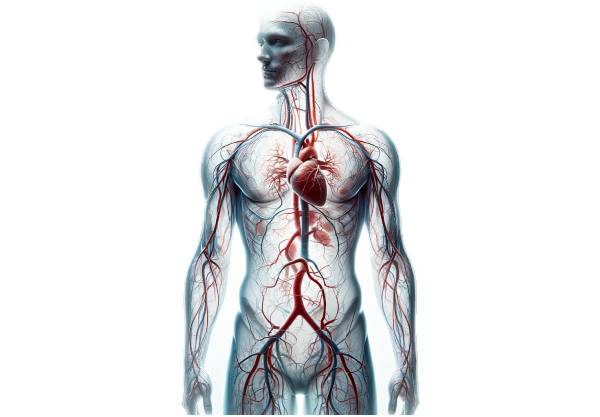
Veins are an essential component of the circulatory system, responsible for returning deoxygenated blood from the body’s tissues back to the heart. Their unique structure, characterized by thin walls, large lumens, and one-way valves, enables them to efficiently handle low-pressure blood flow and serve as reservoirs for blood. This guide delves deep into vein anatomy, explores their physiological functions and roles in thermoregulation, nutrient transport, and immune response, and discusses common venous disorders. We also cover the latest diagnostic techniques, state‐of‐the‐art treatment options, and practical lifestyle and nutritional tips to help you maintain optimal vein health.
Table of Contents
- Anatomical Structure
- Physiological Functions
- Common Vein Diseases
- Diagnostic Methods
- Treatment Options
- Supplemental & Nutritional Support
- Lifestyle & Preventive Practices
- Trusted Resources
- Frequently Asked Questions
Anatomical Structure
Veins possess a distinctive structure optimized for their role in low-pressure blood return and blood storage. Their wall is composed of three layers, each contributing to flexibility, durability, and function.
Wall Composition
- Tunica Intima
The innermost layer is formed by a single layer of endothelial cells. These cells create a smooth, frictionless lining that minimizes turbulence as blood flows through the vein. Additionally, the tunica intima forms the basis of the venous valves, which are critical for preventing backflow. - Tunica Media
The middle layer consists of smooth muscle cells and elastic fibers. Although thinner than in arteries, the tunica media in veins provides enough contractility to help maintain venous tone. Its reduced thickness allows veins to be more compliant and accommodate large volumes of blood. - Tunica Externa (Adventitia)
The outer layer is made up of connective tissue that provides structural support and protection. It anchors the veins to surrounding tissues, helping them maintain their position despite the changes in blood volume.
Valves and Function
Veins, especially those in the limbs, contain one-way valves formed by folds of the tunica intima. These valves are crucial for:
- Preventing the backward flow of blood, particularly against gravity.
- Facilitating the return of blood to the heart through the muscle pump mechanism—when surrounding muscles contract during physical activity, they compress the veins, forcing blood forward.
Types and Classification of Veins
Veins are classified based on their location and function:
- Superficial Veins:
Located close to the skin, these veins are visible and primarily drain blood from the skin and subcutaneous tissues. Examples include the cephalic and basilic veins in the upper extremities and the great and small saphenous veins in the lower extremities. - Deep Veins:
Found deeper within the body, these veins run alongside arteries and drain muscles and internal organs. Examples include the femoral, iliac, and brachial veins. - Perforating Veins:
These veins connect superficial veins to deep veins, ensuring efficient blood transfer between the two systems.
Major Veins in the Human Body
- Upper Extremities:
The cephalic and basilic veins drain the arms and merge into the axillary vein, which then becomes the subclavian vein. - Lower Extremities:
The great saphenous vein runs medially from the foot to the groin, while the small saphenous vein runs along the back of the leg, draining into the popliteal vein. - Abdomen and Thorax:
The superior vena cava (SVC) and inferior vena cava (IVC) are the two largest veins, responsible for returning blood from the upper and lower body, respectively. The hepatic veins drain the liver, and the portal vein carries nutrient-rich blood from the gastrointestinal tract to the liver. - Head and Neck:
The internal and external jugular veins drain blood from the head and neck, while the vertebral veins assist in draining the cervical spine.
Microscopic Anatomy
At the microscopic level, vein walls are characterized by:
- Endothelial Cells:
These cells not only provide a smooth surface for blood flow but also release substances such as nitric oxide that regulate vascular tone. - Smooth Muscle Cells:
Present in the tunica media, these cells facilitate venous constriction and dilation. - Connective Tissue:
Collagen and elastic fibers in the tunica externa impart structural strength and elasticity.
