Introduction to Eales Disease
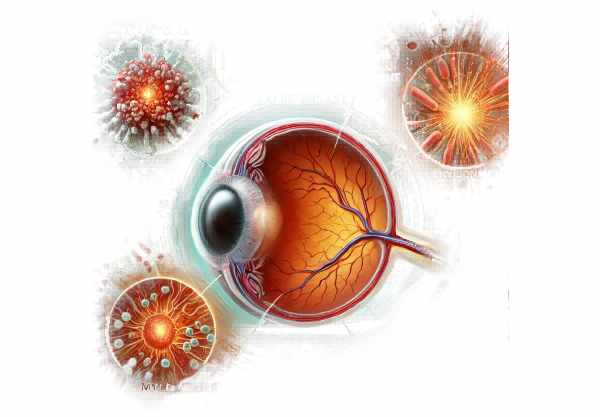
Eales disease is a rare idiopathic occlusive vasculopathy that primarily affects the peripheral retina and is most frequently seen in young adults. Eales disease, named after British ophthalmologist Henry Eales, who first described it in 1880, is characterized by retinal vein inflammation, occlusion, and subsequent neovascularization. This can result in recurring vitreous hemorrhages and, in severe cases, retinal detachment. The exact cause is unknown, but it is thought to have an immunological component, possibly triggered by a hypersensitivity reaction to tuberculosis protein. Eales disease typically manifests unilaterally, but it can progress to bilaterality, causing significant vision loss if not properly managed.
Eales’ Disease Insights
Etiology and Pathophysiology
The exact cause of Eales disease is unknown, but it is suspected to be multifactorial, involving both genetic and environmental factors. The strong association with tuberculosis suggests an immune response to Mycobacterium tuberculosis antigens. This hypersensitivity reaction may result in an inflammatory cascade affecting the retinal veins.
Stages of Eales Disease
Eales disease develops in three distinct stages:
- Inflammatory Stage: Perivasculitis, or inflammation and thickening of the retinal veins, characterizes this initial stage. Patients may experience floaters and mild visual disturbances.
- Occlusive Stage: As the disease advances, inflammation causes venous occlusion, which can result in retinal ischemia. During this stage, patients may experience more severe visual symptoms as a result of retinal ischemia.
- Proliferative Stage: In response to ischemia, new abnormal blood vessels develop (neovascularization). These fragile vessels are prone to bleeding, which can cause recurrent vitreous hemorrhages and, if left untreated, tractional retinal detachment.
Symptoms
The symptoms of Eales disease vary depending on the stage and severity of the condition. Common symptoms include:
- Floaters: Small spots or threads that float across the field of vision, usually caused by vitreous hemorrhage.
- Blurry Vision: This can be caused by macular edema or vitreous hemorrhage, which obscures the visual axis.
- Sudden Vision Loss: A significant vitreous hemorrhage or retinal detachment can result in sudden, severe vision loss.
- Photopsia: Light flashes in the peripheral vision, usually caused by retinal traction or detachment.
- Scotomas: Dark spots or areas of lost vision in the visual field, usually caused by retinal ischemia or hemorrhage.
Risk Factors
Several risk factors have been linked with Eales disease, including:
- Tuberculosis Exposure: A history of tuberculosis or a positive tuberculin skin test may indicate a link to Eales disease.
- Young Age: Eales disease primarily affects people between the ages of 20 and 40.
- Male Gender: Males are more likely than females to develop Eales disease.
- Geographical Predisposition: The condition is more common in countries with a high tuberculosis prevalence, such as India and other parts of Asia.
Complications
If not treated properly, Eales disease can cause a number of serious complications:
- Vitreous Hemorrhage: Recurrent bleeding into the vitreous can cause severe vision loss and may necessitate surgical intervention.
- Retinal Detachment: Neovascularization and fibrovascular proliferation can cause tractional retinal detachment, resulting in severe vision loss.
- Neovascular Glaucoma: The formation of new, abnormal blood vessels in the iris and angle can cause elevated intraocular pressure and glaucoma.
- Cataract Formation: Chronic inflammation and multiple intraocular surgeries can raise the risk of cataract development.
Differential Diagnosis
Several other conditions can present with symptoms similar to Eales disease, so differential diagnosis is essential. These conditions include the following:
- Diabetic Retinopathy: Similar to Eales disease, diabetic retinopathy can cause retinal neovascularization and vitreous hemorrhage, but it is usually associated with a history of diabetes.
