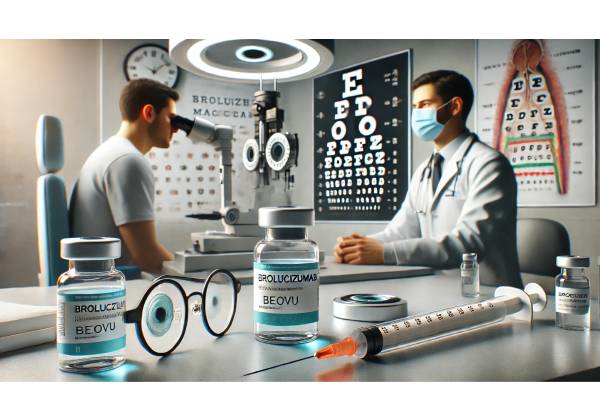
Diabetic macular edema (DME) stands as one of the leading causes of vision impairment in individuals with long-standing diabetes. Historically, patients diagnosed with DME have relied on anti-VEGF injections at frequent intervals—often monthly or bimonthly—to manage persistent retinal swelling and reduce the risk of irreversible sight loss. However, Brolucizumab (Beovu) is emerging as an innovative therapy, particularly for those seeking extended-dosing regimens that maintain or improve vision while minimizing the burden of frequent clinic visits.
Brolucizumab’s value lies not only in its potent VEGF inhibition but also in its molecular design, which enables robust retinal drying and the potential for flexible dosing intervals. This extended-dosing capability can dramatically enhance patient compliance, reduce treatment fatigue, and potentially lower overall healthcare expenses. The following sections detail the condition, how brolucizumab works, emerging clinical protocols, evidence for its safety and effectiveness, current research insights, and key pricing and accessibility considerations. By comprehensively exploring brolucizumab for DME, we hope to shed light on why this therapy is considered a major leap forward in diabetic eye care.
Decoding Diabetic Macular Edema: Understanding the Burden of Vision Loss
What Is Diabetic Macular Edema?
Diabetic macular edema (DME) is a sight-threatening complication of diabetes that stems from chronic hyperglycemia. Over time, elevated blood glucose levels can damage the delicate microvasculature of the retina, causing the small blood vessels to become leaky or occluded. The macula, responsible for central and high-resolution vision, swells in response to fluid accumulation. This swelling directly impairs one’s ability to read, drive, or perform tasks requiring precise visual acuity.
Key indicators of DME include:
- Blurriness and Distorted Vision: Patients may notice a sudden or gradual drop in visual clarity, difficulties focusing on fine details, or images appearing wavy.
- Central Scotoma: Some individuals develop dark or grayish spots in the center of their vision.
- Color Perception Changes: Although less common, certain types of DME can alter how patients perceive colors, making them seem washed out.
- Difficulty with Daily Tasks: Activities like threading a needle, reading small text, and safely maneuvering in low-light environments can become challenging.
Who Is at Risk for DME?
Duration of Diabetes: The longer a person has had type 1 or type 2 diabetes, the greater their risk of developing DME.
Poor Glycemic Control: Chronically elevated blood sugars can accelerate retinal damage.
Hypertension and Dyslipidemia: High blood pressure and elevated cholesterol can exacerbate microvascular complications in the retina.
Chronic Kidney Disease: Diabetic nephropathy often correlates with advanced retinal damage.
Genetic and Lifestyle Factors: While not fully understood, certain genetic dispositions and lifestyle habits (smoking, sedentary living) may heighten susceptibility.
Socioeconomic Impact of DME
From a public health perspective, DME transcends the individual. Loss of vision can lead to job insecurity, reduced independence, and mental health challenges such as depression or social isolation. Globally, billions of dollars are spent yearly managing complications of diabetic retinopathy and DME, with a substantial portion of that cost attributed to direct treatments, productivity losses, and rehabilitation services. Optimal management strategies that preserve sight—especially those that reduce treatment burden—can offer significant economic and quality-of-life benefits.
Limitations of Conventional Treatments
Before the advent of newer agents like brolucizumab, standard treatments for DME often encompassed:
- Laser Photocoagulation: Focal or grid laser therapy to seal leaking microaneurysms. While it can stabilize vision, laser therapy rarely improves visual acuity in advanced disease.
- Anti-VEGF Injections (e.g., Ranibizumab, Aflibercept): By blocking vascular endothelial growth factor (VEGF), these injections help reduce macular swelling. However, some require monthly or bimonthly injections for an extended period, posing challenges to patient compliance and clinic resources.
- Corticosteroid Implants: Intravitreal steroid-based implants can be effective but may increase the risk of elevated intraocular pressure (IOP) and cataract formation.
