Uveal effusion syndrome is a rare and potentially blinding ocular condition characterized by the abnormal accumulation of fluid in the uveal tract, which includes the iris, ciliary body, and choroid. This fluid buildup can cause retinal detachment, resulting in blurred vision, visual field loss, or, in severe cases, complete vision loss. The condition is usually idiopathic, but it can be associated with other systemic diseases or anatomical abnormalities affecting the sclera, the white outer layer of the eyeball.
The pathophysiology of uveal effusion syndrome involves an imbalance in intraocular fluid production versus drainage. When the normal drainage pathways become obstructed or dysfunctional, fluid accumulates in the uveal tissues, causing swelling and retinal detachment. Thickened sclera, abnormalities in the vortex veins (which are responsible for the eye’s venous drainage), and systemic diseases such as nanophthalmos (an abnormally small eye) are all possible causes of this condition.
A comprehensive eye examination is required to diagnose uveal effusion syndrome, which includes fundoscopy to assess the retina and choroid, as well as imaging studies such as ultrasound, optical coherence tomography (OCT), and fluorescein angiography. These diagnostic tools aid in visualizing the extent of fluid accumulation and retinal detachment, guiding treatment decisions. Early detection and appropriate management are critical for avoiding permanent vision loss and improving patient outcomes.
Uveal Effusion Syndrome Management and Treatment
The goal of managing and treating uveal effusion syndrome is to remove the fluid accumulation, reattach the retina, and restore normal vision. Conservative approaches, surgical interventions, and medical therapies tailored to the condition’s underlying cause and severity are all standard treatment options.
Conservative Management
In mild cases or early stages of uveal effusion syndrome, conservative treatment may be sufficient to alleviate symptoms and prevent progression:
- Observation and Monitoring: Schedule regular follow-up appointments to monitor the condition and assess changes in retinal detachment and fluid accumulation. This approach is appropriate for patients with minor symptoms and no immediate threat to vision.
- Positioning: Patients may be advised to maintain specific head positions to allow for natural fluid drainage and to relieve pressure on the affected areas of the eye.
Medical Management
Medical management entails using pharmacological agents to reduce intraocular inflammation and promote fluid reabsorption:
- Corticosteroids: Corticosteroids, either topical or systemic, can be used to reduce inflammation and regulate the immune system. These medications help to reduce fluid production while also promoting retinal reattachment.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs can be used as an additional treatment to reduce inflammation and relieve symptoms.
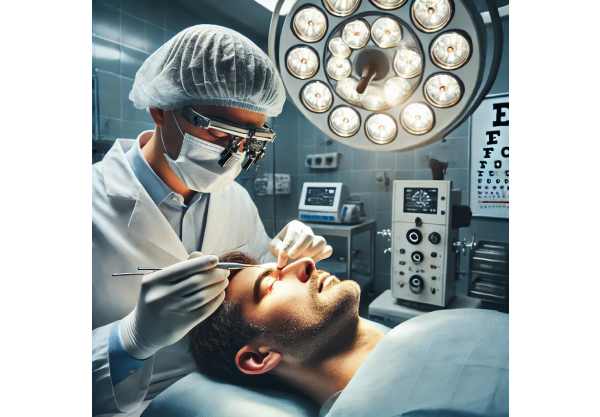
Surgical Interventions
Surgical intervention is frequently required for moderate to severe cases of uveal effusion syndrome, or when conservative and medical management fail to provide adequate relief. There are several surgical options available, each tailored to the patient’s specific needs.
- Sclerectomy: This procedure involves removing a portion of the sclera to open up a new drainage pathway for the accumulated fluid. Sclerectomy techniques include partial-thickness sclerectomy and full-thickness sclerectomy.
- Sclerostomy: A sclerostomy is the process of creating small openings in the sclera to allow fluid to drain. This procedure is less invasive than sclerectomy and can be done with specialized instruments or lasers.
- Vortex Vein Decompression: This surgical procedure focuses on the vortex veins, which are responsible for draining venous blood from the eye. Decompressing these veins can increase fluid outflow and lower intraocular pressure.
- Vitrectomy: In cases where vitreous traction causes retinal detachment, a vitrectomy may be performed to remove the vitreous gel and relieve the traction. This procedure can be combined with other surgical techniques to improve results.
Innovative Approaches to Treating Uveal Effusion Syndrome
Recent advances in the treatment of uveal effusion syndrome have introduced novel approaches that improve the effectiveness, safety, and convenience of managing this condition. These cutting-edge innovations include novel surgical techniques, advanced pharmacological agents, and emerging diagnostic and treatment technologies.
