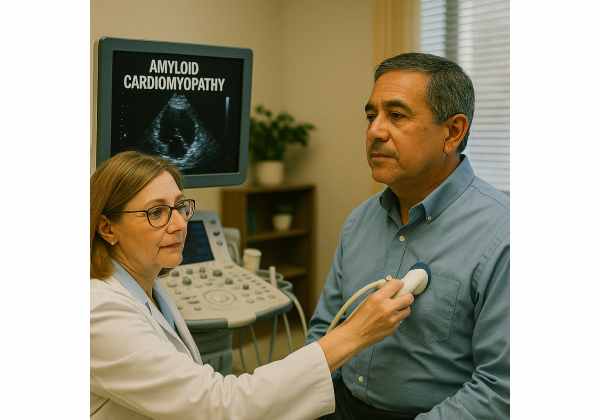
Amyloid cardiomyopathy is a complex, progressive heart disease caused by abnormal protein deposits called amyloid in the heart muscle, leading to stiffening, heart failure, and rhythm disturbances. Often overlooked or mistaken for other conditions, early recognition is vital for improving outcomes and quality of life. This article offers an in-depth, patient-centered guide to understanding amyloid cardiomyopathy—including what causes it, who is most at risk, common symptoms, current diagnostic strategies, the latest treatment approaches, and practical management advice for patients and families.
Table of Contents
- Detailed Overview of Amyloid Cardiomyopathy
- Causative Factors, Effects, and Underlying Risks
- Symptom Patterns and Diagnostic Methods
- Latest Strategies for Treatment and Management
- Frequently Asked Questions
Detailed Overview of Amyloid Cardiomyopathy
Amyloid cardiomyopathy is a form of restrictive cardiomyopathy caused by the buildup of amyloid proteins within the heart tissue. These abnormal proteins, produced elsewhere in the body or by the heart itself, deposit in the cardiac muscle and disrupt its structure and function. As amyloid accumulates, the heart becomes stiff, struggles to fill and pump blood, and may develop electrical conduction problems.
There are several types of amyloidosis that affect the heart, but the two most common are:
- AL (Light-chain) amyloidosis: Often associated with plasma cell disorders.
- ATTR (Transthyretin) amyloidosis: Can be hereditary (mutant) or age-related (wild-type).
Key characteristics of amyloid cardiomyopathy include:
- Stiff heart muscle: Unlike other forms of heart failure, the heart may not appear enlarged, but it loses flexibility.
- Progressive heart failure: Symptoms worsen over time if untreated.
- Multisystem involvement: Amyloid may affect nerves, kidneys, liver, and digestive tract.
Why early recognition is essential:
Diagnosing amyloid cardiomyopathy promptly allows for earlier therapy, potentially slowing progression and preserving heart function.
Practical advice:
If you have unexplained heart failure symptoms, especially with other issues like neuropathy, carpal tunnel, or family history, discuss amyloidosis screening with your cardiologist.
Causative Factors, Effects, and Underlying Risks
Amyloid cardiomyopathy develops when misfolded proteins accumulate in heart tissue. Understanding why this happens—and who is most at risk—can empower prevention, early diagnosis, and effective care.
What Causes Amyloid Cardiomyopathy?
The disease results from different types of amyloid proteins, most commonly:
- AL amyloidosis: Abnormal plasma cells in the bone marrow produce misfolded immunoglobulin light chains, which circulate and deposit as amyloid in organs, including the heart.
- ATTR amyloidosis:
- Hereditary ATTR (hATTR): Caused by genetic mutations in the transthyretin (TTR) gene, inherited in an autosomal dominant fashion.
- Wild-type ATTR (wtATTR): Results from age-related changes in TTR protein, seen in older adults (often over 65–70).
Less common causes include secondary (AA) amyloidosis or rare familial types.
Effects of Amyloid on the Heart
Amyloid protein deposits:
- Stiffen the myocardium: Reducing the heart’s ability to relax and fill.
- Cause thickened ventricular walls: Without the usual increase in heart chamber size.
- Disrupt electrical conduction: Leading to arrhythmias, heart block, or atrial fibrillation.
- Cause valve thickening or regurgitation.
- Impair blood supply: Amyloid can invade small coronary arteries.
