the fallopian tube and serves as the primary site for fertilization. Its highly folded mucosal lining creates a spacious environment where sperm can meet the egg, and where crucial biochemical interactions take place to promote sperm capacitation. - Isthmus:
The isthmus is a narrow, muscular segment that connects the ampulla to the uterine cavity. Its thick muscular walls are essential for generating the peristaltic contractions that help transport the fertilized egg toward the uterus. - Intramural (Interstitial) Part:
This segment passes through the uterine wall and is the narrowest portion of the fallopian tube. It serves as the final passageway for the embryo to enter the uterine cavity, where implantation will occur.
Histological Layers
The fallopian tube is composed of three primary layers:
- Mucosa:
Lined by a pseudostratified columnar epithelium with ciliated and secretory (non-ciliated) cells, the mucosa is responsible for both the absorption of excess fluid and the secretion of nutrients essential for sperm and embryo survival. The cilia generate a directed current to facilitate gamete and embryo transport. - Muscularis:
Consisting of inner circular and outer longitudinal smooth muscle layers, the muscularis generates peristaltic movements. These coordinated contractions are vital for moving the egg and embryo through the tube and towards the uterus. - Serosa:
The outermost layer, a thin serous membrane derived from mesothelium, envelops the tube and anchors it within the pelvic cavity, providing both structural support and protection.
Together, these layers create an environment optimized for fertilization and early embryonic development while facilitating efficient gamete transport.
Functional Dynamics & Role in Fertilization
The fallopian tubes are indispensable to female fertility, performing several key functions that ensure the successful meeting of sperm and egg, as well as the proper transport of the fertilized embryo to the uterus.
Gamete Transportation
- Ovum Capture:
The process begins when the fimbriae of the infundibulum sweep over the ovary to capture the released ovum. The movement of cilia on the epithelial lining generates gentle currents that guide the egg into the tube. - Sperm Migration:
Sperm that enter the reproductive tract must navigate through the cervix and uterus to reach the fallopian tubes. The tubal secretions and rhythmic muscular contractions in the tube facilitate the capacitation and movement of sperm, enhancing their ability to fertilize the ovum.
Fertilization Process
- Site of Fertilization:
Fertilization most commonly occurs in the ampulla, where the environment is ideal for the sperm-egg encounter. The spacious lumen and secretions of the ampulla provide the optimal conditions for sperm capacitation and the acrosome reaction, which enables the sperm to penetrate the egg. - Biochemical Interactions:
The secretory cells of the fallopian tube release proteins, lipids, and growth factors that modify the sperm membrane and prepare the ovum for fertilization. This biochemical milieu is crucial for the successful fusion of gametes.
Embryo Transport
- Movement to the Uterus:
After fertilization, the resulting zygote undergoes cell division while being transported through the isthmus. The combined action of ciliary movement and muscular contractions ensures that the developing embryo reaches the uterus at the right time for implantation. - Hormonal Regulation:
Hormones, particularly estrogen and progesterone, influence the fallopian tube’s secretions and contractility, optimizing the environment for both gamete transport and embryo survival.
Protective and Supportive Environment
- Nutritional Support:
The fluid secreted by the epithelial cells in the fallopian tube is rich in nutrients that support the viability of sperm and the early embryo. - Immunological Protection:
The fallopian tubes maintain an immune-privileged environment that protects gametes and embryos from autoimmune reactions. This delicate balance allows for effective defense against pathogens while preserving the integrity of reproductive cells.
In summary, the fallopian tubes are critical for both gamete and embryo transport, ensuring that the process of fertilization occurs under optimal conditions. Their coordinated actions, regulated by hormonal signals and supported by specialized secretions, are fundamental to successful reproduction.
Vascular Supply, Innervation & Microenvironment
The functionality of the fallopian tubes depends on a rich vascular network, precise innervation, and a tightly regulated microenvironment. These factors work together to support the delicate processes of gamete transport, fertilization, and early embryonic development.
Blood Supply
- Arterial Input:
The fallopian tubes receive blood from both the ovarian and uterine arteries. This dual arterial supply ensures that the tubes are well-nourished and capable of meeting their high metabolic demands during the reproductive cycle. - Venous Drainage:
Venous blood from the fallopian tubes drains into the ovarian and uterine veins, which help remove metabolic waste efficiently and maintain optimal tissue health.
