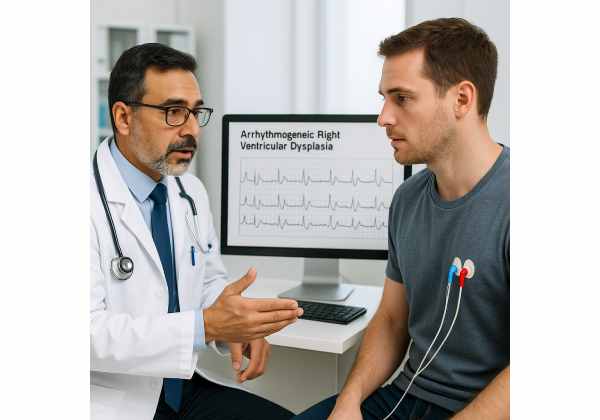
Arrhythmogenic right ventricular dysplasia (ARVD) is a rare but serious inherited heart muscle disorder, characterized by the gradual replacement of healthy right ventricular myocardium with fibrous and fatty tissue. This process disrupts normal electrical signaling in the heart, leading to potentially life-threatening arrhythmias and, in some cases, sudden cardiac death—especially among young adults and athletes. ARVD often goes undetected until a cardiac event occurs, making awareness and early intervention crucial. This in-depth guide explores the pathogenesis, causes, risk factors, clinical features, diagnosis, and current best practices for treatment and ongoing management of ARVD.
Table of Contents
- A Comprehensive Introduction to ARVD
- Causative Factors, Risk Profile, and Outcomes
- Signs, Symptoms, and Diagnostic Pathways
- Management Strategies and Therapeutic Advances
- Frequently Asked Questions
A Comprehensive Introduction to ARVD
Arrhythmogenic right ventricular dysplasia (ARVD), also known as arrhythmogenic right ventricular cardiomyopathy (ARVC), is a genetically determined disorder in which heart muscle cells in the right ventricle are gradually replaced by fibrofatty tissue. This transformation disrupts the heart’s normal electrical system, predisposing individuals to dangerous ventricular arrhythmias, syncope, and sudden cardiac death. Although often inherited in an autosomal dominant manner, not everyone who carries a gene mutation will develop symptoms, and the condition can present at any age. The right ventricle, essential for pumping blood to the lungs, becomes weakened, affecting both rhythm and function.
Key Features of ARVD:
- Genetic Roots: Inheritance is most often autosomal dominant, but genetic expression can vary widely.
- Right Ventricular Focus: The disease targets the right side of the heart, but the left ventricle may become involved over time.
- Risk of Arrhythmia: Recurrent ventricular arrhythmias are a hallmark, sometimes presenting with palpitations, syncope, or cardiac arrest.
- Variable Course: ARVD can remain silent for years, with the first event sometimes being severe.
- Impact on Active Individuals: Sudden death is tragically common in young athletes, making pre-participation screening vital.
Practical Guidance:
Anyone with a family history of ARVD, unexplained syncope, or sudden death in young relatives should seek cardiac evaluation and consider genetic testing.
Causative Factors, Risk Profile, and Outcomes
ARVD is most often rooted in genetic mutations that impact the proteins responsible for cell-to-cell adhesion in cardiac tissue. These desmosomal proteins maintain the structural integrity of heart muscle; when faulty, they allow for cellular detachment and fibrofatty replacement.
Primary Causes:
- Desmosomal Gene Mutations:
Mutations in PKP2, DSG2, DSP, DSC2, and JUP are most frequently implicated. These mutations destabilize heart muscle connections, leading to cell loss and replacement by fat and fibrous tissue. - Family History:
Inheritance is usually autosomal dominant, so having an affected parent or sibling increases risk substantially.
Secondary Factors and Disease Modifiers:
- High-Intensity Exercise:
Endurance sports accelerate disease progression and increase arrhythmia risk. - Sex:
Males are more often and more severely affected, although females may also develop the disease. - Age of Onset:
Symptoms typically begin in adolescence or young adulthood but can appear at any age.