Even though these therapies significantly improved outcomes for countless patients, the drive for more flexible and longer-lasting treatment intervals has fueled research into next-generation anti-VEGF agents—particularly brolucizumab (Beovu).
Brolucizumab’s Core Strengths: Understanding the Mechanism of Action
VEGF and Its Role in DME
Vascular endothelial growth factor (VEGF) is a key signaling protein that promotes the growth and permeability of blood vessels. In diabetic retinopathy and DME, VEGF levels rise in response to ischemia (lack of adequate oxygen) in retinal tissues. This overexpression directly contributes to:
- Abnormal Vessel Growth: New but structurally fragile vessels prone to leakage.
- Blood-Retinal Barrier Breakdown: Increased permeability that allows fluid to seep into the macula, aggravating edema.
By inhibiting VEGF, anti-VEGF medications aim to limit this pathological vessel proliferation and reduce capillary leakage, restoring or maintaining macular thickness at healthier levels.
The Unique Design of Brolucizumab
Brolucizumab (brand name Beovu) distinguishes itself from earlier anti-VEGF agents through its molecular composition:
- Single-Chain Antibody Fragment (scFv): Unlike full-length monoclonal antibodies, brolucizumab is designed as a smaller molecule with high binding affinity. This smaller structure allows for greater molar dosing of the active agent with each injection.
- High Concentration Formulation: Because of its small size and targeted design, brolucizumab can be formulated at higher concentrations without compromising tolerability or injectability. This characteristic underpins its potential for an extended duration of activity in the retina.
- Robust Binding to VEGF-A Isoforms: Brolucizumab inhibits all major isoforms of VEGF-A, the primary isoform implicated in the neovascular and exudative processes underlying DME.
Pharmacokinetics and Tissue Penetration
Another notable advantage of brolucizumab is its pharmacokinetic profile. With a smaller molecular mass, it can potentially:
- Penetrate Retinal Layers More Efficiently: The drug may reach deeper retinal tissue planes, beneficial for widespread diabetic lesions.
- Facilitate Rapid Clearance from the Systemic Circulation: This may reduce the likelihood of systemic side effects sometimes associated with anti-VEGF therapies.
- Allow Higher Molar Delivery in a Smaller Injection Volume: Leading to a potentially faster onset of fluid resolution.
Clinically, these attributes translate into strong, prolonged VEGF suppression in the retina. As a result, brolucizumab often displays an extended duration of effect compared to some predecessor therapies—precisely the feature that has garnered attention for extended-dosing strategies.
Advantages Over Existing Anti-VEGF Options
- Less Frequent Injections: Due to its robust binding and sustained effect, many patients can lengthen the interval between intravitreal injections to 8, 12, or even 16 weeks after the initial loading phase.
- Potentially Superior Drying Effect: Preliminary studies suggest brolucizumab may achieve faster and more thorough reduction of fluid accumulation in the macula.
- High-Level Efficacy: Clinical trials have consistently reported visual outcomes comparable to, or in some cases surpassing, well-established anti-VEGF agents.
These characteristics make brolucizumab a compelling option for DME management, particularly in patients struggling with the rigors of frequent treatment schedules or those requiring a more potent resolution of subretinal fluid.
Extended-Dosing Protocols for Brolucizumab: Streamlining Application and Treatment
One of the most significant features of brolucizumab is the possibility for extended dosing—a major boon for both patients and clinicians. Although specific regimens can vary based on institutional protocols and patient response, a general structure has emerged in clinical practice.
Initial Loading Phase
- First Doses (Loading Period): Treatment typically begins with one intravitreal injection every 4 to 6 weeks for the first three to five doses. This period ensures maximal VEGF suppression, allowing the macula to regain more optimal thickness and function.
- Assessment of Response: At each visit, ophthalmologists measure best-corrected visual acuity (BCVA), evaluate optical coherence tomography (OCT) images to detect fluid, and assess overall ocular health. A rapid resolution of subretinal or intraretinal fluid can indicate whether the patient is likely to benefit from extended intervals.
Transition to Extended Intervals
- 8-Week Interval: After the loading phase, many patients transition to injections every 8 weeks, providing the first step toward decreasing clinic visits.
- 12-Week or Longer Interval: For those demonstrating stable disease control, no active fluid on OCT, and stable or improving visual acuity, the interval may be extended to 12 weeks or more.
- Treat-and-Extend Approach: Some clinicians adopt a “treat-and-extend” strategy, incrementally prolonging the interval between injections (e.g., from 8 weeks to 10 weeks, then to 12 weeks) until fluid reappears or vision deteriorates. At that point, the interval is shortened to maintain disease control.
