Atrioventricular dissociation is a distinctive cardiac rhythm abnormality in which the electrical activity of the atria and ventricles becomes independent, leading to a lack of synchronized heartbeat. While this condition may be benign or asymptomatic in some cases, it can also indicate underlying heart disease or contribute to significant symptoms such as dizziness or syncope. Understanding the mechanisms, triggers, diagnostic tools, and management options for atrioventricular dissociation is crucial for patients and clinicians alike. This comprehensive resource will empower you with the most up-to-date information, practical tips, and expert guidance to help navigate this complex heart rhythm disorder.
Table of Contents
- Understanding Atrioventricular Dissociation
- Causal Factors, Risk Groups, and Physiological Impact
- Key Symptoms and Diagnostic Strategies
- Modern Treatment Approaches and Continuing Care
- Frequently Asked Questions
Understanding Atrioventricular Dissociation
Atrioventricular (AV) dissociation is a type of cardiac arrhythmia in which the atria and ventricles beat independently, each driven by its own pacemaker. Unlike the normal heart rhythm—where the electrical impulse starts in the atria (at the sinoatrial node) and travels through the AV node to stimulate the ventricles—AV dissociation reflects a breakdown in this communication, resulting in the atria and ventricles contracting out of sync.
How AV Dissociation Differs From Other Heart Rhythms
- Normal Rhythm: The SA node paces the atria and controls the ventricles via the AV node.
- AV Dissociation: The atria and ventricles have separate pacemakers and rhythms, with no consistent electrical relationship.
- Not Always Block: It’s not always due to a “block” of the AV node; it may occur because a ventricular pacemaker is faster than the atrial rate, or due to other rhythm disturbances.
Types of AV Dissociation
- Isorhythmic AV Dissociation: The atrial and ventricular rates are similar, but not linked.
- Interference AV Dissociation: An “intruder” pacemaker (often ventricular) suppresses normal conduction.
- Complete AV Dissociation (often with complete AV block): The atria and ventricles function entirely independently.
Clinical Significance
AV dissociation may occur transiently or persistently. It can be:
- Benign (e.g., in athletes or during sleep)
- Pathological (related to heart disease, drug toxicity, or metabolic derangements)
Recognizing and interpreting AV dissociation is important, as it can signal underlying or impending cardiac issues.
Epidemiology
- Seen across all age groups but more common in older adults and those with underlying cardiac conditions.
- Sometimes observed temporarily in otherwise healthy people during sleep, anesthesia, or high vagal tone.
Importance of Early Recognition
Although some cases are incidental, others may predict dangerous arrhythmias or serious conduction disease, making vigilance and early evaluation essential.
Causal Factors, Risk Groups, and Physiological Impact
To fully understand atrioventricular dissociation, it is vital to explore its causes, predisposing factors, and the physiological changes it produces.
What Causes AV Dissociation?
1. Accelerated Ectopic Pacemakers
- A faster secondary pacemaker (often in the ventricles) suppresses normal atrial signals.
- Examples: Accelerated idioventricular rhythm after heart attack.
2. AV Node Dysfunction
- Diseases or damage affecting the AV node (fibrosis, ischemia, degeneration) can impair conduction from atria to ventricles.
3. Drug Effects and Toxicities
- Medications such as beta-blockers, calcium channel blockers, digoxin, or antiarrhythmic drugs can depress AV conduction or alter pacemaker rates.
4. Metabolic and Systemic Causes
- Electrolyte imbalances (hyperkalemia, hypokalemia), hypoxia, hypothyroidism, or acute illness.
5. Increased Vagal Tone
- Seen in healthy individuals during sleep, athletes at rest, or due to vomiting or carotid massage.
6. Cardiac Surgery or Trauma
- Procedures near the conduction system can disrupt normal rhythms.
7. Cardiac Structural Disease
- Cardiomyopathy, myocarditis, amyloidosis, or infiltrative diseases.