Innervation
- Autonomic Nerve Supply:
Autonomic nerve fibers from the pelvic plexus innervate the fallopian tubes. These fibers regulate the rhythmic contractions of the muscularis, ensuring that peristaltic waves occur in a coordinated manner. - Sensory Nerve Input:
Sensory nerves within the tube transmit information about the internal environment, aiding in the regulation of secretion and contraction. This sensory feedback helps adapt the tubal environment to the varying needs of the reproductive process.
Microenvironment Regulation
- Secretory Functions:
The epithelial cells lining the fallopian tubes secrete a fluid that is rich in nutrients, growth factors, and enzymes. This fluid not only supports sperm viability and embryo development but also creates a protective barrier against pathogens. - Hormonal Influence:
Hormones such as estrogen and progesterone modulate the secretory activity and contractility of the fallopian tubes. Estrogen typically enhances ciliary movement and fluid secretion, while progesterone modulates the muscular contractions, ensuring a balanced environment for gamete transport and fertilization. - Immunological Balance:
The fallopian tubes maintain an immunologically privileged environment, minimizing the risk of an autoimmune response against sperm and embryos. This balance is achieved through localized production of immunosuppressive factors and a selective barrier formed by the epithelial lining.
Collectively, the robust vascular supply, targeted innervation, and finely tuned microenvironment ensure that the fallopian tubes function effectively throughout the reproductive cycle, promoting fertility and protecting the delicate processes of fertilization and early embryonic development.
Physiological Insights & Hormonal Influence
The fallopian tubes are governed by a complex interplay of physiological processes and hormonal signals, ensuring that they function optimally to support reproduction. Their dynamic nature is evident in their role in gamete transport, fertilization, and embryo transit, all of which are finely regulated by hormonal influences and cellular interactions.
Hormonal Regulation
- Estrogen:
Estrogen plays a key role in preparing the fallopian tubes for ovulation. It enhances the ciliary beat frequency of the epithelial cells, increases the secretion of nourishing fluids, and promotes muscular contractility. This hormone ensures that the environment within the tube is conducive to capturing the ovum and supporting sperm function. - Progesterone:
After ovulation, progesterone levels rise, modifying the secretions within the fallopian tubes and modulating muscular contractions. Progesterone’s influence helps slow the movement of the fertilized egg, allowing for gradual development before it reaches the uterus. It also plays a protective role by reducing inflammation and supporting cellular differentiation. - Other Hormones:
Additional hormones, such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH), indirectly impact the function of the fallopian tubes by regulating ovarian activity. These hormones ensure that ovulation occurs at the optimal time, coordinating with tubal function to maximize the chances of successful fertilization.
Neural and Paracrine Factors
- Autonomic Input:
The autonomic nervous system, particularly through the pelvic plexus, controls the peristaltic contractions of the fallopian tubes. This neural input is essential for the timed and coordinated movement of gametes and embryos. - Paracrine Signaling:
Local factors such as cytokines, growth factors, and enzymes secreted by the tubal epithelium influence the microenvironment. These paracrine signals regulate processes such as fluid absorption, immune response, and cellular proliferation, ensuring the tube adapts dynamically throughout the menstrual cycle.
Integration with the Reproductive Cycle
- Cycle Synchronization:
The physiological functions of the fallopian tubes are closely aligned with the menstrual cycle. During the follicular phase, estrogen predominates, enhancing tubal motility and secretion. Following ovulation, progesterone modulates these activities, optimizing conditions for fertilization and early embryonic development. - Feedback Mechanisms:
Sensory receptors in the fallopian tubes provide feedback to the central nervous system, allowing for fine-tuning of muscular contractions and secretions. This integrated network ensures that the fallopian tubes respond appropriately to changes in the reproductive environment.
These hormonal and neural influences are critical for the proper functioning of the fallopian tubes. By coordinating the timing of gamete transport and creating a supportive environment for fertilization, these regulatory mechanisms play a vital role in ensuring reproductive success.
