What are orbital fractures?
Orbital fractures are breaks or cracks in the bones surrounding the eye, known as the orbit. These fractures are most commonly caused by facial trauma, such as accidents, falls, sports injuries, or physical assaults. Orbital fractures can range from minor cracks to more complicated breaks involving multiple bones. They frequently cause pain, swelling, bruising, and, in severe cases, visual impairment. Understanding orbital fractures is critical for early diagnosis and treatment to avoid long-term complications.
The Complexities of Orbital Fractures
The specific bones involved and the complexity of the injury determine the classification of orbital fractures. The orbit is made up of several bones: the frontal bone (forming the superior rim), the zygomatic bone (forming the lateral wall), the maxillary bone (forming the inferior wall), the ethmoid bone (forming the medial wall), and the sphenoid bone (forming the posterior wall). Fractures can occur in any of these bones, resulting in a variety of clinical outcomes.
Types of Orbital Fractures
- Orbital Rim Fractures: These fractures affect the bony outer edges of the eye socket. They are typically the result of direct blunt trauma and can be associated with facial fractures.
- Blowout Fractures: These happen when a sudden impact to the eye raises intraorbital pressure, causing the thin bones of the orbital floor or medial wall to fracture. This type of fracture frequently results in herniation of orbital contents, such as fat or muscle, into nearby sinuses.
- Trapdoor Fractures: These are the most common type of blowout fractures in children. The bone fragment acts as a trapdoor, snapping shut after impact and trapping soft tissues, resulting in severe symptoms.
- Orbital Roof Fractures: These involve the upper part of the orbit and are uncommon, usually caused by high-impact trauma. Because of their proximity to the brain, they have the potential to cause intracranial injuries.
- Complex Orbital Fractures: These fractures, which involve multiple orbital bones, are common in severe trauma cases such as car accidents or significant falls.
Causes and Risk Factors
Orbital fractures are most commonly caused by blunt force trauma to the face. Common causes include:
- Automobile Accidents: High-speed collisions frequently cause serious facial trauma, including orbital fractures.
- Sports Injuries: Contact sports like boxing, football, and soccer increase the risk of orbital fractures due to impacts from balls, elbows, or collisions with other players.
- Falls: Accidental falls, especially in older adults, can cause fractures of the orbital bones.
- Physical Assaults: Blows to the face during altercations can result in orbital fractures.
- Industrial Accidents: Work-related injuries involving heavy machinery or falls from heights can cause facial and orbital fractures.
Symptoms
The symptoms of orbital fractures differ according to the type and severity of the fracture. Common symptoms include:
- Pain and swelling: Around the affected eye, frequently accompanied by bruising.
- Double Vision (Diplopia): Caused by eye misalignment due to muscle entrapment or orbital bone displacement.
- Restricted Eye Movement: Caused by muscle entrapment or swelling.
- Enophthalmos: A sunken appearance of the eye, usually associated with blowout fractures.
- Proptosis: Eye protrusion, typically associated with severe fractures or hematomas.
- Numbness in the cheek, upper lip, or gums, indicating an infraorbital nerve injury.
- Visible Deformity: Examples include a step-off deformity on the orbital rim.
Pathophysiology
The pathophysiology of orbital fractures involves the transmission of force to the orbital bones, which results in a break in the continuity of the bony structures. The mechanism of injury differs according to the type of fracture:
- Direct Impact: Blunt force to the orbital rim can fracture the thicker bones that make up the rim.
- Increased Intraorbital Pressure: A blow to the eye can raise the pressure within the orbit, causing the thin bones of the orbital floor or medial wall to give way, resulting in blowout fractures.
- Elastic Recoil: The elastic nature of children’s bones can result in trapdoor fractures, in which a bone fragment snaps back and traps soft tissues.
Complications
Orbital fractures can cause a variety of complications if not treated promptly and properly:
- Orbital Hematoma: The accumulation of blood within the orbit can raise intraorbital pressure and impair vision.
- Muscle Entrapment: Muscles may become trapped in the fracture, resulting in limited eye movement and persistent double vision.
