Atrioventricular tachycardia (AVT) is a type of supraventricular tachycardia characterized by an abnormally rapid heart rhythm that originates from electrical circuits involving the atrioventricular (AV) node. This arrhythmia can affect people of any age and often presents with palpitations, dizziness, or episodes of rapid heartbeat that can be unsettling and, in rare cases, dangerous. AVT encompasses various subtypes, each with its own triggers and underlying mechanisms. With early diagnosis, effective treatment, and lifestyle adjustments, most individuals can manage AVT well and maintain a healthy, active life. This article provides a detailed, accessible guide to understanding, diagnosing, and treating AVT.
Table of Contents
- Understanding Atrioventricular Tachycardia in Depth
- Causal Factors, Health Impact, and Risk Elements
- Detecting Signs and Comprehensive Diagnosis
- Modern Management and Therapeutic Strategies
- Frequently Asked Questions
Understanding Atrioventricular Tachycardia in Depth
Atrioventricular tachycardia (AVT) is a rapid heart rhythm disturbance that results from electrical signals repeatedly circulating within or around the atrioventricular node—the area connecting the heart’s upper and lower chambers. Unlike normal heart rhythms that begin in the sinoatrial (SA) node, AVT arises from abnormal electrical pathways.
Types of Atrioventricular Tachycardia
- Atrioventricular Nodal Reentrant Tachycardia (AVNRT): Most common, involving a dual pathway within the AV node.
- Atrioventricular Reentrant Tachycardia (AVRT): Involves an extra pathway outside the AV node, such as in Wolff-Parkinson-White (WPW) syndrome.
- Other Forms: Rare or atypical pathways can also trigger AVT.
How AVT Affects the Heart
- Heart Rate: Can cause heart rates from 140–250 beats per minute.
- Blood Flow: Rapid rhythm can impair the heart’s ability to pump blood efficiently.
- Symptoms: Vary from mild to severe, sometimes triggering fainting or chest pain.
Who Is at Risk?
- AVT can occur in children, teens, adults, and seniors—sometimes with no apparent cause.
- Individuals with congenital heart defects or a family history of arrhythmias have higher risk.
Practical Advice
- Keep a log of episodes, symptoms, and potential triggers.
- Learn and practice vagal maneuvers (like the Valsalva maneuver) to help stop an episode at home.
Causal Factors, Health Impact, and Risk Elements
Uncovering why AVT happens and what makes some people more vulnerable helps families and patients understand the condition and prevent complications.
Primary Causes
- Congenital Abnormalities: Some people are born with extra electrical pathways in their hearts.
- Genetic Factors: Family history increases risk, and certain genes may predispose individuals to AVT.
- Heart Surgery or Structural Disease: Scarring from surgery or cardiomyopathies can form abnormal conduction pathways.
- Other Medical Conditions: Electrolyte imbalances, thyroid disorders, and stimulant use (such as caffeine or decongestants) can provoke AVT episodes.
Risk Factors
- Age: While AVT can develop at any age, some forms are more common in young adults and middle-aged people.
- Gender: Slightly more common in women, especially AVNRT.
- Lifestyle Factors: High stress, excessive alcohol, stimulants, and sleep deprivation may trigger episodes.
- Other Arrhythmias: Co-existing heart rhythm problems increase the likelihood of AVT.
Potential Health Impact
- Palpitations and Discomfort: Most AVT episodes cause noticeable, sometimes distressing palpitations.
- Reduced Exercise Tolerance: Prolonged or frequent episodes can cause fatigue, dizziness, or fainting.
- Heart Failure Risk: Rare but possible, especially in people with underlying heart disease.
- Blood Clot Risk: Very rapid heart rates increase the risk of blood clots in susceptible patients.
Preventive and Proactive Steps
- Avoid known personal triggers—keep a symptom diary to help identify patterns.
- Manage other health problems, especially high blood pressure, thyroid disease, and diabetes.
- Adopt stress-reduction techniques such as mindfulness, yoga, or deep breathing.
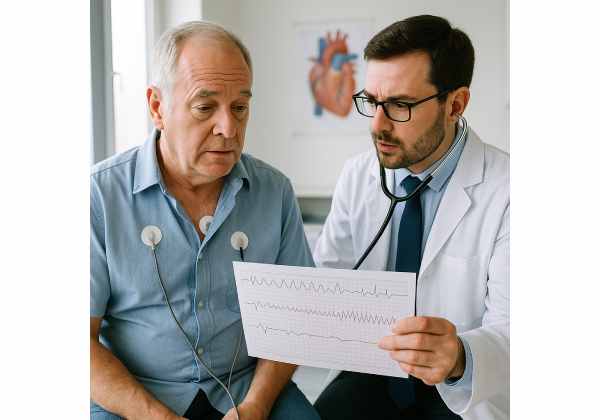
Detecting Signs and Comprehensive Diagnosis
Timely recognition and an accurate diagnosis are key to preventing complications and ensuring effective treatment for AVT.