Common Fallopian Tube Disorders
Several conditions can disrupt the normal function of the fallopian tubes, leading to fertility issues and other reproductive complications. Early identification and treatment of these disorders are crucial for preserving fertility and preventing further complications.
Pelvic Inflammatory Disease (PID)
- Overview and Causes:
PID is an infection of the female reproductive organs, often caused by sexually transmitted bacteria such as Chlamydia trachomatis or Neisseria gonorrhoeae. The infection can ascend from the vagina and cervix to the fallopian tubes, causing inflammation and scarring. - Symptoms:
Women with PID typically experience lower abdominal pain, fever, abnormal vaginal discharge, and pain during intercourse. Chronic PID can lead to significant scarring, resulting in tubal blockage and increased risk of ectopic pregnancy. - Diagnosis and Management:
Diagnosis is made through pelvic examination, laboratory tests for infections, and imaging studies like ultrasound. Treatment involves a course of antibiotics, and in severe cases, surgical intervention may be necessary to remove scar tissue.
Ectopic Pregnancy
- Definition and Etiology:
An ectopic pregnancy occurs when a fertilized egg implants outside the uterine cavity, most commonly within the fallopian tube. This condition is often linked to previous tubal infections, PID, or structural abnormalities in the tubes. - Symptoms:
Early signs include abdominal pain, vaginal bleeding, and in some cases, shoulder pain. If the tube ruptures, it can lead to internal bleeding and become life-threatening. - Diagnosis and Treatment:
Diagnosis is confirmed by transvaginal ultrasound and measuring human chorionic gonadotropin (hCG) levels. Treatment options include methotrexate to medically terminate the ectopic pregnancy or surgical intervention to remove the ectopic tissue and repair the tube.
Tubal Blockage
- Causes:
Blockages in the fallopian tubes can occur due to scarring from infections (like PID), endometriosis, or previous pelvic surgeries. These blockages prevent sperm from reaching the egg and hinder embryo transport to the uterus. - Clinical Manifestations:
Tubal blockage is a common cause of infertility. Women may have no symptoms until they experience difficulty conceiving. - Diagnosis and Intervention:
Tubal patency is typically assessed via hysterosalpingography (HSG) or laparoscopy. Treatment options include surgical removal of blockages or the use of assisted reproductive technologies such as in vitro fertilization (IVF).
Endometriosis
- Pathophysiology:
Endometriosis is characterized by the presence of endometrial tissue outside the uterus, often on the fallopian tubes, ovaries, and pelvic peritoneum. This ectopic tissue causes inflammation, scarring, and adhesions that can distort the normal anatomy of the tubes. - Symptoms:
Common symptoms include severe pelvic pain, painful menstruation, and infertility. The condition can impair the function of the fallopian tubes by blocking them or altering their environment. - Diagnosis and Treatment:
Laparoscopy is the gold standard for diagnosing endometriosis. Treatment options include hormonal therapy, pain management, and surgical removal of endometrial lesions.
Congenital Anomalies
- Tubal Abnormalities:
Some women may be born with structural anomalies in the fallopian tubes that can impair their function. These anomalies may be detected during fertility evaluations and can contribute to infertility. - Diagnosis and Management:
Imaging studies and laparoscopy help diagnose congenital tubal anomalies. Management depends on the severity of the defect and may involve surgical correction or assisted reproductive techniques.
Understanding these conditions is essential for early detection and appropriate management. Timely intervention can improve fertility outcomes and reduce the risk of complications, making awareness of fallopian tube health a critical aspect of female reproductive wellness.
Diagnostic Approaches & Evaluation Methods
Accurate diagnosis of fallopian tube disorders is key to effective treatment and fertility management. A combination of clinical assessments, imaging studies, and specialized tests provides a comprehensive evaluation of tubal structure and function.
Clinical Examination and History
- Detailed Medical History:
A thorough history, including menstrual cycle details, previous infections, surgeries, and sexual history, helps identify risk factors for tubal disorders. A careful examination of symptoms such as pelvic pain and infertility is also critical. - Physical Examination:
A pelvic exam can reveal tenderness, masses, or abnormalities in the adnexal region, which may indicate underlying tubal pathology.
