Introduction to Chalcosis
Chalcosis is a rare ocular condition caused by the deposit of copper or copper-containing foreign bodies in the eye. This condition typically develops after an ocular injury, in which copper or a copper alloy becomes embedded in the ocular tissues. The presence of copper in the eye can cause a series of inflammatory responses and tissue damage, which, if not treated, can result in severe visual impairment or blindness. Chalcosis is distinguished from another similar condition known as siderosis, which causes iron deposits in the eye. Understanding chalcosis is critical for early detection and effective treatment, particularly in patients who have had ocular trauma involving copper or brass.
Chalcosis: Detailed Examination of Condition
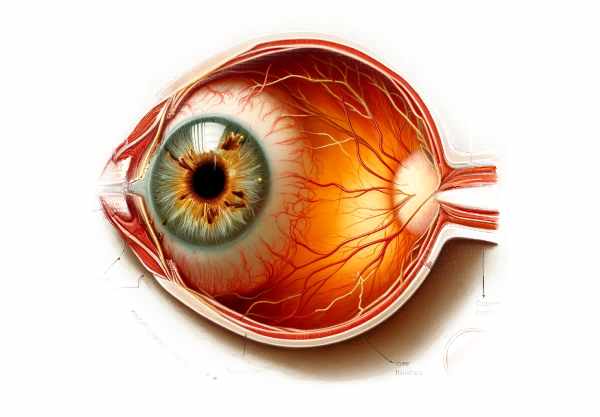
Chalcosis is caused by the toxic effects of copper when it enters the eye, typically through penetrating trauma with copper-containing objects. This condition can affect different parts of the eye, causing a variety of symptoms and complications depending on the amount of copper deposited and the length of exposure.
Pathophysiology
Copper is an essential trace element in the body that participates in a variety of enzymatic processes. However, when copper accumulates in the eye, it can become toxic. Copper’s toxicity arises from its ability to catalyze the formation of free radicals, which causes oxidative stress and cellular damage. The damage primarily affects the anterior segment of the eye, including the cornea, lens, and anterior chamber.
Corneal Involvement
One of the distinguishing features of chalcosis is the presence of a greenish or brownish discoloration of the cornea known as the “chalcosis ring.” This ring is formed as a result of copper deposition in the corneal stroma and Descemet membrane. A slit-lamp examination can reveal the ring, which is frequently used to diagnose chalcosis.
Lens Changes
Copper deposition can also cause changes in the lens, resulting in a distinct appearance known as “sunflower cataract” or “sunflower lens.” This condition is distinguished by a central disc of opacity and radiating petal-like spokes. Copper ions deposit in the anterior lens capsule and cortex, resulting in these distinct opacities. Sunflower cataracts can significantly impair vision if they progress and require surgical intervention.
Anterior Chamber and Iris
Copper in the anterior chamber can cause inflammation, a condition known as anterior uveitis. The iris may also show signs of copper deposition, which can result in heterochromia (different-colored eyes) or copper deposits on the iris surface. Persistent inflammation can lead to complications like glaucoma, which occurs when increased intraocular pressure damages the optic nerve, potentially resulting in vision loss.
Retina and Choroidal Involvement
Copper, while less common, can affect the eye’s posterior segment. Retinal toxicity can cause pigmentary changes, retinal detachment, and retinal hemorrhages. The choroid, a vascular layer of the eye, can show signs of copper deposition, resulting in choroiditis and vision problems.
Clinical Presentation
The clinical presentation of chalcosis varies according to the amount of copper exposure and the time since the initial injury. Patients can present with a variety of symptoms, including:
Symptoms may include decreased visual acuity, eye pain or discomfort, redness and inflammation, photophobia (light sensitivity), floaters or flashes of light, and iris color changes.
The severity of symptoms is related to the amount of copper deposited and the resulting inflammatory response. In some cases, the initial ocular trauma may be minor, and the symptoms of chalcosis may appear gradually over time, making early diagnosis difficult.
Risk Factors
Several risk factors can predispose people to chalcosis. The primary risk factor is a history of ocular trauma from copper-containing objects. Metalworking, welding, and construction are all significant risk factors for eye injuries. Furthermore, people with underlying conditions that impair ocular integrity, such as corneal dystrophies or previous eye surgeries, may be more likely to develop chalcosis after being exposed to copper.
Complications
If not diagnosed and treated promptly, chalcosis can cause a number of serious complications. The complications include:
- Glaucoma: Persistent inflammation and copper deposition can raise intraocular pressure, causing optic nerve damage.
- Cataracts: Sunflower cataracts can progress, resulting in significant visual impairment that may necessitate surgical intervention.
- Corneal Scarring: Chronic corneal inflammation and copper deposition can cause corneal opacities and scarring, compromising vision.
- Retinal Damage: Copper toxicity can cause retinal pigmentary changes, detachment, and hemorrhages, potentially resulting in permanent vision loss.
Pathologic Findings
A histopathological examination of chalcosis-affected ocular tissues reveals copper deposits in the cornea, lens, and other ocular structures. These deposits appear as reddish-brown granules, which are frequently associated with inflammatory cell infiltration. The extent of tissue damage varies with the duration and severity of copper exposure.
