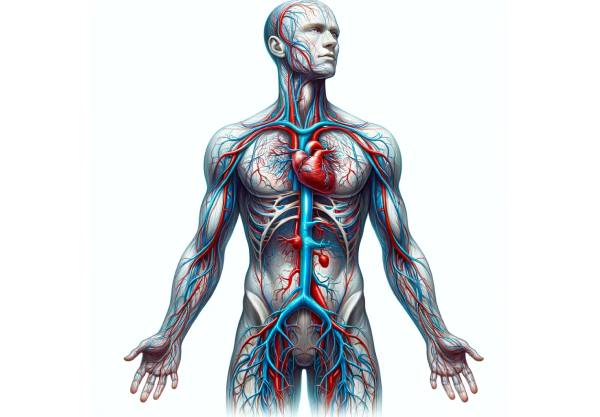
Blood vessels are the dynamic network of conduits that transport blood throughout the human body. They include arteries, veins, and capillaries—each uniquely structured to fulfill its role in the circulation of oxygen, nutrients, and waste products. Their robust design supports high-pressure blood flow, while their flexibility ensures efficient distribution, regulation, and exchange at the cellular level. Understanding the detailed anatomy and physiology of blood vessels is essential for diagnosing and treating cardiovascular diseases. This guide offers an in-depth exploration of blood vessel structure, examines common vascular disorders, reviews state-of-the-art diagnostic and treatment techniques, and provides actionable lifestyle tips and nutritional strategies for optimal vascular health.
Table of Contents
- Anatomical Details
- Vessel Physiology & Functions
- Common Vascular Disorders
- Diagnostic Methods
- Treatment Options
- Nutritional & Supplementary Strategies
- Lifestyle & Preventive Tips
- Reliable Resources
- Frequently Asked Questions
Anatomical Details of Blood Vessels
Blood vessels are the structural framework of the circulatory system and are categorized into arteries, veins, and capillaries—each with specialized architecture designed for specific functions.
Arteries
Arteries carry oxygenated blood away from the heart to the tissues. Their walls are thick and robust to withstand high pressure. They are composed of three layers:
- Tunica Intima:
This innermost layer consists of a single layer of endothelial cells that creates a smooth, frictionless surface. It also contains a thin basement membrane that supports cellular adhesion and regulates permeability. - Tunica Media:
The middle layer is rich in smooth muscle cells and elastic fibers. In large arteries such as the aorta, elastic fibers allow the vessel to expand and recoil with each heartbeat, buffering the pulsatile output. In smaller arteries and arterioles, a greater proportion of smooth muscle facilitates precise regulation of blood flow through vasoconstriction and vasodilation. - Tunica Externa (Adventitia):
The outer layer, composed primarily of connective tissue and collagen, provides structural support and protection. It also houses small blood vessels (vasa vasorum) that nourish the arterial wall and nerves that regulate vessel tone.
Veins
Veins transport deoxygenated blood back to the heart under lower pressure. Their structure differs markedly from arteries:
- Tunica Intima:
Veins are lined with endothelial cells, and many veins—especially in the lower extremities—contain valves that prevent backflow, ensuring unidirectional blood movement towards the heart. - Tunica Media:
The muscular layer in veins is thinner and contains fewer smooth muscle cells compared to arteries. This reduced muscularity reflects the lower pressure in the venous system. - Tunica Externa:
In veins, this layer is typically thicker than the tunica media and is composed of collagen-rich connective tissue that anchors the vessel to surrounding tissues, preventing excessive distension.
Capillaries
Capillaries are the smallest and most abundant vessels where the exchange of gases, nutrients, and waste occurs.
- Single Endothelial Layer:
Capillaries consist of a thin layer of endothelial cells, which minimizes the distance for diffusion, enabling efficient exchange between blood and tissues. - Basement Membrane:
A delicate basement membrane supports the endothelial layer and plays a role in filtration. - Permeability Variations:
Capillaries can be continuous, fenestrated, or sinusoidal—each type is specialized for different levels of permeability to meet the demands of various tissues.
Microcirculation
The microcirculation system encompasses arterioles, capillaries, and venules. Arterioles regulate blood entry into capillary beds through constriction and dilation, ensuring that blood flow is adjusted according to local tissue metabolic needs.
Specialized Vessels
Certain vessels have unique structures:
- Coronary Arteries: Supply the heart muscle with oxygen-rich blood.
- Pulmonary Vessels: Include the pulmonary arteries (carrying deoxygenated blood to the lungs) and pulmonary veins (returning oxygenated blood to the heart).