Venous Plexuses and Sinuses
- Venous Plexuses:
Complex networks of veins, such as the pelvic venous plexus and vertebral venous plexus, provide collateral circulation and help distribute blood evenly, especially in cases of venous obstruction. - Venous Sinuses:
Specialized channels, like the superior sagittal sinus in the brain, are crucial for draining blood from the central nervous system.
Clinical Relevance
A deep understanding of vein anatomy is essential for diagnosing and treating a range of venous disorders including varicose veins, deep vein thrombosis (DVT), and chronic venous insufficiency (CVI). This knowledge also informs surgical procedures, intravenous therapy, and the management of cardiovascular diseases.
Physiological Functions
Veins perform several critical functions that are essential to maintaining overall circulatory and cardiovascular health. Their unique design supports efficient blood return, storage, and even thermoregulation.
Blood Return to the Heart
Veins operate within a low-pressure system that facilitates the return of blood to the heart:
- Low-Pressure, High-Capacity Vessels:
Due to their larger lumens and thinner walls compared to arteries, veins can transport large volumes of blood with minimal resistance. - Valvular Function:
The presence of one-way valves prevents blood from flowing backward, ensuring unidirectional flow toward the heart. - Muscle Pump Mechanism:
Contraction of surrounding skeletal muscles, especially in the legs, compresses the veins and propels blood upward, overcoming gravity. - Respiratory Pump:
Changes in thoracic pressure during breathing further facilitate venous return.
Blood Reservoir and Volume Regulation
Veins serve as reservoirs for blood, helping to regulate overall blood volume and pressure:
- Venous Reserve:
Approximately 60–70% of the body’s blood volume is stored in the venous system. This reserve can be mobilized during times of increased demand, such as during exercise or hemorrhage. - Capacity for Expansion:
The elastic properties of veins allow them to expand in response to increased blood volume without a significant rise in pressure.
Nutrient and Waste Transport
Veins are integral to the transport of nutrients, hormones, and waste products:
- Waste Removal:
Veins collect deoxygenated blood along with metabolic waste and carbon dioxide from tissues, transporting them to the heart and lungs for exhalation. - Nutrient Distribution:
Veins also play a role in distributing absorbed nutrients from the gastrointestinal tract via the portal system, ensuring tissues receive essential compounds.
Thermoregulation
Veins near the surface of the skin help regulate body temperature:
- Heat Exchange:
When body temperature rises, increased blood flow through superficial veins facilitates heat loss. Conversely, reduced flow helps conserve heat. - Arteriovenous Anastomoses:
Specialized connections between arteries and veins allow for rapid changes in blood flow to the skin, enhancing temperature control.
Immune Function and Hormonal Regulation
- Immune Surveillance:
Veins transport white blood cells to various parts of the body, aiding in the detection and elimination of pathogens. - Endothelial Regulation:
Endothelial cells lining veins secrete substances like nitric oxide, which help regulate vascular tone and blood flow. - Hormone Transport:
Veins distribute hormones from endocrine glands to target organs, playing a key role in maintaining homeostasis.
Common Vein Diseases
Veins are prone to several disorders that can significantly impact health and quality of life. Early detection and management of these conditions are crucial for preventing complications and improving outcomes.
Varicose Veins
Varicose veins are swollen, twisted veins that commonly appear in the legs.
- Causes:
Weakened venous valves, genetic predisposition, aging, pregnancy, obesity, and prolonged standing contribute to their development. - Symptoms:
Visible bulging veins, aching, cramping, and a feeling of heaviness in the legs, along with swelling and skin discoloration. - Treatment:
Compression stockings, lifestyle changes, sclerotherapy, laser treatments, radiofrequency ablation, and surgical vein stripping are common treatment options.
Deep Vein Thrombosis (DVT)
DVT involves the formation of a blood clot in a deep vein, typically in the legs.
- Risk Factors:
Prolonged immobility, recent surgery, cancer, hormonal therapy, and genetic clotting disorders. - Symptoms:
Swelling, pain, tenderness, warmth, and redness in the affected limb; however, some cases are asymptomatic. - Treatment:
Anticoagulants, thrombolytic therapy, compression stockings, and in severe cases, surgical thrombectomy or vena cava filter placement to prevent pulmonary embolism.
Chronic Venous Insufficiency (CVI)
CVI occurs when veins cannot efficiently return blood to the heart, leading to pooling and increased pressure in the lower extremities.