Personalized Treatment Adjustments
Extended-dosing protocols are not one-size-fits-all. Factors influencing how far apart injections can be spaced include:
- Severity of DME: Patients with extensive macular thickening or multiple fluid compartments may require a slower approach to extension.
- Patient Compliance and Accessibility: Individuals living far from treatment centers or those with personal commitments that limit frequent clinic attendance often benefit most from extended dosing.
- Anatomical Response: Some patients experience fluid resolution very quickly; others require multiple loading injections before meaningful improvement occurs.
- Treatment History: Patients who have been heavily treated with other anti-VEGF medications and show partial resistance might need a more cautious extension schedule.
Combining Brolucizumab With Other Therapies
In complex or refractory DME cases, brolucizumab may be used in conjunction with:
- Focal/Pattern Laser: Especially if the edema is localized and can be partially controlled with focal laser sessions.
- Steroid Implants: Inflammatory components may coexist, and short-term steroids can tamp down inflammatory processes while brolucizumab manages the VEGF-driven aspect of the disease.
- Metabolic Control Measures: Tight glycemic control, blood pressure management, and lipid-lowering strategies remain crucial adjuncts to any DME treatment.
This multifaceted approach can be customized based on patient history, OCT findings, and the treating physician’s clinical judgment, thereby ensuring a holistic approach to DME management.
Gauging Clinical Impact: Effectiveness and Safety Profile of Brolucizumab
Robust Efficacy in Visual and Anatomical Outcomes
Multiple clinical trials and real-world studies now document brolucizumab’s efficacy for diabetic macular edema. Outcomes have shown:
- Significant Gain in Best-Corrected Visual Acuity (BCVA): Many patients experience an improvement of 5 to 10 letters on standardized visual acuity charts, translating into a meaningful enhancement in day-to-day functioning.
- Rapid Fluid Resolution: Compared to some other anti-VEGF agents, brolucizumab may achieve faster clearance of intraretinal fluid or subretinal fluid.
- Lower Treatment Burden Over Time: Patients who remain fluid-free are frequently able to move to an 8- or 12-week dosing interval, decreasing the frequency of clinic visits.
Safety and Tolerability
While anti-VEGF therapies are generally well-tolerated, each new medication must be carefully scrutinized for side effects:
- Intraocular Inflammation (IOI): Early post-marketing reports for brolucizumab suggested a slightly increased risk of IOI, including rare instances of retinal vasculitis and vascular occlusions. Rigorous pharmacovigilance efforts, updated injection guidelines, and refined screening practices have mitigated this concern. Current data indicate that with proper administration and monitoring, these events are infrequent.
- Endophthalmitis: As with any intravitreal injection, sterile technique is paramount to reduce the risk of infection.
- Systemic Adverse Effects: Similar to other anti-VEGF agents, the systemic risk of thromboembolic events (heart attack or stroke) remains low, though caution is always advised in patients with recent cardiovascular events.
- Injection-Related Discomfort: Most patients tolerate intravitreal injections well when proper anesthetic drops and antiseptic measures are employed. Mild transient discomfort or redness can occur.
Minimizing Potential Complications
To decrease the likelihood of adverse events:
- Patient Selection: Physicians weigh factors such as recent cardiovascular history, previous episodes of severe intraocular inflammation, and medication allergies.
- Sterile Technique: Adequate disinfection of the ocular surface, use of sterile eyelid speculums, and single-use instruments can prevent infections.
- Close Monitoring: A follow-up visit within 1–2 weeks after the injection can catch and address early signs of inflammation or other complications.
- Patient Education: Empowering patients with knowledge of warning signs (e.g., sudden vision changes, eye pain, redness) fosters prompt reporting and timely intervention if issues arise.
In sum, while brolucizumab carries potential risks akin to other intravitreal therapies, adherence to recommended protocols has enabled the majority of patients to benefit from its robust efficacy with minimal complications.
Latest Research Findings: Clinical Trials and Real-World Data on Brolucizumab
Clinical Trials Shaping DME Treatment
- KESTREL and KITE Studies:
These pivotal phase III trials evaluated brolucizumab in DME patients. Over 1,500 participants were randomized to receive either brolucizumab or a comparative anti-VEGF. Key findings included:
- Improved BCVA Gains: Brolucizumab-treated patients achieved non-inferior or, in some assessments, even superior visual acuity gains compared to control groups.
- Robust Drying Effect: OCT scans showed meaningful reductions in central subfield thickness (CST), highlighting brolucizumab’s efficacy in resolving fluid buildup.
- Extended Dosing Success: A notable proportion of patients on brolucizumab maintained fluid-free maculas on 12-week dosing intervals following loading.