- Portal Veins: Transport nutrient-rich blood from the gastrointestinal tract to the liver for processing.
In summary, the detailed architecture of blood vessels—from thick, elastic arterial walls to the thin, permeable structure of capillaries—underpins their ability to deliver oxygen and nutrients while efficiently removing waste. This sophisticated design is crucial for sustaining life and adapting to various physiological demands.
Vessel Physiology & Functions
The primary function of blood vessels is to ensure the continuous and efficient circulation of blood throughout the body. This section explores how arteries, veins, and capillaries work together to maintain vascular function and overall homeostasis.
Oxygen and Nutrient Delivery
- Arterial Transport:
Arteries transport oxygen-rich blood and nutrients from the heart to the tissues. The smooth, elastic walls of arteries not only allow them to withstand high pressure but also enable rapid distribution of blood during increased physical activity. - Capillary Exchange:
At the capillary level, the close proximity between blood and tissues allows for the diffusion of oxygen and nutrients into cells, while waste products like carbon dioxide are removed and transported back to the lungs and kidneys.
Regulation of Blood Pressure
Blood vessels play a critical role in controlling blood pressure through several mechanisms:
- Vasoconstriction and Vasodilation:
Smooth muscle cells in the tunica media adjust the diameter of blood vessels in response to neural and hormonal signals. Vasoconstriction increases blood pressure, whereas vasodilation decreases it. - Elastic Recoil:
In large elastic arteries, the capacity to stretch and recoil helps dampen the pulsatile output of the heart, ensuring a more continuous blood flow. - Baroreceptor Reflex:
Specialized receptors in arterial walls, such as those in the carotid sinus and aortic arch, sense changes in blood pressure and trigger reflex adjustments via the autonomic nervous system.
Distribution of Blood Flow
- Regional Regulation:
Blood vessels are adept at directing blood flow to tissues based on their metabolic demands. For example, during exercise, arteries supplying skeletal muscles dilate, while those supplying the gastrointestinal tract constrict. - Microcirculation Control:
Precapillary sphincters regulate the flow of blood into capillary beds, ensuring that active tissues receive increased oxygen and nutrients.
Waste Removal and Thermoregulation
- Venous Return:
Veins return deoxygenated blood and metabolic waste products to the heart, where blood is then pumped to the lungs or kidneys for filtration and excretion. - Heat Exchange:
Blood vessels, particularly those close to the skin, help regulate body temperature by controlling heat dissipation. In warm conditions, vasodilation increases blood flow to the skin to release heat, while in cold conditions, vasoconstriction conserves heat.
Endothelial Function
The endothelium, a critical layer lining all blood vessels, plays a multifaceted role:
- Barrier and Selective Permeability:
It regulates the passage of substances between the blood and surrounding tissues. - Vasoactive Substance Production:
Endothelial cells produce nitric oxide and endothelin, which are crucial for vascular tone regulation. - Inflammatory Modulation and Coagulation:
The endothelium helps mediate inflammatory responses and maintains a balance between clotting and bleeding.
Overall, the physiology of blood vessels is intricately designed to maintain efficient circulation, regulate blood pressure, and facilitate the exchange of vital substances. Their coordinated functions are central to sustaining life and ensuring that the body’s tissues are well nourished and free from waste.
Common Vascular Disorders
Various conditions can affect blood vessels, leading to serious cardiovascular complications. This section reviews prevalent vascular disorders, their underlying mechanisms, clinical presentations, and potential complications.
Atherosclerosis
Atherosclerosis is a chronic condition marked by the buildup of plaques within arterial walls.
- Pathogenesis:
Endothelial injury initiates a cascade of lipid accumulation, inflammatory cell infiltration, and fibrous tissue formation. Over time, these plaques narrow the arterial lumen and reduce blood flow. - Clinical Consequences:
Atherosclerosis can lead to coronary artery disease (causing angina or heart attacks), peripheral artery disease (resulting in leg pain and mobility issues), and carotid artery disease (increasing stroke risk).
Hypertension
High blood pressure exerts continuous stress on the vascular system.
- Mechanism:
Persistent elevation in blood pressure damages the endothelial lining and promotes arterial stiffening. Over time, this can lead to vascular remodeling and increased risk of cardiovascular events. - Complications:
Chronic hypertension is associated with heart failure, kidney disease, and an increased risk of stroke.
Aneurysms
An aneurysm is an abnormal dilation of a blood vessel due to weakening of its wall.