- Causes:
Varicose veins, DVT, obesity, and prolonged periods of sitting or standing. - Symptoms:
Leg swelling, fatigue, pain, skin changes (thickening, discoloration), and the development of venous ulcers. - Treatment:
Compression therapy, lifestyle changes, medications to improve venous tone, sclerotherapy, endovenous laser treatment, and surgical interventions.
Phlebitis and Thrombophlebitis
Phlebitis is the inflammation of a vein, which may progress to thrombophlebitis if a clot forms.
- Causes:
Vein injury, infection, prolonged IV catheter use, and varicose veins. - Symptoms:
Pain, redness, tenderness, and swelling along the affected vein. - Treatment:
NSAIDs, warm compresses, elevation, and, if a clot is present, anticoagulant medications.
Spider Veins (Telangiectasia)
Spider veins are small, dilated blood vessels visible on the skin surface, often appearing as red, blue, or purple lines.
- Causes:
Genetics, hormonal changes, sun exposure, and prolonged standing. - Symptoms:
Generally asymptomatic but may cause cosmetic concerns and occasional discomfort. - Treatment:
Sclerotherapy, laser therapy, and lifestyle modifications to improve circulation.
Venous Ulcers
Venous ulcers are chronic wounds, usually located on the lower legs, that develop as a consequence of long-standing venous insufficiency.
- Causes:
Chronic venous insufficiency, varicose veins, and previous DVT can lead to venous stasis and subsequent ulcer formation. - Symptoms:
Painful, non-healing ulcers with irregular borders, often accompanied by skin changes and swelling. - Treatment:
Compression therapy, wound care (debridement and dressings), and treatment of the underlying venous disorder.
Pelvic Congestion Syndrome (PCS)
PCS is characterized by chronic pelvic pain resulting from varicose veins in the pelvis.
- Causes:
Hormonal changes, multiple pregnancies, and retrograde blood flow in the pelvic veins. - Symptoms:
Persistent dull pelvic pain that worsens with prolonged standing, after intercourse, or just before menstruation. - Treatment:
Hormonal therapy, pain management, and minimally invasive procedures such as embolization to block affected veins.
Superior Vena Cava Syndrome (SVCS)
SVCS occurs when the superior vena cava is obstructed, impairing blood flow from the upper body to the heart.
- Causes:
Tumors (commonly lung cancer or lymphoma), thrombosis, and infections. - Symptoms:
Swelling of the face, neck, and upper limbs; shortness of breath; coughing; and chest pain. - Treatment:
Addressing the underlying cause (e.g., cancer treatment), anticoagulation, stent placement, and supportive care.
Diagnostic Methods
A combination of clinical evaluations, imaging studies, and specialized tests is used to accurately diagnose venous disorders.
Clinical Examination
- Medical History:
Gathering detailed information on symptoms such as leg pain, swelling, skin discoloration, and a history of varicose veins or thrombosis. - Physical Examination:
Inspection and palpation of the affected areas to detect varicosities, tenderness, and signs of venous stasis.
Ultrasound Imaging
- Duplex Ultrasound:
This non-invasive test combines traditional ultrasound with Doppler technology to visualize vein structure and assess blood flow. It is the gold standard for diagnosing DVT and evaluating venous reflux in CVI.
Venography
- Procedure:
A contrast dye is injected into a peripheral vein, and X-ray images are taken to outline the vein’s course. Venography is especially useful in complex cases where ultrasound findings are inconclusive.
Magnetic Resonance Venography (MRV)
- Technique:
MRV uses magnetic resonance imaging to provide detailed images of the venous system without radiation exposure. It is particularly useful for evaluating pelvic and abdominal veins.
Computer Tomography Venography (CTV)
- Application:
CTV combines CT scanning with contrast dye to produce cross-sectional images of the venous system, useful for detecting deep vein thrombosis, SVCS, and venous malformations.
Photoplethysmography (PPG)
- Method:
PPG uses light sensors placed on the skin to measure changes in blood volume, providing data on venous function and detecting insufficiency.
Air Plethysmography (APG)
- Principle:
APG measures changes in limb volume via an inflatable cuff, which helps assess venous reflux and the efficacy of treatments like compression therapy.
Laboratory Tests
- D-dimer Test:
Elevated levels of D-dimer indicate active clot formation and breakdown, useful for diagnosing DVT when combined with clinical evaluation. - Blood Clotting Profiles:
Tests that assess coagulation parameters help in evaluating the risk of thrombosis.
Endovenous Pressure Measurement
- Invasive Testing:
Direct measurement of venous pressure via a catheter inserted into the vein provides precise information on venous hypertension, crucial for chronic venous insufficiency evaluation.