Minimal Invasive Scleral Surgery
Minimally invasive scleral surgery (MISS) is a significant advance in the surgical treatment of uveal effusion syndrome. This technique uses microincision instruments and advanced imaging guidance to perform precise scleral modifications while causing minimal trauma to surrounding tissues. Key advantages of MISS include:
- Reduced Surgical Trauma: Smaller incisions and refined surgical techniques reduce tissue damage, resulting in faster postoperative recovery and less inflammation.
- Enhanced Safety: The use of high-resolution imaging and microinstruments improves precision and control during surgery, lowering the risk of complications.
- Improved Outcomes: When compared to traditional scleral surgery, patients who undergo MISS typically experience faster visual recovery and better overall outcomes.
Laser-Assisted Scleral Procedures
Laser technology has transformed many aspects of ophthalmic surgery, including the management of uveal effusion syndrome. Laser-assisted scleral procedures, such as laser sclerostomy and laser sclerectomy, have several advantages over traditional surgical methods.
- Precision and Control: Lasers are extremely precise, allowing for targeted modifications to the sclera with minimal collateral damage.
- Minimized Bleeding: Lasers reduce intraoperative bleeding, improving the procedure’s safety and effectiveness.
- Quick Recovery: Because laser-assisted procedures are minimally invasive, patients typically recover more quickly.
Anti-VEGF Therapy
Anti-vascular endothelial growth factor (anti-VEGF) therapy, which is widely used in the treatment of retinal diseases, is being investigated for its potential use in uveal effusion syndrome. Anti-VEGF agents, such as bevacizumab and ranibizumab, prevent the formation of abnormal blood vessels and decrease vascular permeability, reducing fluid accumulation in the uveal tissues. Early research indicates that intravitreal injections of anti-VEGF agents can effectively reduce uveal effusion and improve retinal reattachment.
Immunomodulatory Agents
Immunomodulatory agents, which regulate the immune response, are being studied for their potential to treat uveal effusion syndrome. These agents target specific inflammatory pathways, allowing for a more targeted approach to reducing inflammation and increasing fluid reabsorption. Examples include:
- Interleukin Inhibitors: Agents that inhibit interleukins, such as IL-6 and IL-17, are being investigated for their ability to reduce intraocular inflammation and fluid accumulation.
- TNF-Alpha Inhibitors: Infliximab, a TNF-α inhibitor, has shown promise in reducing inflammation and improving outcomes in patients with uveal effusion syndrome.
High-Resolution Imaging
Imaging advancements have significantly improved the diagnosis and treatment of uveal effusion syndrome. High-resolution imaging modalities, such as optical coherence tomography (OCT) and ultra-widefield fundus imaging, offer detailed views of the retina and choroid, allowing for early detection and precise monitoring of fluid accumulation and retinal detachment. These imaging techniques are critical for guiding surgical procedures and evaluating treatment outcomes.
Nanotechnology for Drug Delivery
Nanotechnology provides novel approaches to delivering drugs more effectively and with fewer side effects. Nanoparticles can encapsulate drugs and deliver them directly to the site of inflammation, increasing drug concentration while decreasing systemic toxicity. Examples of nanotechnology-based drug delivery systems are:
- Liposomal Formulations: Liposomes are spherical vesicles that can encapsulate drugs, allowing for precise delivery and controlled release.
- Polymeric Nanoparticles: These nanoparticles can deliver multiple drugs at once, increasing treatment efficacy and patient compliance.
Genetic Testing
Advances in genetic testing and personalized medicine open up new possibilities for tailoring treatment strategies to individual patients. Genetic testing can identify specific genetic mutations or polymorphisms that increase the risk of uveal effusion syndrome. This data can help guide the choice of targeted therapies and optimize treatment protocols.
- Pharmacogenomics: Pharmacogenomic testing can detect genetic variations that influence drug metabolism and response, allowing for personalized dosing and the selection of the most effective medications.
Biomarker Discovery
Biomarkers are quantifiable indicators of biological processes or therapeutic responses that can help diagnose, monitor, and treat uveal effusion syndrome. Research is ongoing to identify novel biomarkers associated with uveal inflammation and fluid accumulation.
- Inflammatory Cytokines: Biomarkers like IL-6, IL-17, TNF-α, and CRP are being studied for their ability to predict disease activity and treatment response.
- MicroRNAs: MicroRNAs are small, non-coding RNA molecules that influence gene expression and inflammation. Specific microRNAs associated with uveal effusion syndrome may act as diagnostic and prognostic biomarkers.