Common Symptoms
- Palpitations: Sudden, rapid heartbeat—sometimes described as “fluttering” or “racing.”
- Dizziness or Lightheadedness: Especially during or after an episode.
- Shortness of Breath: May occur during intense episodes or with underlying heart disease.
- Chest Pain or Discomfort: Sometimes present, but always warrants prompt medical attention.
- Fainting (Syncope): Rare but possible in severe or prolonged episodes.
- Fatigue or Weakness: Especially if episodes are frequent.
When to Seek Emergency Care
- If you experience chest pain, fainting, or symptoms lasting longer than 20–30 minutes.
- If your symptoms occur with existing heart disease or other risk factors.
Diagnostic Tests
1. Physical Examination:
- Listen for fast heart rhythms, irregular pulses, or other cardiac signs.
2. Electrocardiogram (ECG/EKG):
- Essential for identifying the type of tachycardia during an episode.
3. Ambulatory ECG Monitoring (Holter or Event Monitor):
- Records heart rhythm over days or weeks to capture intermittent episodes.
4. Echocardiogram:
- Assesses heart structure and function, rules out underlying disease.
5. Electrophysiology Study (EPS):
- An invasive test to pinpoint the abnormal pathway and plan treatment, usually for recurrent or severe AVT.
Differential Diagnoses
- Sinus tachycardia
- Atrial fibrillation or atrial flutter
- Ventricular tachycardia
- Panic attacks (sometimes mimic symptoms)
Patient-Friendly Tips
- Ask your doctor about wearing a mobile ECG patch or using a smartphone ECG device for home monitoring.
- Stay hydrated and avoid excessive caffeine, as dehydration and stimulants can trigger episodes.
Modern Management and Therapeutic Strategies
Effective management of AVT blends immediate care, long-term treatment, and practical self-care strategies for daily living.
Acute Episode Management
- Vagal Maneuvers: Actions like bearing down, coughing, or applying ice to the face can sometimes terminate an episode.
- Medications: Intravenous adenosine or other antiarrhythmics in the emergency department for acute termination.
- Cardioversion: Rarely needed; used if unstable or unresponsive to other measures.
Long-Term Medical Therapy
- Beta Blockers or Calcium Channel Blockers: Help control heart rate and prevent recurrences.
- Antiarrhythmic Drugs: For persistent or frequent AVT not controlled by standard medications.
- Lifestyle Adjustments:
- Reduce caffeine and alcohol.
- Practice regular stress reduction.
- Prioritize consistent sleep.
Catheter Ablation
1. What It Is:
- A minimally invasive procedure that uses radiofrequency energy to destroy abnormal electrical pathways.
2. Success Rate: - High success (over 95% in many centers), often curative.
3. Who Should Consider It: - Recommended for people with frequent, severe, or medication-resistant AVT.
Living with AVT
- Regular Cardiology Follow-Up: Annual checkups or as advised.
- Physical Activity: Most people can exercise; check with your doctor for individual recommendations.
- Emergency Plan: Have a clear plan for what to do during an episode—carry a card or alert device if needed.
Special Considerations
- Children and Young Adults: May outgrow some forms of AVT or need ablation.
- Pregnancy: Discuss with your doctor, as AVT may require tailored management during pregnancy.
- Older Adults: Monitor for medication side effects or co-existing arrhythmias.
Practical Self-Care Advice
- Track your symptoms in a journal or app—this helps your healthcare team fine-tune your care.
- Share information about your condition with close friends or family so they can help in emergencies.
Frequently Asked Questions
What is atrioventricular tachycardia (AVT)?
Atrioventricular tachycardia (AVT) is a rapid heart rhythm originating from abnormal electrical circuits involving the AV node. It causes episodes of fast, sometimes irregular heartbeats.
How is AVT diagnosed?
Diagnosis is based on ECG findings during an episode and sometimes ambulatory monitoring to capture intermittent events. Additional heart tests may be required.
Can AVT be life-threatening?
AVT is rarely life-threatening but can cause significant symptoms and, in rare cases, complications if untreated or present with other heart conditions.
What are the main treatments for AVT?
Treatments include vagal maneuvers, medications, and catheter ablation for curative therapy in many cases. Management depends on frequency and severity.
Are there lifestyle changes to reduce AVT episodes?
Yes, avoiding stimulants, managing stress, ensuring adequate hydration, and regular sleep help reduce episodes in many people.
Can AVT recur after ablation?
While catheter ablation is highly effective, a small number of people may experience recurrences and need repeat procedures or medication.
Is AVT the same as atrial fibrillation?
No, AVT and atrial fibrillation are distinct arrhythmias. AVT involves the AV node; atrial fibrillation arises from chaotic activity in the atria.
Disclaimer:
This article is intended for educational purposes only and should not replace medical advice from your healthcare provider. If you have symptoms or concerns, always consult a qualified health professional.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your favorite social network. Follow us for more trusted health content, and help us support others by sharing this information!