8. Ischemic Heart Disease
- Heart attacks, especially involving the inferior wall, may lead to AV dissociation.
Risk Factors for AV Dissociation
- Advanced age
- Pre-existing conduction system disease (bundle branch block, previous heart block)
- Recent cardiac surgery or myocardial infarction
- Use of AV-nodal blocking medications
- Chronic kidney disease (due to electrolyte disturbances)
- Underlying structural heart disease
Physiological Consequences
- Loss of atrial “kick” (the boost to ventricular filling from coordinated atrial contraction)
- Reduced cardiac output and potential for hypotension
- Variable ventricular rates—can be slow (bradycardia) or normal
- Risk of progression to complete heart block or dangerous arrhythmias
Complications
- Syncope (fainting)
- Heart failure symptoms
- Exacerbation of angina or underlying cardiac disease
- Sudden cardiac arrest in severe cases
Preventive Strategies and Patient Advice
- Regular review of medications by a healthcare provider.
- Prompt evaluation of new dizziness, syncope, or palpitations.
- Monitoring in patients with high risk, especially post-cardiac surgery or heart attack.
Key Symptoms and Diagnostic Strategies
Symptoms of atrioventricular dissociation depend on the underlying cause, the rates of atrial and ventricular contraction, and the degree of cardiac output impairment.
Recognizing the Signs
- Mild or Asymptomatic: Some people, especially athletes, may have no symptoms.
- Palpitations: Sensation of irregular, forceful, or missed heartbeats.
- Dizziness or Lightheadedness: Caused by momentary drops in cardiac output.
- Syncope (Fainting): Particularly with profound bradycardia or loss of ventricular output.
- Chest Discomfort or Shortness of Breath: Especially if cardiac output drops or underlying heart disease exists.
- Fatigue and Reduced Exercise Capacity: Chronic or intermittent in nature.
Physical Exam Findings
- Variable pulse: Irregular, sometimes with “cannon A waves” (forceful jugular venous pulsations)
- Bradycardia: Slow heart rate may be detected
- Blood pressure fluctuations
- Murmurs or gallops may be present if associated valve disease or heart failure exists
Diagnostic Process
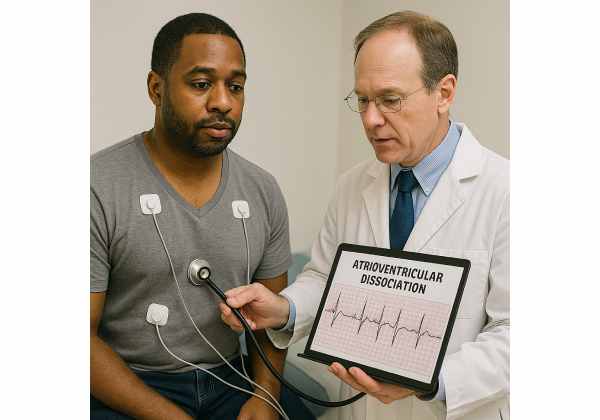
1. Electrocardiogram (ECG/EKG)
- Cornerstone test—shows independent atrial (P wave) and ventricular (QRS complex) activity.
- Helpful for distinguishing AV dissociation from other rhythm abnormalities.
2. Ambulatory Cardiac Monitoring
- Holter monitor or event recorder to catch intermittent episodes.
3. Electrophysiology Study
- In select cases, an invasive test to map conduction and guide therapy.
4. Echocardiogram
- Assesses cardiac structure, function, and underlying disease.
5. Laboratory Evaluation
- Electrolyte levels, drug levels, thyroid function, and markers of myocardial injury.
6. Additional Imaging
- MRI or CT for suspected infiltrative or structural heart disease.
Differential Diagnosis
- Third-degree (complete) AV block (similar ECG, but different mechanism)
- Junctional rhythms
- Idioventricular or ventricular escape rhythms
- Sinus node dysfunction
Tips for Patients
- Keep a detailed log of symptoms and what triggers them.