These diagnostic methods, used in combination, allow healthcare professionals to develop a comprehensive understanding of a patient’s venous health and determine the most appropriate treatment strategies.
Treatment Options
Treatment for vein disorders is tailored to the specific condition, its severity, and the overall health of the patient. Options range from conservative lifestyle modifications to advanced minimally invasive procedures and surgical interventions.
Lifestyle Modifications
- Exercise and Movement:
Regular physical activity, such as walking, swimming, or cycling, improves muscle pump function in the legs and reduces the risk of venous stasis. - Weight Management:
Maintaining a healthy weight reduces pressure on the veins, especially in the lower extremities. - Leg Elevation:
Elevating the legs above heart level several times a day can help reduce swelling and improve venous return. - Avoid Prolonged Sitting/Standing:
Frequent breaks to move around help prevent blood pooling in the legs.
Medical Management
- Compression Therapy:
Compression stockings provide graduated pressure that supports the veins, improves blood flow, and reduces swelling. - Medications:
- Anticoagulants (e.g., heparin, warfarin, DOACs) prevent the formation or extension of blood clots.
- Anti-inflammatory Drugs (NSAIDs) alleviate pain and inflammation associated with phlebitis.
- Venoactive Agents such as diosmin and hesperidin enhance venous tone and reduce symptoms of CVI.
Minimally Invasive Procedures
- Sclerotherapy:
Injection of a sclerosing solution into the affected vein causes it to collapse and eventually be reabsorbed. This is effective for treating spider veins and small varicose veins. - Endovenous Laser Therapy (EVLT):
A laser fiber is inserted into the vein, and laser energy is applied to close the vein, typically used for larger varicose veins. - Radiofrequency Ablation (RFA):
Radiofrequency energy is delivered via a catheter to heat and close problematic veins, offering similar benefits to EVLT. - Foam Sclerotherapy:
A foam sclerosant is injected into larger veins, providing more effective contact with the vein wall and improved closure.
Surgical Interventions
- Vein Stripping and Ligation:
In severe cases of varicose veins, the affected vein (commonly the great saphenous vein) is surgically removed. - Phlebectomy:
Small incisions are made to remove varicose veins near the skin’s surface, often performed under local anesthesia. - Venous Bypass Surgery:
A bypass is created using a healthy vein to reroute blood flow around a blocked or severely damaged vein. - Thrombectomy:
Surgical removal of a blood clot is sometimes necessary in cases of extensive DVT.
Advanced and Innovative Treatments
- VenaSeal Closure System:
A medical adhesive is used to seal off varicose veins. This procedure is minimally invasive and typically does not require tumescent anesthesia. - Mechanochemical Ablation (MOCA):
A dual-action approach that mechanically disrupts the vein wall while simultaneously injecting a sclerosant, resulting in effective vein closure. - Stem Cell Therapy:
Emerging research is exploring the use of stem cells to regenerate damaged venous tissue. Although experimental, this approach may offer future treatment options for chronic venous insufficiency. - Robotic-Assisted Surgery:
Robotic systems enhance surgical precision and are used for complex venous procedures, reducing recovery time and improving outcomes.
These varied treatment options ensure that therapy is personalized, addressing both symptoms and underlying causes, and improving overall vascular health.
Supplemental & Nutritional Support
In addition to conventional therapies, certain nutritional supplements can support vein health by improving circulation, reducing inflammation, and strengthening vein walls.
Recommended Supplements
- Diosmin and Hesperidin:
Often used in combination, these bioflavonoids improve vein tone, reduce capillary permeability, and alleviate symptoms of chronic venous insufficiency. - Horse Chestnut Extract:
Contains aescin, which has anti-inflammatory and vasoprotective properties, effectively reducing leg swelling and discomfort associated with varicose veins. - Grape Seed Extract:
Rich in antioxidants, grape seed extract strengthens blood vessels, improves circulation, and lowers inflammation. - Butcher’s Broom:
Known for its ability to increase venous tone and reduce swelling, this herb is useful in managing varicose veins and CVI. - Gotu Kola:
This herb promotes collagen production, strengthens connective tissue, and improves microcirculation, which benefits overall vein health. - Vitamin C and Vitamin E:
Both are potent antioxidants that support collagen synthesis and protect vein walls from oxidative damage. - Omega-3 Fatty Acids:
Found in fish oil, omega-3s have anti-inflammatory properties that improve blood flow and reduce the risk of blood clots. - Bioflavonoids:
These compounds enhance vascular strength and flexibility while reducing inflammation. - Zinc:
Zinc supports overall vascular health by aiding in tissue repair and reducing oxidative stress.