- Types:
Aneurysms can be saccular (berry-shaped) or fusiform (spindle-shaped). They most commonly affect the aorta and cerebral arteries. - Risks:
Rupture of an aneurysm can cause catastrophic internal bleeding, often with fatal outcomes if not promptly treated. - Management:
Early detection and repair—via surgical or endovascular techniques—are critical to prevent rupture.
Peripheral Artery Disease (PAD)
PAD results from atherosclerosis in the arteries supplying the limbs.
- Symptoms:
Patients commonly experience claudication, characterized by pain or cramping in the legs during exercise due to insufficient blood flow. - Progression:
Severe cases can lead to critical limb ischemia, ulcers, and even gangrene. - Treatment:
Lifestyle modifications, medications, and revascularization procedures help manage symptoms and improve circulation.
Venous Disorders
Venous disorders are often related to impaired blood return to the heart.
- Varicose Veins:
Incompetent venous valves lead to dilated, tortuous veins, especially in the legs, causing discomfort and cosmetic concerns. - Chronic Venous Insufficiency (CVI):
Prolonged venous hypertension results in skin changes, edema, and ulceration. - Deep Vein Thrombosis (DVT):
The formation of clots in deep veins, typically in the legs, can lead to pulmonary embolism if the clot dislodges.
Raynaud’s Phenomenon
Raynaud’s phenomenon is characterized by episodic vasospasm of small vessels, particularly in the fingers and toes.
- Triggers:
Exposure to cold temperatures or emotional stress can provoke the condition. - Manifestations:
Affected areas typically undergo color changes (white, blue, then red), accompanied by numbness and pain.
Vasculitis
Vasculitis involves inflammation of blood vessel walls.
- Etiology:
It can be idiopathic or associated with autoimmune conditions, infections, or medications. - Effects:
Inflammation can lead to vessel narrowing, blockage, or aneurysm formation, with symptoms depending on the vessels involved.
Understanding these vascular disorders is essential for early diagnosis and intervention. Effective management can significantly reduce the risk of severe complications and improve overall cardiovascular health.
Diagnostic Methods for Vascular Health
Accurate diagnosis of vascular disorders relies on a blend of clinical evaluation, imaging studies, and functional tests. These methods are crucial for determining the extent of vascular damage and guiding treatment decisions.
Clinical Evaluation
- Medical History and Physical Examination:
A detailed patient history—including symptoms such as chest pain, leg pain, or swelling—is taken. Physical examination assesses pulses, blood pressure, and any visible vascular abnormalities (e.g., varicosities, skin changes). - Risk Factor Assessment:
Factors such as smoking, diabetes, hypertension, and high cholesterol are evaluated to determine cardiovascular risk.
Laboratory Tests
- Blood Tests:
Lipid profiles, blood glucose levels, and inflammatory markers (e.g., C-reactive protein) are measured to assess the risk of atherosclerosis and other vascular conditions. - Biomarkers:
Specific biomarkers may be used to gauge vascular inflammation and endothelial dysfunction.
Imaging Techniques
- Doppler Ultrasound:
A non-invasive technique that uses sound waves to evaluate blood flow and detect blockages or narrowing in arteries and veins. It is particularly useful for diagnosing PAD and DVT. - Duplex Ultrasound:
Combines traditional ultrasound and Doppler to produce detailed images and measure blood flow velocity. - CT Angiography (CTA):
Utilizes computed tomography and contrast dye to generate high-resolution images of blood vessels, ideal for detecting aneurysms, blockages, and plaque buildup. - Magnetic Resonance Angiography (MRA):
Uses magnetic fields and radio waves to produce detailed vascular images without ionizing radiation, suitable for patients requiring frequent imaging. - Conventional Angiography:
An invasive procedure where contrast dye is injected into blood vessels, and X-ray imaging is used to visualize arterial blockages and malformations. It remains the gold standard for coronary artery assessment.
Functional and Advanced Tests
- Ankle-Brachial Index (ABI):
This simple test compares blood pressure in the ankles and arms to diagnose peripheral artery disease. - Exercise Stress Testing:
Assesses cardiovascular function under physical stress, revealing ischemic changes that might not be present at rest. - Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT):
These techniques provide detailed images of the arterial wall and plaque composition, aiding in treatment planning for coronary interventions.
Through these diagnostic approaches, clinicians can obtain a comprehensive picture of vascular health, ensuring that treatment plans are precisely tailored to the individual’s condition.