Imaging Techniques
- Hysterosalpingography (HSG):
HSG is a radiographic procedure that involves injecting a contrast dye into the uterine cavity. X-ray images then reveal the shape of the uterine cavity and the patency of the fallopian tubes. HSG is the most common test for evaluating tubal blockages or structural anomalies. - Transvaginal Ultrasound:
This non-invasive imaging technique uses a transducer inserted into the vagina to produce detailed images of the pelvic organs, including the fallopian tubes. It can detect cysts, signs of inflammation, and other structural abnormalities. - Sonohysterography:
By infusing saline into the uterine cavity during an ultrasound, sonohysterography provides enhanced visualization of the uterine cavity and tubal patency, offering additional details in cases of suspected abnormalities.
Laparoscopy
- Direct Visualization:
Laparoscopy is a minimally invasive surgical procedure that allows direct observation of the pelvic organs, including the fallopian tubes. It is particularly useful for diagnosing conditions like endometriosis, PID, and congenital anomalies. - Therapeutic Interventions:
In addition to diagnosis, laparoscopy permits simultaneous treatment, such as the removal of adhesions or scar tissue that may be blocking the tubes.
Laboratory Tests
- Semen Analysis:
In cases of infertility, semen analysis is performed to assess sperm quality and detect potential tubal obstruction if sperm are absent or present in low numbers in the ejaculate. - Infection Screening:
Testing for sexually transmitted infections (STIs) such as chlamydia and gonorrhea is critical, as these are common causes of PID and subsequent tubal damage.
Advanced Diagnostic Procedures
- Magnetic Resonance Imaging (MRI):
Although not used routinely, MRI can provide high-resolution images of the pelvic anatomy, useful in complex cases where detailed soft tissue visualization is required. - Laparoscopic Chromopertubation:
This technique involves injecting dye during laparoscopy to assess tubal patency directly. It is highly effective for evaluating subtle tubal blockages that might not be visible on HSG or ultrasound.
By combining these diagnostic methods, clinicians can accurately evaluate the fallopian tubes, determine the extent of any damage or blockages, and devise the most appropriate treatment strategy to preserve fertility and reproductive health.
Treatment Options & Interventions
Treatment for fallopian tube disorders is tailored to the specific condition, its severity, and the patient’s reproductive goals. Management may involve conservative medical therapies, surgical interventions, or assisted reproductive technologies (ART) when necessary.
Medical Management
- Antibiotic Therapy:
In cases of pelvic inflammatory disease (PID), prompt antibiotic treatment is essential. A combination of antibiotics is used to target common pathogens, reducing inflammation and preventing long-term scarring that could obstruct the tubes. - Hormonal Treatments:
Hormonal therapies, including oral contraceptives and gonadotropin-releasing hormone (GnRH) agonists, can help manage conditions such as endometriosis. By reducing the growth of ectopic endometrial tissue, these treatments alleviate inflammation and improve tubal function.
Surgical Interventions
- Laparoscopic Surgery:
Minimally invasive laparoscopic techniques are commonly employed to diagnose and treat tubal disorders. Procedures such as adhesiolysis (removal of adhesions) and tubal cannulation can restore patency and improve fertility outcomes. - Salpingostomy and Salpingectomy:
For ectopic pregnancies, a salpingostomy (removal of the ectopic tissue while preserving the tube) or a salpingectomy (removal of the affected tube) may be performed. The choice depends on the extent of damage and the patient’s future fertility plans. - Tubal Reanastomosis:
In cases of tubal blockage due to previous surgeries or scarring, microsurgical procedures such as tubal reanastomosis can reconnect the tube segments, thereby restoring its function. These delicate procedures require specialized surgical expertise.
Assisted Reproductive Technologies (ART)
- In Vitro Fertilization (IVF):
When tubal damage is severe and cannot be corrected surgically, IVF offers an alternative. Eggs are retrieved from the ovaries, fertilized in the laboratory, and then the resulting embryos are transferred directly into the uterus, bypassing the fallopian tubes altogether. - Intracytoplasmic Sperm Injection (ICSI):
Often used in conjunction with IVF, ICSI involves injecting a single sperm directly into an egg. This technique is particularly useful in cases of male factor infertility or tubal obstruction.