- Bring all current medications to your appointments.
- Report any new fainting episodes, chest pain, or rapid heartbeats urgently.
Modern Treatment Approaches and Continuing Care
Effective management of AV dissociation targets the underlying cause, symptom relief, and prevention of complications.
Acute Management
1. Hemodynamically Unstable Patients
- Immediate intervention—may require temporary pacing, intravenous atropine, or advanced cardiac life support protocols.
- Correction of reversible causes (electrolytes, drug toxicity, hypoxia).
2. Hemodynamically Stable or Mildly Symptomatic
- Observation and monitoring.
- Adjust or discontinue medications affecting AV conduction.
3. Specific Therapies Based on Etiology
- Drug-induced: Withdrawing or adjusting offending drugs.
- Post-surgical: Supportive care, pacing if needed.
Permanent Solutions
1. Pacemaker Implantation
- Indicated for symptomatic or persistent AV dissociation with significant bradycardia.
- Pacemakers restore normal AV synchrony and prevent recurrence of dangerous pauses.
2. Treating Underlying Conditions
- Ischemic heart disease: Revascularization, medications.
- Cardiomyopathy or infiltrative disease: Disease-specific therapies.
- Infections: Antibiotics or antiviral therapies.
Long-Term Management and Monitoring
- Routine Cardiology Follow-Up: Regular check-ups, device checks if a pacemaker is placed.
- Lifestyle Adjustments:
- Avoid dehydration, extreme exertion unless cleared by your doctor.
- Manage chronic conditions (diabetes, hypertension).
- Medication Review: Frequent re-evaluation for drug interactions and effects on heart rhythm.
Prognosis
- Benign in many cases (especially in healthy young people or athletes).
- Prognosis depends on the underlying cause and promptness of intervention.
- With a pacemaker, many people can return to full, active lives.
Innovations in Care
- MRI-compatible pacemakers
- Leadless pacemaker technology
- Remote monitoring for arrhythmia and device function
- Ongoing research into biological pacing and regenerative therapies
Patient Empowerment and Support
- Ask your provider about your risk for recurrence or progression to complete heart block.
- Consider wearing a medical alert bracelet if you have a device or are at risk for rhythm disturbances.
- Engage in regular exercise and heart-healthy habits, with medical guidance.
Frequently Asked Questions
What is atrioventricular dissociation in the heart?
Atrioventricular dissociation is a heart rhythm abnormality where the atria and ventricles beat independently of each other, often due to separate pacemaker activity or conduction block.
What causes atrioventricular dissociation?
Causes include heart disease, drug toxicity, increased vagal tone, electrolyte disturbances, cardiac surgery, or a fast ectopic pacemaker overriding the normal rhythm.
What are the symptoms of atrioventricular dissociation?
Symptoms may be absent, but can include palpitations, dizziness, fainting, chest pain, fatigue, or shortness of breath, especially if the heart’s output is reduced.
How is atrioventricular dissociation diagnosed?
Diagnosis is confirmed by ECG, which shows independent atrial (P wave) and ventricular (QRS) activity. Additional monitoring and cardiac tests help clarify the cause and guide treatment.
What is the treatment for atrioventricular dissociation?
Treatment depends on the cause and symptoms. Mild cases may need no intervention. Severe or symptomatic cases may require pacemaker implantation or correction of underlying issues.
Is atrioventricular dissociation dangerous?
It can be benign in healthy people, but in others it may signal serious heart disease or risk of sudden cardiac arrest. Timely evaluation is important for safety.
Can atrioventricular dissociation go away?
Some cases are temporary, especially if caused by drugs or acute illness, and resolve when the trigger is removed. Persistent or symptomatic cases often require ongoing care.
Disclaimer:
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with questions regarding any medical condition.
If you found this article valuable, please share it on Facebook, X (formerly Twitter), or your preferred social network. Support our mission by spreading reliable health information—your help allows us to keep creating trusted, expert-led content for everyone.