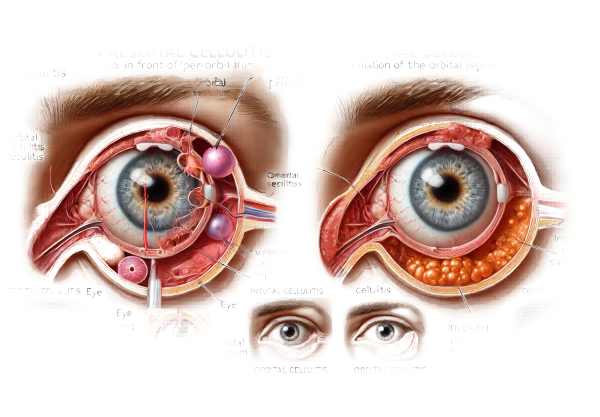
- Infection: Open fractures or those involving the sinuses may result in orbital cellulitis or abscess formation.
- Vision Loss: Direct optic nerve injury or secondary effects from increased intraorbital pressure can cause permanent vision loss.
- Cosmetic Deformities: Misalignment of the orbital bones can cause visible facial asymmetry and a sunken eye appearance.
Differential Diagnosis
To accurately diagnose orbital fractures, it is necessary to distinguish them from other conditions that may present with similar symptoms.
- Orbital Cellulitis: An infection of the orbital tissues can cause pain, swelling, and restricted eye movement, but it usually starts with a fever and systemic symptoms.
- Sinusitis: Sinusitis can cause pain and swelling around the eyes, but it does not have the trauma history of a fracture.
- Orbital Tumors: Tumors can cause proptosis and vision changes, but they typically develop gradually and do not have an acute trauma history.
- Traumatic Optic Neuropathy: Direct injury to the optic nerve can result in vision loss after trauma, but without the bony involvement seen in fracture.
Epidemiology
Orbital fractures are fairly common, particularly in cases involving facial trauma. They are more common in men, often because they participate in more activities that put their faces at risk. Sports and high-energy activities pose a particular risk to young adults and adolescents. Orbital fractures are also more common in urban areas due to higher rates of car accidents and assaults.
Understanding the specifics of orbital fractures, such as their types, causes, symptoms, and potential complications, is critical for healthcare providers to accurately diagnose and manage this condition.
Methods for Diagnosing Orbital Fractures
Diagnosing orbital fractures necessitates a multifaceted approach that combines clinical evaluation with advanced imaging techniques and, in some cases, additional tests to confirm the extent and severity of the injury.
Clinical Evaluation
The first step in diagnosing orbital fractures is a thorough clinical evaluation that includes:
- Patient History: A detailed account of the trauma event, including the mechanism of injury, the force involved, and any prior facial injuries.
- Physical Examination: A thorough examination of the eye and surrounding structures for signs of fracture, such as bruising, swelling, deformity, and limited eye movements. The evaluation of visual acuity, pupillary responses, and ocular motility is critical.
- Palpation: Checking for bony irregularities, tenderness, and step-off deformities on the orbital rim and other facial bones.
Imaging Studies
Imaging is critical in confirming the diagnosis of orbital fractures and determining their extent and complexity:
- CT Scan (Computed Tomography) is the gold standard for diagnosing orbital fractures. A CT scan provides detailed cross-sectional images of the orbital bones, allowing for accurate fracture location and assessment. It detects bone displacement, muscle entrapment, and associated soft tissue injuries. Coronal and axial views are especially useful for examining the orbital floor and medial wall.
- MRI (Magnetic Resonance Imaging): While not typically used for initial diagnosis, MRI can be useful in assessing soft tissue injuries, optic nerve damage, and intracranial complications. It offers better contrast resolution for soft tissues than CT.
- X-rays: While less detailed than CT scans, plain radiographs can occasionally be used as a preliminary assessment tool, particularly in situations where CT is not immediately available. Waters’ view and Caldwell view are common projections for visualizing the orbit.
Additional Diagnostic Tools
- Ultrasound: Ocular ultrasound can be used to evaluate the globe and intraorbital structures, especially when a foreign body is suspected or a thorough examination of soft tissues is required.
- Ophthalmic Examination: An ophthalmologist’s comprehensive eye examination may include a slit-lamp examination, a dilated fundus examination, and intraocular pressure measurement to detect globe injuries or retinal damage.
- Forced Duction Test: This test determines whether restricted eye movement is the result of mechanical entrapment or neurological causes. It entails manually moving the eye to test for resistance.