Emerging and Innovative Therapies
- Robotic-Assisted Surgery:
Advances in robotic surgery have increased the precision of laparoscopic procedures on the fallopian tubes, reducing recovery times and enhancing surgical outcomes. - Regenerative Medicine:
Research into stem cell therapy and tissue engineering holds promise for repairing damaged fallopian tube tissue. Although still experimental, these techniques may offer future solutions for restoring tubal function. - Fertility Preservation:
For women at risk of tubal damage from medical treatments (e.g., chemotherapy), options such as egg or embryo freezing can preserve reproductive potential for future use.
By employing a multidisciplinary treatment approach, healthcare providers can address various fallopian tube disorders effectively. Tailored interventions, whether surgical or through assisted reproduction, improve fertility outcomes and help maintain overall reproductive health.
Nutritional Strategies & Supplementation
Optimal fallopian tube health is influenced by proper nutrition and targeted supplementation. A balanced diet rich in essential nutrients supports reproductive health by reducing inflammation, promoting cellular repair, and ensuring a conducive environment for gamete transport and embryo development.
Key Nutrients for Reproductive Health
- Vitamin D:
Adequate vitamin D levels support hormonal balance and immune function, which are crucial for maintaining the integrity of fallopian tube tissues. - Vitamin E:
Known for its antioxidant properties, vitamin E helps protect cells from oxidative stress, potentially reducing inflammation and supporting tubal health. - Folic Acid:
Folic acid is critical for cell division and DNA synthesis, which are essential for healthy reproductive tissue. It is particularly important during preconception and early pregnancy. - Zinc:
Zinc is vital for reproductive function, influencing sperm quality and hormone metabolism. It also plays a role in tissue repair and immune response.
Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish oil, flaxseed, and walnuts, offer potent anti-inflammatory benefits. They help maintain the integrity of cell membranes and support hormonal balance, both of which are important for optimal fallopian tube function.
Herbal Supplements
- Vitex (Chaste Tree Berry):
Vitex is renowned for its hormone-regulating properties. It may help balance reproductive hormones, regulate menstrual cycles, and support fallopian tube health. - Evening Primrose Oil:
Rich in gamma-linolenic acid (GLA), evening primrose oil may improve the quality of cervical mucus and reduce inflammation, promoting a healthy reproductive environment.
Antioxidant Support
- Coenzyme Q10 (CoQ10):
CoQ10 supports cellular energy production and acts as an antioxidant, protecting reproductive tissues from oxidative damage. - N-Acetylcysteine (NAC):
NAC replenishes glutathione levels, a critical antioxidant that helps mitigate oxidative stress and supports overall reproductive health.
Integrating these nutritional strategies and supplements into your daily regimen can help foster an optimal environment for fallopian tube function and overall fertility.
Lifestyle Practices for Reproductive Wellness
Maintaining healthy fallopian tubes and overall reproductive function requires more than just medical treatment and proper nutrition—it also demands a proactive approach through lifestyle choices. The following practices can help reduce the risk of tubal damage, improve fertility, and promote overall reproductive well-being.
Diet and Hydration
- Balanced Diet:
Eating a diet rich in fruits, vegetables, lean proteins, and whole grains ensures a steady supply of antioxidants, vitamins, and minerals that support reproductive health. - Stay Hydrated:
Adequate hydration supports the production of healthy cervical mucus and maintains optimal tissue function, including that of the fallopian tubes.
Physical Activity
- Regular Exercise:
Engaging in regular, moderate exercise improves blood circulation, which is vital for delivering nutrients and removing toxins from the reproductive organs. Activities such as walking, swimming, and yoga are beneficial. - Stress-Relieving Activities:
Exercise not only enhances physical health but also helps reduce stress, which can adversely affect hormonal balance and reproductive function.
Avoid Harmful Substances
- Quit Smoking:
Smoking has been linked to decreased fertility and tubal damage due to its negative impact on blood flow and increased oxidative stress. Quitting smoking is one of the best decisions for reproductive health. - Limit Alcohol Consumption:
Excessive alcohol intake can disrupt hormonal balance and impair reproductive function. Moderation is key to preserving fertility.