Other Risk Contributors:
- Environmental or Viral Insults:
Although ARVD is genetic, episodes of myocarditis or other heart inflammation may unmask or worsen the disease. - Incomplete Penetrance:
Not every gene carrier develops clinical disease, but they remain at risk and can pass on the mutation.
Clinical Outcomes:
- Arrhythmias and Sudden Cardiac Death:
The most feared consequence, especially during exertion or stress. - Heart Failure:
Progressive right (and later left) ventricular dysfunction can lead to chronic heart failure. - Emotional and Social Impact:
Lifestyle restrictions, device implantation, and the psychological effects of living with a genetic disease can be profound.
Practical Advice:
If you are genetically at risk, limit intense exercise and stay in close contact with your cardiologist to monitor for early signs of disease progression.
Signs, Symptoms, and Diagnostic Pathways
ARVD’s clinical presentation varies widely. Some individuals may remain symptom-free for years, while others experience early and severe manifestations. The first sign may be a fainting episode or, tragically, sudden death—especially during or after intense physical activity.
Common Symptoms:
- Palpitations or sensations of a racing heart
- Fainting spells, often during exercise or emotional stress
- Chest discomfort or pain not related to coronary artery disease
- Progressive shortness of breath or fatigue
- Swelling in the abdomen, ankles, or legs (right-sided heart failure)
- Sudden cardiac arrest (may be the initial presentation)
Who Should Be Evaluated?
- Anyone with a family history of ARVD or sudden cardiac death
- Young individuals with unexplained fainting, palpitations, or abnormal ECGs
- Athletes experiencing exercise-induced syncope
Diagnostic Approach:
- History and Physical Examination:
Assess for symptoms, risk factors, and family history. - 12-Lead Electrocardiogram (ECG):
Looks for hallmark features such as T-wave inversions in right precordial leads, epsilon waves, and arrhythmias. - Holter or Event Monitoring:
Extended rhythm monitoring helps capture transient ventricular arrhythmias. - Echocardiography:
Evaluates right ventricular size, function, and wall motion abnormalities. May reveal thinning of the RV wall or dilation. - Cardiac MRI:
The gold standard for visualizing fibrofatty infiltration, ventricular enlargement, and wall motion abnormalities. - Genetic Testing:
Confirms diagnosis in ambiguous cases, identifies at-risk relatives, and may influence management decisions. - Electrophysiological Studies:
Used for risk stratification or ablation therapy in patients with recurrent arrhythmias. - Endomyocardial Biopsy:
Rarely performed, but can show fibrofatty replacement—though sampling errors limit its use.
Diagnostic Criteria:
A combination of major and minor criteria—including clinical, ECG, imaging, histopathology, and genetics—are used to confirm ARVD (the revised Task Force Criteria).
Practical Guidance:
Keep a log of any symptoms, and make sure your healthcare team is aware of your family’s cardiac history. Genetic counseling can empower families to make informed decisions.
Management Strategies and Therapeutic Advances
Although ARVD cannot be cured, advancements in risk assessment, arrhythmia prevention, and heart failure therapy have greatly improved outcomes. A personalized, multidisciplinary approach is essential.
Core Principles of Management:
- Prevention of Sudden Cardiac Death:
The primary goal—especially for those at high risk of ventricular arrhythmias. - Arrhythmia Suppression:
Medications and device-based therapies reduce the frequency and impact of abnormal rhythms. - Preservation of Heart Function:
Early intervention can slow the progression of right and left ventricular dysfunction.
Main Therapeutic Options:
- Lifestyle Adjustments:
- Avoid Competitive Sports:
High-intensity exercise is strongly discouraged, as it increases the risk of arrhythmias and sudden death. - Education:
Patients and families should know the symptoms of arrhythmias and the importance of regular follow-up.