Differences From Siderosis
Chalcosis should not be confused with siderosis, another ocular condition caused by iron deposition. While both conditions have similarities, such as the presence of metallic foreign bodies and the potential for significant ocular damage, their presentation and pathological findings differ significantly. Siderosis is characterized by rust-colored deposits and a different pattern of intraocular involvement than chalcosis, which has greenish or brownish deposits.
Prognosis
The prognosis for chalcosis is dependent on prompt diagnosis and treatment. Early detection and removal of the copper-containing foreign body can prevent additional copper deposition and reduce the inflammatory response. However, if untreated, chalcosis can cause irreversible damage and permanent vision loss. Patients with a history of copper-related ocular trauma require regular follow-up and monitoring to ensure early intervention if symptoms of chalcosis develop.
Preventing Chalcosis: Key Measures
- Use Protective Eyewear: Always wear appropriate protective eyewear when engaging in activities that could cause eye injury, such as metalworking, welding, or construction.
- Maintain Workplace Safety: To avoid accidental eye injuries, ensure that safety protocols are followed in workplaces with metalwork and copper-containing materials.
- Seek Immediate Medical Attention: If you sustain an eye injury, get medical help right away, especially if it involves metallic foreign bodies. Early intervention can help prevent complications.
- Routine Eye Examinations: Regular eye exams, particularly for those in high-risk occupations, can help detect early signs of ocular conditions such as chalcosis.
- Educate on Eye Injury Risks: Increase workers’ and individuals’ awareness of the risks associated with ocular trauma and the importance of protective measures in high-risk activities.
- Proper Metal Handling: Use caution when handling copper-containing objects and other metals, and store and use them safely to reduce the risk of accidents.
- Follow-Up Care: If you have had a copper-related eye injury, schedule follow-up appointments and monitor for any delayed onset of chalcosis.
- First Aid Training: Provide workplaces and individuals with first aid knowledge and resources so that eye injuries can be effectively managed before professional medical help arrives.
Diagnostic methods
Chalcosis is diagnosed using a combination of the patient’s history, clinical examination, and advanced imaging techniques. A thorough patient history is essential, especially for any instances of ocular trauma or exposure to copper-containing materials. This history can provide important clues for the diagnostic process.
Clinical Examination
The initial clinical examination includes a thorough ophthalmic evaluation with slit-lamp biomicroscopy. This allows for the identification of distinguishing features such as corneal discoloration, sunflower cataracts, and copper deposits in the vitreous body. Gonioscopy can be used to assess the anterior chamber angle and identify any copper deposits or inflammatory changes.
Advanced Imaging Techniques.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and vitreous. It is useful for detecting retinal changes and determining the amount of copper deposited in the ocular tissues.
- Fundus Photography: This technique produces detailed images of the retina, highlighting pigmentary changes and the presence of copper deposits. It is especially useful for documenting disease progression and assessing treatment outcomes.
- Ultrasound Biomicroscopy (UBM): UBM can produce detailed images of the anterior segment of the eye, such as the cornea, lens, and ciliary body. It is useful for determining the effects of copper deposition on these structures.
Electroretinography (ERG)
ERG measures the retina’s electrical responses to light stimulation. In cases of chalcosis, ERG can aid in evaluating retinal function and detecting early signs of retinal toxicity before significant structural changes emerge.
Lab Tests
While not always necessary, laboratory tests such as serum copper levels can be considered when systemic copper toxicity is suspected. However, ocular manifestations are usually independent of systemic copper levels.
Chalcosis: Effective Treatment Strategies
The primary goal of treating chalcosis is to remove the copper-containing foreign body and manage the resulting ocular damage. Treatment strategies include:
- Surgical Removal: The definitive treatment for chalcosis is surgical removal of the intraocular foreign body. Depending on where the foreign body is located, techniques like vitrectomy or anterior segment surgery may be used. Prompt removal is critical to avoiding additional copper toxicity and minimizing ocular damage.
- Anti-inflammatory Medications: Corticosteroids and non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat inflammation caused by chalcosis. These medications can be given topically, orally, or intraocularly, depending on the severity of the inflammation.
- Antioxidants: Antioxidant therapy is intended to reduce oxidative stress caused by copper deposition. Vitamin E and other antioxidants can be used to neutralize free radicals and protect the ocular tissues from further damage.
- Management of Secondary Conditions: Secondary conditions like cataracts, glaucoma, and retinal detachment necessitate specialized treatments. Sunflower cataracts may require cataract surgery, whereas glaucoma can be treated with medications or surgical procedures that lower intraocular pressure. Retinal detachment may necessitate surgical repair to reattach the retina and restore visual function.
Innovative and Emerging Therapies 1. Chelation Therapy Chelation therapy, which uses agents such as D-penicillamine to bind and remove copper ions from ocular tissues, is being studied experimentally. Although promising, these therapies are still in the experimental stage and require additional research to determine their safety and efficacy.
- Gene Therapy: Advances in gene therapy show promise for treating chalcosis at the molecular level. Researchers are working to develop gene-editing techniques that can target and modify the genes responsible for copper metabolism, potentially preventing copper accumulation in ocular tissues.
- Nanotechnology: The use of nanoparticles for targeted drug delivery is a growing field. Nanoparticles can be designed to deliver anti-inflammatory and antioxidant agents directly to affected ocular tissues, increasing therapeutic efficacy while reducing systemic side effects.
Trusted Resources
Books
- “Ophthalmology” by Myron Yanoff and Jay S. Duker
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn and Dante J. Pieramici