Treatment Options and Interventions
Effective management of vascular disorders involves a combination of lifestyle modifications, medications, minimally invasive procedures, and, in some cases, surgical interventions. The goal is to restore optimal blood flow, reduce complications, and improve quality of life.
Lifestyle Modifications
- Diet:
Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limiting sodium and trans fats helps manage blood pressure and cholesterol. - Exercise:
Regular physical activity enhances circulation, improves arterial elasticity, and helps maintain a healthy weight. - Smoking Cessation:
Quitting smoking is one of the most effective ways to prevent arterial damage and reduce the risk of atherosclerosis. - Weight Management and Stress Reduction:
Maintaining a healthy weight and managing stress through techniques such as meditation or yoga can have a significant positive impact on vascular health.
Pharmacological Therapies
- Antihypertensive Medications:
ACE inhibitors, beta-blockers, and calcium channel blockers help lower blood pressure and reduce stress on the vascular system. - Statins:
These medications lower LDL cholesterol and stabilize plaques, slowing the progression of atherosclerosis. - Antiplatelet Agents and Anticoagulants:
Drugs like aspirin, clopidogrel, and warfarin help prevent clot formation, reducing the risk of heart attack, stroke, and deep vein thrombosis. - Vasodilators:
Medications such as nitroglycerin improve blood flow by relaxing and dilating blood vessels.
Minimally Invasive Procedures
- Angioplasty and Stenting:
A balloon catheter is used to widen narrowed arteries, and a stent is placed to keep the vessel open, improving blood flow in coronary and peripheral arteries. - Endovenous Ablation:
Laser or radiofrequency techniques are used to treat varicose veins, restoring proper venous circulation. - Thrombectomy:
Clot-removal procedures can rapidly restore blood flow in cases of acute deep vein thrombosis or arterial occlusion.
Surgical Interventions
- Bypass Surgery:
Creating a bypass around a blocked artery using a graft can restore blood flow to critical areas, particularly in coronary artery disease. - Endarterectomy:
The surgical removal of plaque from an artery, typically performed on carotid arteries to reduce stroke risk. - Aneurysm Repair:
Aneurysms may be repaired either by open surgery or through endovascular stent grafts to prevent rupture.
Emerging Therapies
- Gene and Stem Cell Therapies:
Research is underway to develop treatments that target genetic causes of vascular disease and regenerate damaged vessel tissue. - Novel Antioxidant and Anti-inflammatory Agents:
New drugs aimed at reducing oxidative stress and inflammation are being investigated to improve endothelial function and prevent plaque progression.
A personalized approach that integrates lifestyle changes with appropriate medical and surgical treatments is crucial for managing vascular disorders and maintaining long-term cardiovascular health.
Nutritional & Supplementary Strategies
Nutritional support plays a key role in vascular health. A diet rich in essential nutrients, combined with targeted supplements, can help reduce inflammation, improve endothelial function, and promote overall cardiovascular well-being.
Essential Nutrients
- Omega-3 Fatty Acids:
Found in fish oil and flaxseeds, these fatty acids help reduce inflammation and support the elasticity of blood vessels. - Coenzyme Q10 (CoQ10):
This antioxidant is vital for energy production in cells and helps protect the endothelium from oxidative damage. - Magnesium:
Essential for vascular relaxation, magnesium aids in maintaining healthy blood pressure and preventing arterial stiffness. - Vitamins C and E:
These antioxidants help neutralize free radicals, protecting blood vessel walls and supporting collagen production for structural integrity.
Herbal Supplements
- Garlic Extract:
Known for its cardiovascular benefits, garlic can help lower blood pressure, reduce plaque formation, and improve overall vascular function. - Turmeric (Curcumin):
With powerful anti-inflammatory properties, curcumin helps reduce vascular inflammation and supports endothelial health. - Green Tea Extract:
Rich in catechins, green tea extract promotes antioxidant activity and may improve blood vessel function. - Resveratrol:
Found in grapes and red wine, resveratrol has been shown to enhance endothelial function and reduce inflammation.
Dietary Practices
- Whole Foods Diet:
Emphasize consumption of fruits, vegetables, lean proteins, whole grains, and healthy fats to supply essential nutrients for vascular repair and maintenance. - Regular Meal Timing:
Consistent eating patterns help maintain steady blood glucose and insulin levels, reducing vascular stress. - Hydration:
Adequate water intake is crucial for maintaining blood volume and supporting optimal vascular function.
Implementing these nutritional strategies, alongside traditional medical therapies, provides a holistic approach to improving and maintaining vascular health.