- Medication Management:
- Beta-Blockers:
First-line for suppressing arrhythmic episodes and lowering adrenergic stimulation. - Antiarrhythmic Drugs (e.g., sotalol, amiodarone):
Used when arrhythmias persist despite beta-blockers. - Heart Failure Therapies:
ACE inhibitors, ARBs, diuretics, and mineralocorticoid receptor antagonists for those with reduced right or left ventricular function.
- Implantable Cardioverter-Defibrillator (ICD):
- Indications:
Patients with a history of sustained ventricular arrhythmia, cardiac arrest, or significant right ventricular dysfunction. - Benefits:
ICDs dramatically lower the risk of sudden death by detecting and treating life-threatening rhythms in real-time.
- Catheter Ablation:
- For Drug-Resistant Arrhythmias:
Ablation destroys small areas of heart tissue responsible for abnormal rhythms. Multiple procedures may be needed due to disease progression.
- Advanced Heart Failure Therapies:
- Mechanical Circulatory Support:
In advanced cases, devices like ventricular assist devices (VADs) may be considered. - Heart Transplant:
The last resort for those with refractory heart failure or intractable arrhythmias.
- Psychological and Social Support:
- Counseling:
Coping with a genetic and potentially life-threatening illness requires psychological support for patients and their families. - Support Groups:
Connecting with others facing ARVD can help reduce isolation and anxiety.
- Family Screening and Genetic Counseling:
- Testing for Relatives:
All first-degree relatives should undergo clinical and genetic assessment, even if asymptomatic.
Practical Guidance:
Always carry a medical alert ID, inform close contacts about your diagnosis and action plan, and stay informed about the latest research and support resources.
Complications to Monitor:
- Medication side effects (fatigue, bradycardia, amiodarone toxicity)
- ICD-related complications (infection, inappropriate shocks)
- Disease progression to left ventricular involvement and heart failure
Tips for Living Well with ARVD:
- Prioritize regular checkups, even when feeling well.
- Avoid over-the-counter stimulants and illicit substances.
- Maintain a heart-healthy diet and stable weight.
- Practice stress reduction—mindfulness, relaxation, and counseling can be helpful.
Frequently Asked Questions
What is arrhythmogenic right ventricular dysplasia in plain language?
Arrhythmogenic right ventricular dysplasia is a genetic disorder where heart muscle in the right ventricle is replaced by scar and fat tissue, increasing the risk of dangerous heart rhythms and sudden death.
How is ARVD usually detected?
ARVD is detected through a mix of heart imaging (MRI, echocardiogram), ECG, family history review, genetic testing, and sometimes specialized tests like electrophysiology studies.
Who is at risk for ARVD?
Those with a family history of ARVD, unexplained fainting, or sudden cardiac death—especially in young athletes—are at highest risk and should undergo screening.
What are the main symptoms of ARVD?
Common symptoms include heart palpitations, fainting (often during exercise), chest discomfort, fatigue, and, rarely, sudden cardiac arrest.
What treatments help prevent sudden death in ARVD?
The most effective measure is an implantable cardioverter-defibrillator (ICD), combined with medications, lifestyle modifications, and regular follow-up care.
Can people with ARVD play sports?
Strenuous and competitive sports should be avoided, as they increase the risk of arrhythmias and sudden cardiac death.
How does ARVD differ from other heart conditions?
ARVD is unique for its genetic origin, predominant right ventricular involvement, and strong link to exercise-induced arrhythmias and sudden death in youth.
Disclaimer
This article is provided for educational purposes only and is not a substitute for professional medical advice. If you or a loved one are concerned about ARVD or related symptoms, always consult a qualified healthcare provider. In an emergency, seek immediate medical attention.
If you found this resource helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Follow us for more trusted medical information, and support our mission by spreading awareness—your engagement empowers us to continue delivering quality content!