Integrating Supplements
Before starting any supplement regimen, consult a healthcare provider. When combined with a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, these supplements can significantly bolster vein health and improve overall circulatory function.
Lifestyle & Preventive Practices
Adopting healthy lifestyle practices can go a long way in maintaining optimal vein health and preventing venous disorders.
Daily Health Practices
- Maintain a Healthy Weight:
Excess weight puts additional pressure on your veins, particularly in the legs. Achieving and maintaining a healthy weight can reduce this stress. - Regular Physical Activity:
Exercises such as walking, cycling, and swimming boost circulation and strengthen the muscles that help pump blood through the veins. - Leg Elevation:
Elevating your legs above heart level several times a day reduces swelling and aids venous return. - Wear Compression Stockings:
Compression stockings are especially beneficial for individuals with varicose veins or CVI, as they enhance blood flow and reduce swelling. - Stay Hydrated:
Drinking plenty of water maintains proper blood volume and circulation. - Avoid Prolonged Immobility:
Whether sitting or standing for long periods, taking frequent breaks to move and stretch can prevent blood from pooling in your legs. - Avoid Tight Clothing:
Loose, comfortable clothing reduces pressure on the legs and abdomen, minimizing the risk of venous compression. - Quit Smoking and Limit Alcohol:
Smoking damages blood vessels and reduces circulation, while excessive alcohol intake can lead to dehydration and impaired vascular function. - Manage Stress:
Techniques such as meditation, yoga, and deep breathing help lower blood pressure and improve overall vascular health. - Dietary Considerations:
Eating a balanced diet rich in antioxidants, fiber, and healthy fats supports vascular health. Foods such as berries, citrus fruits, leafy greens, and fatty fish are particularly beneficial.
These practices, when incorporated into daily life, contribute significantly to long-term vein health and overall well-being.
Trusted Resources
Reliable information is essential for managing venous disorders effectively. Below are some authoritative resources that offer in-depth knowledge and guidance on vein health.
Books
- “The Vein Book” by John J. Bergan and Nisha Bunke-Paquette:
An exhaustive resource covering the anatomy, physiology, diagnosis, and treatment of venous disorders, ideal for both patients and healthcare professionals. - “Venous Disease Simplified” by Alun H. Davies and Ian Loftus:
A practical guide that demystifies venous diseases, offering insights into diagnosis, management, and treatment strategies. - “Chronic Venous Insufficiency: Diagnosis and Treatment” by Mark G. Whiteley:
This book provides an in-depth examination of chronic venous insufficiency, exploring the underlying mechanisms and modern treatment approaches.
Academic Journals
- Journal of Vascular Surgery: Venous and Lymphatic Disorders:
A leading publication featuring research, reviews, and clinical studies on venous and lymphatic disorders. - Phlebology:
A peer-reviewed journal that focuses on the latest advancements in the diagnosis and treatment of venous diseases.
Mobile Apps and Online Tools
- VeinSeek:
An augmented reality app that helps healthcare providers locate veins for intravenous access, enhancing procedural accuracy. - MyVeinHealth:
Provides comprehensive information on vein health, risk factors, and treatment options, along with symptom tracking and appointment management. - VeinApp:
A resource-rich app that offers educational content on venous disorders, guidance on compression therapy, and tools to locate vein specialists.
Frequently Asked Questions
What is the primary function of veins?
Veins return deoxygenated blood from the body’s tissues back to the heart. They serve as blood reservoirs, assist in thermoregulation, and facilitate the transport of nutrients, waste products, and hormones throughout the body.
How do vein valves work?
Vein valves, formed by folds in the tunica intima, prevent the backward flow of blood. They ensure that muscle contractions and respiratory movements propel blood efficiently toward the heart.
What causes varicose veins?
Varicose veins result from weakened or damaged valves, which allow blood to pool in the veins. Risk factors include genetics, aging, pregnancy, obesity, and prolonged periods of standing.
How is deep vein thrombosis (DVT) diagnosed?
DVT is typically diagnosed using duplex ultrasound, which visualizes blood clots and assesses blood flow. Other tests, like the D-dimer blood test and imaging studies, may be used to confirm the diagnosis.
What treatments are available for chronic venous insufficiency?
Chronic venous insufficiency can be managed with compression therapy, lifestyle modifications, medications, minimally invasive procedures (such as EVLT and RFA), and surgical interventions if necessary.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
Please share this article on Facebook, X (formerly Twitter), or your preferred platform to help promote awareness about vein health and encourage proactive cardiovascular care.