- Hess Charting: This diagnostic tool can help assess and document the severity of ocular motility restrictions caused by muscle entrapment or nerve damage.
Orbital Fracture Treatment
The severity and type of orbital fracture, as well as the presence of any complications such as muscle entrapment, vision impairment, or cosmetic deformities, all influence treatment decisions. The treatment options range from conservative management to surgical intervention.
Conservative Management
- Observation: Minor, non-displaced fractures with no evidence of muscle entrapment, significant deformity, or vision impairment can be treated conservatively with close observation. Patients are usually monitored for changes in symptoms or complications.
- Cold Compresses and Pain Management: Using cold compresses during the acute phase can help reduce swelling and bruising. Over-the-counter analgesics such as acetaminophen or ibuprofen can help with pain management.
- Antibiotics: If there is a breach in the sinus wall or a risk of infection, prophylactic antibiotics may be recommended to prevent orbital cellulitis.
Surgical Intervention
Several scenarios call for surgery:
- Displaced Fractures: If a fracture causes significant bone displacement, surgical repair may be required to restore the normal anatomy of the orbit and avoid cosmetic deformities.
- Muscle Entrapment: When extraocular muscles become trapped within the fracture site, causing restricted eye movements and double vision, surgical intervention is required to free the muscle.
- Orbital Floor Reconstruction: In the case of blowout fractures, reconstruction of the orbital floor may be required to prevent enophthalmos and provide proper eye support. Titanium mesh, porous polyethylene implants, and autologous bone grafts are all options for accomplishing this.
- Orbital Roof and Medial Wall Fractures: These fractures frequently necessitate surgical intervention to prevent complications such as cerebrospinal fluid leaks, encephaloceles, or significant cosmetic deformities.
Innovative and Emerging Therapies
- Minimally Invasive Techniques: Advances in endoscopic techniques have enabled less invasive surgical approaches to the repair of certain types of orbital fractures, particularly blowout fractures. These techniques reduce surgical complications and shorten recovery times.
- Custom 3D-Printed Implants: 3D printing technology has enabled the development of patient-specific implants for orbital reconstruction, resulting in a better anatomical fit and potentially better outcomes.
- Biodegradable Implants: New research on biodegradable implants for orbital floor reconstruction seeks to provide temporary support during healing before gradually degrading and being absorbed by the body, reducing the need for permanent foreign materials.
- Regenerative Medicine: Research into regenerative medicine and tissue engineering holds promise for future treatments, with the potential to regenerate bone and soft tissues in the orbit and improve the outcomes of orbital fracture repairs.
Effective orbital fracture management requires timely diagnosis, appropriate conservative or surgical treatment, and consideration of innovative therapies to improve patient outcomes.
Effective Ways to Improve and Prevent Orbital Fractures
- Wear Protective Gear: Always wear appropriate protective gear, such as helmets and face shields, when participating in activities that pose a high risk of facial trauma, such as contact sports and construction work.
- Use Seatbelts: Always use seatbelts while driving or riding in a vehicle to reduce the risk of facial injuries in an accident.
- Fall Prevention: Take steps to prevent falls, particularly in older adults, such as installing handrails, securing loose rugs, and providing adequate lighting in the home.
- Sports Safety: Wear eye protection and use proper techniques to reduce the risk of facial injuries.
- Avoid Physical Altercations: Use conflict resolution techniques to avoid physical confrontations that could cause facial trauma.
- Strength Training: Perform strength and conditioning exercises to improve overall body stability and lower the risk of falls and injuries.
- Home Safety: Make sure your living space is free of hazards that could cause trips and falls, such as cluttered walkways and uneven floors.
- Regular Eye Exams: Regular eye examinations can help detect any pre-existing conditions that may increase the risk of eye injuries or complicate the treatment of orbital fractures.
- Awareness and Education: To increase safety and awareness, educate yourself and others about the risks and preventive measures associated with orbital fractures.
Trusted Resources
Books
- “Orbital Trauma: Principles and Practice” by Alaa El-Hindy and Chris L. T. Roxburgh
- “Management of Orbital and Ocular Adnexal Tumors and Inflammations” by Arun D. Singh and Brijesh K. Singh
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn
Online Resources
- American Academy of Ophthalmology (AAO): aao.org
- American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS): asoprs.org
- National Eye Institute (NEI): nei.nih.gov