Major Risk Factors
- Age: Wild-type ATTR often occurs in men over 65; hereditary forms may show up earlier.
- Genetics: Family history of amyloidosis or unexplained heart failure increases risk.
- Gender: Males are affected more frequently, especially with wild-type ATTR.
- Race/Ethnicity: Certain mutations (like V122I) are more common in people of African descent.
- Other diseases: Multiple myeloma or other plasma cell disorders (for AL amyloidosis).
- History of carpal tunnel syndrome: Can precede heart symptoms by years, especially in ATTR.
Other Organs Commonly Affected
Amyloidosis is often a multisystem disease. In addition to the heart, amyloid may affect:
- Nerves: Numbness, tingling, autonomic dysfunction.
- Kidneys: Proteinuria, kidney failure.
- Liver and spleen: Enlargement, abnormal liver function.
- Digestive system: Diarrhea, constipation, weight loss.
- Tendons and joints: Carpal tunnel syndrome, joint pain.
Practical advice:
If you or a family member develop “unusual” combinations of symptoms—heart failure with neuropathy, kidney issues, or unexplained fatigue—ask your doctor about amyloidosis.
Symptom Patterns and Diagnostic Methods
Amyloid cardiomyopathy often presents with subtle, gradually worsening symptoms. Because the disease mimics other heart and systemic illnesses, diagnosis can be delayed without a high level of suspicion.
Cardinal Symptoms
- Shortness of breath: Initially with exertion, then at rest.
- Edema: Swelling in the legs, feet, or abdomen.
- Fatigue: Persistent, often disproportionate to activity.
- Palpitations: Irregular heartbeat or fluttering sensations.
- Fainting or near-fainting: Especially with exertion or standing up.
- Chest discomfort: Less common, but possible.
Other Clues Pointing to Amyloidosis
- Bilateral carpal tunnel syndrome: Especially if both hands are affected.
- Unexplained weight loss
- Peripheral neuropathy: Numbness, tingling, or burning in the hands and feet.
- Orthostatic hypotension: Feeling faint when standing due to low blood pressure.
- Protein in urine (proteinuria): Kidney involvement.
- Easy bruising or “pinch purpura”: Skin changes, especially around the eyes.
When to Suspect Amyloid Cardiomyopathy
- Heart failure symptoms without typical risk factors.
- Heart failure with preserved ejection fraction but “thick” heart walls.
- Family history of unexplained cardiac or neurologic disease.
- Refractory arrhythmias or conduction disease in older adults.
Diagnostic Approach
1. Medical History and Physical Examination
- Focus on heart failure, neurological, and systemic symptoms.
- Family history of amyloidosis or early heart disease.
2. Electrocardiogram (ECG)
- Low voltage QRS complexes, especially with “thick” heart muscle on echo.
- Arrhythmias or conduction delays.
3. Echocardiogram
- Key findings: Thickened ventricular walls, small chambers, normal or reduced ejection fraction.
- “Sparkling” or “granular” appearance of the myocardium.
4. Blood and Urine Tests
- Markers for heart failure (BNP, NT-proBNP).
- Light chain assay (free kappa and lambda), serum and urine protein electrophoresis (for AL amyloidosis).
5. Cardiac MRI
- Offers detailed images and can detect tissue changes suggestive of amyloid.
6. Nuclear Imaging
- Bone-avid tracers (like technetium pyrophosphate scan) help differentiate ATTR from AL amyloidosis.
7. Biopsy
- Definitive diagnosis: Heart tissue, abdominal fat pad, or other organ biopsies, stained with Congo red to reveal amyloid deposits.
8. Genetic Testing
- For hereditary (ATTR) forms—helps with diagnosis and family counseling.
Differential Diagnosis:
Hypertrophic cardiomyopathy, hypertensive heart disease, aortic stenosis, or other infiltrative disorders.
Practical advice:
If you’re being evaluated for heart failure and have unusual symptoms, ask if amyloidosis has been considered.
Latest Strategies for Treatment and Management
Management of amyloid cardiomyopathy is highly specialized and depends on the type of amyloidosis and the extent of heart involvement. The primary goals are to control symptoms, slow disease progression, and address the underlying cause.
1. General Principles of Care
- Multidisciplinary team: Cardiologists, hematologists, neurologists, and genetic counselors may be involved.
- Early treatment is crucial: Outcomes are best when started before advanced heart failure or organ dysfunction.
2. Targeted Therapy Based on Amyloid Type
AL Amyloidosis
- Chemotherapy: Targets abnormal plasma cells (similar to multiple myeloma treatment). Agents may include bortezomib, cyclophosphamide, and dexamethasone.
- Autologous stem cell transplant: For selected patients.
- Supportive care: Treat heart failure symptoms carefully—patients are more sensitive to standard heart medications.
ATTR Amyloidosis
- TTR Stabilizers: Tafamidis is the first FDA-approved drug that stabilizes the TTR protein, slowing disease progression in both wild-type and hereditary ATTR.
- Gene silencers: Patisiran and inotersen reduce TTR protein production (mainly for hereditary forms).
- Experimental therapies: Ongoing trials are exploring gene editing and new stabilizers.
3. Heart Failure Management
Cautious use of standard heart failure therapies:
- Diuretics: To manage fluid overload. Start low, go slow—patients may be very sensitive.
- Beta-blockers and ACE inhibitors: Often not well-tolerated due to low blood pressure or conduction problems.
- Avoid certain medications: Calcium channel blockers and digoxin can worsen symptoms in amyloidosis.
4. Arrhythmia and Device Therapy
- Pacemakers: For patients with heart block or severe bradycardia.
- Implantable cardioverter-defibrillator (ICD): May be considered in some cases, though sudden cardiac death is often due to electromechanical dissociation, not arrhythmia.
5. Advanced Heart Failure Therapies
- Heart transplantation: An option for carefully selected patients, especially if the amyloid process can be controlled.
- Left ventricular assist device (LVAD): Rarely used due to the nature of the disease.
6. Comprehensive Supportive Care
- Monitor for multi-organ involvement: Regular screening for kidney, liver, and nerve function.
- Nutritional support: Address unintentional weight loss or gastrointestinal symptoms.
- Physical and occupational therapy: Maximize mobility and independence.
- Palliative care: Important for symptom management and quality of life in advanced disease.
7. Living With Amyloid Cardiomyopathy
- Regular follow-ups: Lifelong monitoring with a specialist.
- Lifestyle adjustments: Sodium restriction, fluid management, and energy conservation strategies.
- Family education and support: Genetic counseling for hereditary forms, psychosocial support for coping.
Practical advice:
Keep a symptoms journal, bring loved ones to appointments, and explore patient support organizations for amyloidosis.
Frequently Asked Questions
What is amyloid cardiomyopathy?
Amyloid cardiomyopathy is a heart disease where abnormal amyloid proteins build up in the heart muscle, causing it to become stiff, impairing its ability to pump blood, and leading to heart failure and rhythm problems.
What causes amyloid cardiomyopathy?
It is mainly caused by AL (light-chain) or ATTR (transthyretin) amyloidosis, which are disorders that result in misfolded proteins depositing in heart tissue.
What are the symptoms of amyloid cardiomyopathy?
Common symptoms include shortness of breath, swelling in the legs or abdomen, fatigue, irregular heartbeat, fainting, and sometimes chest discomfort. Symptoms often develop gradually and worsen over time.
How is amyloid cardiomyopathy diagnosed?
Diagnosis involves a combination of physical examination, imaging (echocardiogram, cardiac MRI), blood and urine tests, nuclear scans, and sometimes biopsy or genetic testing to confirm amyloid deposits and their type.
Is there a cure for amyloid cardiomyopathy?
There is currently no cure, but new treatments can slow progression and improve symptoms, especially if started early. Therapy depends on the amyloid type and extent of organ involvement.
What is the life expectancy with amyloid cardiomyopathy?
Life expectancy varies widely depending on the type (AL vs. ATTR), stage at diagnosis, and response to treatment. Early diagnosis and therapy can extend survival and improve quality of life.
Can amyloid cardiomyopathy be inherited?
Some forms, especially hereditary ATTR amyloidosis, are passed down in families. Genetic counseling and testing are important for family members of affected individuals.
Disclaimer:
This article is provided for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with any questions or concerns about your health.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your favorite platform, and follow us for more expert health content. Your support helps us continue delivering trusted medical information for all.