- Retinal Vein Occlusion: While this condition can cause similar retinal changes, it is typically associated with systemic vascular diseases such as hypertension and atherosclerosis.
- Sarcoidosis is an inflammatory disease that can affect multiple organs, including the eyes, resulting in granulomatous uveitis and retinal vasculitis.
- Behçet’s Disease is an autoimmune condition that can result in recurrent oral and genital ulcers, uveitis, and retinal vasculitis.
- Sickle Cell Retinopathy: This condition is common in sickle cell disease patients and can cause retinal ischemia and neovascularization.
Pathologic Findings
A histopathological examination of eyes with Eales disease reveals:
- Perivasculitis is inflammation around the retinal veins.
- Venous Occlusion: The blockage of retinal veins caused by inflammatory processes.
- Neovascularization is the formation of new blood vessels in response to ischemia.
- Fibrovascular Proliferation: The expansion of fibrous tissue and blood vessels, causing traction on the retina.
Effects on Quality of Life
Because of its recurrence and the risk of severe visual impairment, Eales disease can have a significant impact on quality of life. Frequent medical visits, potential surgical interventions, and the stress of managing a chronic eye condition can all have an impact on one’s mental health and daily life. Early detection and appropriate treatment are critical in preserving vision and reducing complications.
Prevention Tips
- Regular Eye Examinations: People, particularly those in high-risk groups, should have regular eye exams to detect early signs of Eales disease and other retinal conditions. Early detection can help prevent complications and preserve vision.
- Tuberculosis Screening: Given the link between Eales disease and tuberculosis, screening for tuberculosis is critical in high-risk populations. Early detection and treatment of tuberculosis may reduce the risk of developing Eales disease.
- Healthy Lifestyle: Adopting a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking can improve overall health and potentially lower the risk of inflammatory conditions affecting the eyes.
- Prompt Treatment of Infections: Treating systemic infections as soon as possible and effectively can help prevent complications that may trigger inflammatory responses, including those affecting the eyes.
- Manage Chronic Conditions: Proper management of chronic conditions such as diabetes and hypertension is critical because they can worsen retinal vascular issues, potentially complicating Eales disease.
- Protective Eyewear: Wearing protective eyewear during activities that may result in eye injury can help prevent trauma-induced inflammatory responses in the retina.
- Stay Informed: Learning about the symptoms and risk factors for Eales disease can lead to earlier detection and treatment. Awareness is critical for managing and preventing potential complications.
- Seek Medical Advice for Visual Symptoms: Any sudden changes in vision, such as floaters, flashes of light, or loss of vision, should result in an immediate medical evaluation to rule out serious conditions, including Eales disease.
- Adhere to Treatment Plans: Individuals diagnosed with Eales disease or related conditions must follow prescribed treatment plans and attend follow-up appointments to monitor disease progression and avoid complications.
- Avoidance of Tuberculosis Exposure: In areas with a high prevalence, taking precautions to avoid tuberculosis, such as vaccination and avoiding high-risk environments, can be beneficial.
Diagnostic methods
A comprehensive approach is required to diagnose Eales disease, which includes clinical evaluation, imaging studies, and laboratory tests. The goal is to confirm the presence of retinal vasculitis and neovascularization while excluding other conditions with similar symptoms.
- Ophthalmic Examination: The first step is an ophthalmologist’s thorough examination of the eyes. This includes:
- Visual Acuity Test: To determine the clarity of vision.
- Slit-Lamp Examination: Examine the anterior segment of the eye for signs of inflammation.
- Fundus Examination: Using an ophthalmoscope, examine the retina for signs of perivasculitis, retinal hemorrhages, or neovascularization.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and photographing the dye as it travels through the retinal blood vessels. It aids in the detection of leakage, occlusion, and neovascularization in the retina, confirming the diagnosis of Eales disease.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina. It aids in detecting macular edema, vitreous hemorrhage, and other structural changes associated with Eales disease.
- Ultrasound B-Scan: When vitreous hemorrhage obscures the view of the retina, an ultrasound B-scan can aid in visualizing the posterior segment and detecting retinal detachment or other complications.