Lifestyle & Preventive Tips for Vascular Health
Long-term vascular health is influenced by daily lifestyle choices. Incorporating preventive measures and healthy habits can significantly reduce the risk of developing vascular disorders and improve overall cardiovascular function.
Healthy Eating and Hydration
- Balanced Diet:
Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit processed foods, saturated fats, and excessive salt. - Regular Hydration:
Drinking adequate water supports blood volume and circulation, aiding in the prevention of high blood pressure.
Physical Activity
- Regular Exercise:
Aim for at least 150 minutes of moderate aerobic exercise per week. Activities like brisk walking, cycling, or swimming help maintain vascular elasticity and overall cardiovascular fitness. - Strength Training and Flexibility:
Incorporating resistance exercises and stretching improves muscle tone, supports weight management, and enhances vascular function.
Avoidance of Harmful Habits
- Quit Smoking:
Smoking is a major risk factor for vascular disease. Quitting smoking can significantly improve arterial function and reduce the risk of atherosclerosis. - Limit Alcohol:
Moderate alcohol consumption is advised, as excessive intake can raise blood pressure and damage blood vessels.
Stress Management
- Mindfulness Practices:
Engage in meditation, yoga, or deep breathing exercises to reduce stress, lower blood pressure, and promote a healthy vascular system. - Regular Sleep:
Ensure 7–9 hours of quality sleep per night to support overall health and allow for the recovery and repair of blood vessels.
Regular Health Monitoring
- Routine Check-Ups:
Regular visits to your healthcare provider help in early detection and management of hypertension, high cholesterol, and other risk factors. - Self-Monitoring:
Use home blood pressure monitors and mobile apps to track your health metrics and stay proactive in managing your cardiovascular risk.
By integrating these lifestyle habits, you can create a strong foundation for vascular health and reduce your risk of cardiovascular diseases.
Trusted Resources for Vascular Health
Accessing reliable and up-to-date information is essential for maintaining vascular health. The following resources provide comprehensive insights into vascular biology, disease management, and preventive strategies.
Recommended Books
- “The Cardiovascular Cure” by John P. Cooke:
A practical guide that explores lifestyle and medical interventions to improve cardiovascular health. - “The Complete Guide to Lowering High Blood Pressure Naturally” by Deborah Mitchell:
Offers evidence-based strategies for managing blood pressure and enhancing vascular health. - “Heart 411: The Only Guide to Heart Health You’ll Ever Need” by Marc Gillinov and Steven Nissen:
Provides an accessible overview of maintaining heart and vascular health.
Academic Journals
- Journal of Vascular Research:
Focuses on the latest research in vascular biology, providing insights into disease mechanisms and innovative treatments. - Arteriosclerosis, Thrombosis, and Vascular Biology:
Publishes peer-reviewed studies on vascular pathophysiology, atherosclerosis, and related cardiovascular conditions.
Mobile Applications
- MyFitnessPal:
An app that helps track diet and exercise, supporting weight management and overall vascular health. - Blood Pressure Monitor:
Enables users to log and monitor their blood pressure, which is critical for managing hypertension. - Headspace:
Offers guided meditation and mindfulness practices that contribute to stress reduction and improved cardiovascular function.
These trusted resources empower you with the latest knowledge and tools to support your vascular health journey.
Frequently Asked Questions
What are blood vessels?
Blood vessels are the network of arteries, veins, and capillaries that transport blood throughout the body, delivering oxygen and nutrients to tissues and removing waste products.
How do blood vessels regulate blood pressure?
Blood vessels regulate blood pressure through mechanisms such as vasoconstriction and vasodilation, the elasticity of arterial walls, and the baroreceptor reflex, which together adjust vascular resistance and maintain homeostasis.
What is atherosclerosis?
Atherosclerosis is a condition characterized by the buildup of plaques in arterial walls, leading to narrowed vessels, reduced blood flow, and an increased risk of heart attacks, strokes, and peripheral artery disease.
How are blood vessel disorders diagnosed?
Diagnostic methods include physical examinations, blood tests, and imaging techniques such as Doppler ultrasound, CT angiography, MR angiography, and conventional angiography to assess vessel structure and blood flow.
How can lifestyle changes improve vascular health?
A balanced diet, regular exercise, smoking cessation, stress management, and routine health monitoring can significantly improve blood vessel function, lower blood pressure, and reduce the risk of vascular diseases.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
We encourage you to share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about vascular health and empower others with valuable knowledge!




