Hereditary retinal dystrophies are a diverse group of genetic eye disorders that progressively damage the retina, leading to vision loss and sometimes blindness. These conditions, including retinitis pigmentosa, Stargardt disease, and cone-rod dystrophies, can affect people of all ages and backgrounds. Understanding the latest treatments—spanning traditional care, surgical procedures, and groundbreaking therapies—is essential for those living with, or caring for someone with, these conditions. In this comprehensive guide, we’ll explore practical solutions and cutting-edge advances that offer new hope and improved quality of life.
Table of Contents
- Understanding the Disorders and Their Impact
- Mainstream and Drug-Based Strategies
- Surgical Options and Interventional Care
- Breakthrough Innovations and Future Technologies
- Research Trials and the Path Forward
- Frequently Asked Questions
- Disclaimer
Understanding the Disorders and Their Impact
Hereditary retinal dystrophies are a family of inherited eye diseases that gradually deteriorate the retina—the delicate tissue lining the back of the eye responsible for capturing light and sending visual signals to the brain. These conditions can manifest as retinitis pigmentosa (RP), Stargardt disease, Best disease, cone-rod dystrophy, and others, each with distinct genetic causes and patterns of vision loss.
Pathophysiologically, most hereditary retinal dystrophies arise from mutations in genes vital for the structure or function of retinal cells (rods and cones). This leads to progressive cell dysfunction and death, beginning with night blindness or loss of peripheral vision, and eventually impacting central sight and color vision as the disease advances.
- Prevalence: RP, the most common subtype, affects approximately 1 in 4,000 people worldwide. Other dystrophies are rarer but collectively impact millions.
- Risk Factors: The single most important risk factor is a family history of inherited eye disease. Different inheritance patterns include autosomal dominant, autosomal recessive, X-linked, and mitochondrial.
Symptoms may appear at any age, but the majority experience gradual vision decline. Early diagnosis, tailored support, and proactive management are critical for preserving sight and independence.
Practical advice: If you notice persistent trouble seeing in low light, difficulties with peripheral vision, or have a family history of unexplained vision loss, consider a referral to an ophthalmologist specializing in inherited retinal diseases.
Mainstream and Drug-Based Strategies
There is currently no universal cure for hereditary retinal dystrophies, but established medical and rehabilitative therapies can help preserve vision, slow disease progression, and maintain quality of life. Here’s how conventional and pharmacological treatments play a role:
- Low Vision Rehabilitation: Early referral to vision rehabilitation specialists can make a profound difference. Practical aids such as magnifiers, large-print materials, audio devices, and electronic readers help maximize remaining vision.
- Vitamin and Nutritional Supplements: For some subtypes—particularly retinitis pigmentosa—vitamin A palmitate has been suggested to modestly slow progression (consult with a physician about safety and dosing). Omega-3 fatty acids and lutein may also be recommended, but evidence is variable.
- Pharmacological Approaches: There is no FDA-approved medication for most hereditary retinal dystrophies, but ongoing research explores neuroprotective agents and antioxidants to delay retinal cell degeneration.
- Management of Complications: Secondary issues like cataracts, cystoid macular edema, or refractive errors can be treated with conventional therapies such as topical carbonic anhydrase inhibitors or surgery for cataracts.
- Genetic Counseling: This is vital for all affected individuals and their families, offering insight into inheritance, family planning, and opportunities to participate in gene-specific trials.
Regular eye exams and tailored follow-up are essential to detect complications early and ensure timely intervention.
Practical advice: Adopting a healthy lifestyle—including a balanced diet rich in leafy greens, regular physical activity, and protection against excessive sunlight—may help preserve vision and overall well-being.
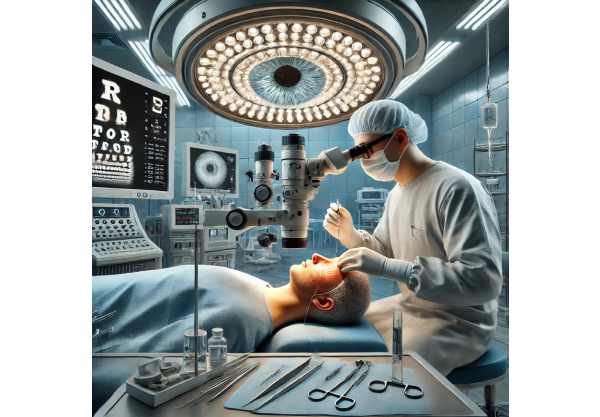
Surgical Options and Interventional Care
Though surgery cannot cure hereditary retinal dystrophies, several interventional and surgical strategies may address complications or restore partial function. Here’s a closer look:
- Cataract Extraction: Many patients develop cataracts earlier than average; modern phacoemulsification can improve visual clarity and quality of life, even if the underlying retinal disease persists.
- Intravitreal Injections: For cystoid macular edema (fluid buildup in the retina), injections of anti-VEGF agents or steroids can help reduce swelling and temporarily improve vision.
- Retinal Prostheses (Bionic Eyes): For individuals with advanced retinal degeneration and little to no remaining vision, electronic implants such as the Argus II or similar devices can restore limited visual perception by stimulating surviving retinal or optic nerve cells.
- Microincisional Vitrectomy: In rare cases of vitreous hemorrhage or retinal detachment, minimally invasive surgery is required to stabilize or save vision.
- Laser Therapies: Not a cure, but used selectively for complications like abnormal blood vessels or to seal retinal tears.
Surgical and device-based options are not universally suitable and are tailored to the individual’s specific type of dystrophy, disease stage, and remaining retinal function.
Practical advice: Engage in regular dialogue with your retina specialist to discuss eligibility for surgical or device-based interventions and to proactively manage treatable complications.
Breakthrough Innovations and Future Technologies
The last few years have ushered in remarkable progress for hereditary retinal dystrophies, including groundbreaking gene and cell therapies, next-generation implants, and advanced diagnostics.
- Gene Therapy: Luxturna (voretigene neparvovec) is approved for RPE65-related retinal dystrophy, offering hope for sight restoration. Other gene therapies targeting different genetic mutations (e.g., RPGR, ABCA4) are in clinical trials, with some demonstrating significant vision gains.
- Stem Cell Therapies: Research into replacing or repairing damaged retinal cells using stem cell–derived photoreceptors is advancing, with several early-stage trials showing safety and initial efficacy.
- Optogenetics: This innovative technique uses light-sensitive proteins introduced into remaining retinal cells to enable light perception in otherwise blind eyes—still experimental but highly promising.
- AI-Enhanced Imaging: Artificial intelligence is revolutionizing retinal imaging, enabling earlier and more precise detection of disease progression and response to treatment, allowing for more personalized care.
- Advanced Retinal Implants: Newer bionic eye systems and wireless subretinal implants are being designed to provide improved image resolution and better integration with the visual system.
These high-tech advances are rapidly moving from the lab to clinical practice, offering hope for significant improvements in vision and daily function.
Practical advice: Ask your doctor about your eligibility for gene therapy or participation in emerging technology trials—early involvement can offer access to the latest breakthroughs.
Research Trials and the Path Forward
The pace of clinical research in hereditary retinal dystrophies is accelerating, providing new opportunities for affected individuals and families. Participation in clinical trials not only opens doors to advanced treatments but also helps drive discovery and innovation for future generations.
- Active Trials: Dozens of ongoing clinical trials worldwide are focused on gene therapy, optogenetics, neuroprotective drugs, and stem cell transplants for multiple forms of hereditary retinal dystrophy.
- Pipeline Medications: Several new drug candidates—such as neurotrophic factors, RNA-based therapies, and antioxidants—are showing promise in early-stage research.
- Device Development: New bionic eye prototypes, advanced retinal prostheses, and assistive technology tools are undergoing testing, with improved functionality and accessibility as key goals.
- Patient Registries: International patient databases are critical for tracking long-term outcomes, understanding natural history, and accelerating future trial recruitment.
- Advocacy and Education: Patient organizations play a vital role in raising awareness, supporting families, and funding vital research efforts around the globe.
The future holds unprecedented hope for hereditary retinal dystrophies, thanks to collaborative global research and a growing network of clinical innovation. Patients and families are encouraged to explore clinical trial participation and to connect with support groups for guidance.
Practical advice: Stay updated on research developments by subscribing to newsletters from reputable eye health foundations or clinical trial registries.
Frequently Asked Questions
What is the most effective treatment for hereditary retinal dystrophies?
Gene therapy, specifically Luxturna for RPE65 mutations, is currently the most effective treatment for select patients. Other forms of hereditary retinal dystrophy may benefit from clinical trials, vision rehabilitation, and proactive management of complications to optimize outcomes.
Are there any new treatments for retinitis pigmentosa?
Yes, gene therapies, stem cell transplantation, and optogenetic strategies are among the newest treatments in clinical trials. These innovations aim to slow progression or restore vision in patients with advanced disease.
Can vitamin A or supplements help slow hereditary retinal dystrophy?
High-dose vitamin A palmitate may help slow retinitis pigmentosa progression for some people, but its use must be carefully monitored by a physician due to potential toxicity. Other supplements, like omega-3s, may offer supportive benefits.
Is surgery an option for hereditary retinal dystrophies?
While surgery cannot cure these conditions, procedures such as cataract extraction, vitrectomy, or the implantation of bionic eyes can improve vision or manage complications in select patients.
How can I join a clinical trial for retinal dystrophy?
Start by consulting your retina specialist and searching reputable clinical trial registries online. Eligibility depends on your genetic mutation, disease stage, and location. Many trials are actively enrolling globally.
What lifestyle changes can help manage hereditary retinal dystrophies?
Protect your eyes from UV light, maintain a nutrient-rich diet, avoid smoking, and seek regular eye exams. Early intervention, use of visual aids, and a supportive environment can help maintain independence and quality of life.
Disclaimer
This guide is for informational and educational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult your eye care professional or healthcare provider with any questions about your condition or before starting any new therapy.
If you found this article helpful, please share it with your friends and family on Facebook, X (formerly Twitter), or your preferred social platform. Your support allows us to continue producing expert, reliable health content. Follow us for more updates—your advocacy makes a difference!