Sexual Health and Safe Practices
- Practice Safe Sex:
Use barrier methods during sexual activity to protect against sexually transmitted infections (STIs), which are a major cause of pelvic inflammatory disease (PID) and subsequent tubal damage. - Regular Gynecological Check-Ups:
Routine visits to a healthcare provider can help detect and treat infections early, preventing complications that may affect the fallopian tubes.
Stress Management and Mental Health
- Reduce Stress:
Chronic stress can negatively impact reproductive hormones and fertility. Incorporating stress management techniques such as meditation, deep-breathing exercises, or yoga can be highly beneficial. - Adequate Sleep:
Good quality sleep is essential for the body’s repair and regeneration processes, including those in the reproductive system. Aim for 7–9 hours of sleep per night.
By adopting these lifestyle practices, you can create a supportive environment for the fallopian tubes and overall reproductive health, thereby increasing the chances of successful conception and a healthy pregnancy.
Trusted Resources & Further Reading
Staying informed about reproductive health and the function of the fallopian tubes is essential for both patients and healthcare providers. Below are some trusted resources that offer detailed information, current research, and practical guidance on maintaining optimal fertility.
Recommended Books
- “Taking Charge of Your Fertility” by Toni Weschler:
A comprehensive guide to understanding reproductive health and fertility, offering practical advice on enhancing natural fertility through lifestyle and dietary changes. - “The Infertility Cure” by Randine Lewis:
Explores holistic approaches to treating infertility, including natural remedies and lifestyle modifications that support fallopian tube health. - “It Starts with the Egg” by Rebecca Fett:
Focuses on optimizing egg quality and overall reproductive health, with relevant insights into improving tubal function and fertility outcomes.
Academic Journals
- Fertility and Sterility:
A leading journal in reproductive medicine that publishes research on infertility, reproductive biology, and treatment innovations, including studies on fallopian tube function. - Human Reproduction:
This peer-reviewed journal covers a broad spectrum of reproductive health topics, offering in-depth research on the anatomy, physiology, and pathology of the female reproductive system.
Digital Tools and Mobile Apps
- Clue:
A menstrual cycle tracking app that helps monitor fertility, ovulation, and reproductive health, offering insights into potential issues with the fallopian tubes. - Ovia Fertility:
Provides personalized fertility tracking and insights based on menstrual cycles, offering tools that can assist in identifying and managing reproductive health concerns. - Glow:
An app that tracks menstrual cycles, fertility, and overall reproductive health, with a supportive community and tailored insights to help manage fertility challenges.
These resources provide valuable insights and practical tools to help you understand, monitor, and enhance fallopian tube health and overall fertility.
Frequently Asked Questions About Fallopian Tubes
What are fallopian tubes and what is their primary function?
Fallopian tubes are narrow, muscular ducts that connect the ovaries to the uterus. Their main function is to capture the ovum during ovulation, provide an environment for fertilization, and transport the fertilized egg (zygote) to the uterus for implantation.
How do fallopian tubes support fertility?
The fallopian tubes facilitate sperm and egg interaction through their ciliated epithelium and secretory cells. Their peristaltic contractions help transport the ovum and embryo, while the secretions provide nourishment and protection, thereby promoting successful fertilization and implantation.
What are common conditions affecting the fallopian tubes?
Common conditions include pelvic inflammatory disease (PID), ectopic pregnancy, tubal blockages, endometriosis affecting the tubes, and congenital anomalies. These disorders can lead to infertility, chronic pain, and other reproductive complications.
How are fallopian tube disorders diagnosed?
Diagnosis typically involves imaging techniques such as hysterosalpingography (HSG), transvaginal ultrasound, and laparoscopy, along with a thorough clinical examination and relevant laboratory tests to assess tubal patency and detect inflammation or scarring.
What lifestyle changes can improve fallopian tube health?
Maintaining a healthy diet, staying hydrated, practicing safe sex, avoiding smoking and excessive alcohol, managing stress, and regular gynecological check-ups are key lifestyle practices that support the health of the fallopian tubes and overall fertility.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about fallopian tube health and female reproductive wellness.
Processes, Conditions, and Preventative Strategies