- Real-World Observational Cohorts:
Post-approval, multiple ophthalmic centers have published observational data. In these real-world settings—where patients often exhibit coexisting pathologies and variable compliance—brolucizumab maintained consistent and promising outcomes. Some reported that the drug successfully salvaged vision in patients who had plateaued on other anti-VEGFs, pointing to brolucizumab’s capacity to manage refractory DME. - Longitudinal Safety Assessments:
Several post-marketing registries and safety databases continue to track rates of intraocular inflammation, vasculitis, and other adverse effects. The consensus so far remains that while vigilance is necessary, the incidence of severe complications remains low, and the benefit-risk profile favors ongoing use in appropriate candidates.
Potential Indications and Future Directions
Brolucizumab’s mechanism—potent VEGF-A inhibition with small-molecule technology—opens the door for broader applications beyond DME. Notably, neovascular age-related macular degeneration (nAMD) and other macular pathologies have already seen brolucizumab introduced to clinical practice. Ongoing investigations aim to determine whether:
- Longer Than 12-Week Intervals are feasible for select patients, further reducing the injection burden.
- Combination Therapies (e.g., pairing brolucizumab with new anti-fibrotic or anti-inflammatory agents) could offer synergy in advanced or poorly controlled diabetes-related retinal diseases.
- Personalized Monitoring (via home-based OCT devices or wearable technologies) might refine treat-and-extend algorithms, enabling truly individualized injection schedules.
Given these evolving possibilities, it’s no surprise that many retina specialists consider brolucizumab a cornerstone of next-generation DME therapy.
Navigating the Financial Landscape: Pricing and Accessibility of Brolucizumab
Typical Cost Considerations
In most healthcare markets, brolucizumab pricing reflects its status as a specialized biologic therapy. Several factors influence the cost:
- Geographical Region: Prices can vary substantially between countries and even within the same country, depending on local regulations, reimbursement policies, and negotiated agreements with manufacturers.
- Healthcare System: In single-payer systems, bulk procurement or government-subsidized programs may bring prices down, while in private insurance models, coverage often hinges on formulary inclusion.
- Dose and Treatment Frequency: Although each brolucizumab vial contains a standard 6 mg dose, the total annual expense may be reduced if patients can extend their injection intervals to 12 weeks or beyond.
In some regions, an intravitreal injection of brolucizumab may cost around USD 1,000 to USD 2,000 per vial when factoring in wholesale acquisition costs or negotiated rates. Clinical administration fees, facility charges, and related expenses can add to this base price. Thus, a patient receiving 8–10 injections a year might expect total drug-related costs to range between USD 8,000 and USD 20,000 annually. These figures are approximate and vary greatly depending on insurance coverage and specific clinical protocols.
Insurance Coverage and Reimbursement
- Commercial Insurance: Many private insurers require documentation of medical necessity, including evidence that a patient’s DME is insufficiently controlled with other treatments. They may also mandate step therapy protocols, where brolucizumab is covered only after less costly anti-VEGF agents are tried.
- Medicare and Government Programs: Older or disabled individuals may benefit from coverage under national healthcare programs. However, the extent of coverage depends on local guidelines and whether brolucizumab is included in standard formularies.
- Prior Authorization Process: Clinicians typically submit prior authorization requests that detail the severity of the patient’s DME, previous treatment history, and the rationale for choosing brolucizumab, especially if extended dosing is anticipated.
Pathways for Access and Affordability
- Manufacturer Assistance Programs: Pharmaceutical companies often provide co-pay cards or direct financial aid to eligible patients. These programs can significantly lower out-of-pocket costs, especially for individuals who lack robust insurance coverage.
- Institutional Discount Schemes: Certain clinics or health systems negotiate volume-based discounts, passing some savings on to patients.
- Nonprofit and Charitable Organizations: Diabetes-related charities and vision-oriented nonprofits sometimes partner with pharmaceutical companies to cover partial treatment costs for uninsured or underinsured individuals.
- Clinical Trials: Patients who meet eligibility criteria may access the medication at reduced or no cost by participating in research studies, although such trials require strict adherence to protocols and frequent follow-up visits.
Balancing Cost with Clinical Benefits
For many patients, brolucizumab’s extended-dosing potential and high efficacy may translate into fewer injections per year, thus offsetting the per-injection cost. Fewer visits reduce transportation expenses, missed workdays, and logistical burdens—an especially important consideration for older or mobility-challenged individuals. When factoring in these indirect savings, brolucizumab may prove cost-effective for select patient populations, particularly those with poor tolerance to frequent injections or those requiring potent resolution of edema that has been unresponsive to other agents.
Disclaimer
This article is intended for educational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider regarding any questions about a medical condition, treatment options, or before starting a new healthcare regimen.