Innovative Diagnostic Techniques
- OCT Angiography (OCTA): OCTA is a non-invasive imaging technique for obtaining detailed images of the retinal and choroidal vasculature. It can detect microvascular changes, neovascularization, and areas of ischemia without the use of dye injections, making it safer and more convenient for patients.
- Indocyanine Green Angiography (ICGA): Similar to fluorescein angiography, ICGA employs indocyanine green dye. It improves visualization of the choroidal vasculature, which can be useful in complicated cases of Eales disease with choroidal involvement.
- Electroretinography (ERG): ERG detects the electrical responses of different cell types in the retina, such as photoreceptors and ganglion cells. It aids in the assessment of retinal function and the detection of dysfunction caused by ischemia or inflammation.
Lab Tests
- Tuberculosis Screening: Given the link between Eales disease and tuberculosis, tuberculosis screening is critical. Tests include:
- Tuberculin Skin Test (TST): To detect a Mycobacterium tuberculosis infection, whether past or present.
- Interferon-Gamma Release Assays (IGRAs) are blood tests that assess the immune response to tuberculosis antigens.
- Blood Tests: General blood tests, such as the complete blood count (CBC) and inflammatory markers (e.g., ESR, CRP), can help determine the patient’s overall inflammatory status.
Comprehensive Evaluation
Combining these diagnostic methods enables a thorough evaluation of Eales disease. This comprehensive approach aids in confirming the diagnosis, determining the severity of the disease, and developing appropriate treatment strategies.
Effective Treatment for Eales Disease
The treatment of Eales disease focuses on inflammation control, preventing complications, and preserving vision. A combination of medical and surgical procedures is frequently required.
Standard Treatment Options
- Corticosteroids: Oral or periocular corticosteroids are frequently used to reduce inflammation. They help to control perivasculitis and prevent further retinal damage. Topical steroids may also be used to treat anterior segment inflammation.
- Anti-Tubercular Therapy (ATT): In cases where tuberculosis is confirmed or suspected, a complete course of anti-tubercular therapy is required. This aids in addressing the underlying cause and reducing the occurrence of inflammation.
- Anti-VEGF Injections: Treatment for neovascularization and macular edema involves intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) agents such as bevacizumab or ranibizumab. These injections help to lower the risk of vitreous hemorrhage and improve visual outcomes.
- Laser Photocoagulation: Laser-based pan-retinal photocoagulation (PRP) is an effective treatment for retinal neovascularization. It lowers the risk of vitreous hemorrhage and retinal detachment by coagulating abnormal blood vessels and preventing their growth.
Surgical Treatment Alternatives
- Vitrectomy: A pars plana vitrectomy is used to treat recurring or persistent vitreous hemorrhage. This surgery involves removing the vitreous gel and any blood that may be present, allowing for better retina visualization and treatment.
- Scleral Buckling: Retinal detachment is treated with scleral buckling surgery to reattach the retina. This involves wrapping a silicone band around the eye to support the retina and reduce traction from the vitreous.
- Retinal Cryotherapy: Cryotherapy can help treat peripheral retinal neovascularization. This method uses extreme cold to destroy abnormal blood vessels and reduce inflammation.
Innovative and Emerging Therapies
- Biologic Agents: Research is being conducted into the use of biologic agents that target specific inflammatory pathways. These agents, such as TNF-alpha inhibitors, may provide new ways to manage inflammation in Eales disease.
- Gene Therapy: Although still in the experimental stage, gene therapy has the potential to treat retinal diseases by delivering genetic material to correct or modify the underlying causes.
- Stem Cell Therapy: Stem cell therapy is used to regenerate damaged retinal tissue and restore function. This emerging field has the potential to transform the treatment of retinal diseases such as Eales disease.
Supportive Measures
- Regular Monitoring: Patients with Eales disease should have regular follow-up appointments to monitor disease progression and adjust treatment plans as needed.
- Visual Rehabilitation: Visual rehabilitation, as well as the use of low-vision aids, can help patients with significant vision loss improve their quality of life and independence.
- Lifestyle Modifications: Promoting a healthy lifestyle, such as a balanced diet, regular exercise, and quitting smoking, can improve overall eye health and reduce inflammation.
Trusted Resources
Books
- “Retinal Vascular Disease” by A.M. Joussen, T.W. Gardner, B. Kirchhof, S. Ryan
- “Retina” by Stephen J. Ryan, Andrew P. Schachat, Charles P. Wilkinson
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski










