What is Corneal Degenerations?
Corneal degenerations refer to a group of ocular disorders characterized by progressive changes and deterioration of the corneal tissue. These conditions can lead to significant visual impairment and discomfort. Unlike corneal dystrophies, which are typically hereditary and present early in life, corneal degenerations are often associated with aging, trauma, inflammation, or other underlying medical conditions. The cornea, the clear front surface of the eye, is crucial for maintaining vision clarity and focus. When degenerative changes occur, they can compromise the structural integrity and transparency of the cornea, leading to various symptoms and complications. Understanding the different types of corneal degenerations, their causes, and their impact on eye health is essential for early detection and effective management.
Corneal Degeneration Insights
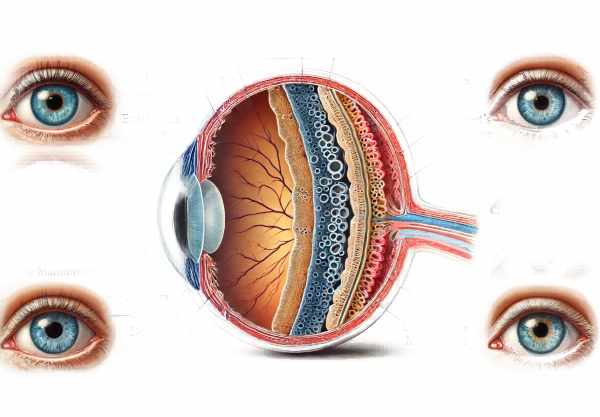
Corneal degenerations encompass a variety of conditions, each with unique etiologies, manifestations, and implications for vision. The cornea is composed of five layers: the epithelium, Bowman’s layer, the stroma, Descemet’s membrane, and the endothelium. Degenerative changes can affect any of these layers, leading to distinctive clinical features.
Types of Corneal Degenerations
- Keratoconus: This is one of the most well-known corneal degenerations. Keratoconus involves the thinning and bulging of the cornea into a cone-like shape, causing distorted vision. It typically starts in adolescence and progresses over time. The exact cause is unknown, but genetic and environmental factors are believed to play a role.
- Terrien’s Marginal Degeneration: Characterized by peripheral thinning of the cornea, Terrien’s marginal degeneration often begins in the superior cornea and can progress circumferentially. This condition usually affects older adults and can lead to irregular astigmatism and vision loss.
- Mooren’s Ulcer: A painful, chronic ulcerative condition, Mooren’s ulcer causes peripheral corneal thinning and can lead to perforation if untreated. The etiology is not fully understood, but it may involve an autoimmune response.
- Fuchs’ Endothelial Dystrophy: Although classified as a dystrophy, this condition involves degenerative changes in the endothelial cells. It leads to corneal edema and blurred vision due to the failure of the endothelium to maintain corneal dehydration.
- Limbal Girdle of Vogt: This condition is characterized by white, crescent-shaped deposits near the limbus (the border between the cornea and the sclera). It is commonly seen in older adults and is usually asymptomatic but can be associated with vision disturbances if it extends into the central cornea.
- Band Keratopathy: This degeneration involves the deposition of calcium salts in the superficial cornea, leading to a band-like appearance. It can result from chronic inflammation, hypercalcemia, or other systemic conditions and can cause visual impairment if the deposits become dense.
Pathophysiology
The underlying mechanisms of corneal degenerations vary depending on the specific condition but generally involve disruptions in cellular and extracellular matrix homeostasis.
- Structural Changes: In conditions like keratoconus, changes in the collagen structure and enzymatic degradation lead to thinning and biomechanical weakening of the cornea. This results in the characteristic conical deformation.
- Inflammatory Processes: Inflammatory mediators play a significant role in conditions like Mooren’s ulcer and Terrien’s marginal degeneration. Chronic inflammation leads to tissue damage, thinning, and ulceration.
- Metabolic Imbalances: Disorders like band keratopathy involve metabolic imbalances that lead to the deposition of abnormal substances in the cornea. Calcium deposition in band keratopathy disrupts the normal transparency of the cornea.
- Cellular Dysfunction: In Fuchs’ endothelial dystrophy, the dysfunction and loss of endothelial cells impair the cornea’s ability to pump out excess fluid, leading to stromal edema and vision loss.
Symptoms and Clinical Features
The symptoms of corneal degenerations vary widely based on the specific condition and its severity. Common symptoms include:
- Visual Disturbances: Blurred vision, ghosting, and halos are common as the cornea’s shape and transparency are altered.
- Pain and Discomfort: Conditions involving ulceration or significant thinning, such as Mooren’s ulcer, can cause severe pain.
- Photophobia: Increased sensitivity to light is often seen in conditions that disrupt the smooth surface of the cornea.
- Foreign Body Sensation: Irregularities on the corneal surface can create a sensation of something being in the eye.
Risk Factors
Several factors can increase the risk of developing corneal degenerations:
- Genetic Predisposition: Family history plays a role, particularly in conditions like keratoconus.
- Age: Many degenerative conditions, such as Fuchs’ endothelial dystrophy and limbal girdle of Vogt, are more common in older adults.
- Environmental Factors: UV exposure and eye rubbing have been implicated in the progression of keratoconus.
- Systemic Conditions: Diseases like rheumatoid arthritis and hypercalcemia can predispose individuals to corneal degenerations like Mooren’s ulcer and band keratopathy.
Impact on Vision
The impact of corneal degenerations on vision depends on the extent and location of the degenerative changes:
- Irregular Astigmatism: Thinning and deformities of the cornea, as seen in keratoconus, lead to irregular astigmatism that cannot be corrected with glasses.
- Decreased Visual Acuity: Edema and scarring, particularly in the central cornea, significantly reduce visual acuity.
- Visual Fluctuations: Conditions like Fuchs’ endothelial dystrophy cause vision to fluctuate, especially upon waking, due to changes in corneal hydration.
Understanding these diverse aspects of corneal degenerations is crucial for developing effective diagnostic and therapeutic strategies.
Prevention Tips
- Protect Your Eyes: Always wear protective eyewear during activities that pose a risk of eye injury, such as sports, woodworking, or handling chemicals.
- Avoid Eye Rubbing: Refrain from rubbing your eyes, as this can exacerbate conditions like keratoconus and contribute to corneal thinning.
- Manage Systemic Conditions: Keep systemic conditions, such as diabetes and rheumatoid arthritis, under control with appropriate medical management to reduce the risk of associated corneal degenerations.
- Use Proper Contact Lens Hygiene: Follow recommended guidelines for contact lens use, including proper cleaning, storage, and timely replacement to prevent infections and corneal damage.
- Regular Eye Exams: Schedule regular comprehensive eye exams to detect early signs of corneal degenerations and other eye conditions.
- Protect Against UV Exposure: Wear sunglasses that block 100% of UV rays to protect your corneas from harmful ultraviolet radiation.
- Stay Hydrated: Adequate hydration helps maintain overall eye health and can prevent dryness that might contribute to corneal issues.
- Use Lubricating Eye Drops: If you experience dry eyes, use lubricating eye drops to keep the corneal surface moist and healthy.
- Avoid Smoking: Smoking can contribute to oxidative stress and inflammation, which are risk factors for various eye conditions, including corneal degenerations.
- Follow Prescribed Treatments: Adhere to any prescribed treatments or medications for pre-existing eye conditions to prevent complications and further degeneration.
Diagnostic Methods
Diagnosing corneal degenerations involves a combination of clinical evaluation and advanced diagnostic tools to accurately identify and assess the extent of the condition. Here are some of the standard and innovative diagnostic techniques used:
- Slit Lamp Examination: This is the cornerstone of corneal diagnosis. Using a slit lamp, eye care professionals can closely examine the cornea’s layers, detecting abnormalities such as thinning, deposits, and ulcerations. The slit lamp provides high magnification and illumination, allowing for detailed visualization of corneal structures.
- Corneal Topography: This non-invasive imaging technique maps the surface curvature of the cornea. It is particularly useful in diagnosing keratoconus and other conditions that alter the corneal shape. Corneal topography creates a detailed, color-coded map that highlights areas of steepening and thinning, aiding in the detection of even subtle changes.
- Pachymetry: Pachymetry measures the thickness of the cornea, which is crucial for diagnosing conditions like keratoconus and Terrien’s marginal degeneration. Ultrasonic or optical pachymeters provide accurate corneal thickness readings, helping to monitor disease progression and guide treatment decisions.
- Ocular Coherence Tomography (OCT): OCT provides high-resolution cross-sectional images of the cornea, allowing for detailed assessment of each corneal layer. This technique is invaluable for diagnosing and monitoring conditions such as Fuchs’ endothelial dystrophy, where changes in the endothelial layer and corneal thickness are critical indicators.
- Confocal Microscopy: This advanced imaging technique offers in vivo, high-resolution images of the cornea at the cellular level. It is particularly useful for detecting inflammatory cells, endothelial cell loss, and other microscopic changes that occur in degenerative corneal conditions.
- Specular Microscopy: Specular microscopy focuses on the endothelial layer of the cornea, providing detailed images and cell counts. This is essential for diagnosing and managing Fuchs’ endothelial dystrophy, where endothelial cell density and morphology are key parameters.
- Genetic Testing: For hereditary corneal degenerations like keratoconus, genetic testing can identify specific mutations associated with the condition. While not routinely used in clinical practice, genetic testing is an emerging tool that can provide insights into the risk and prognosis of degenerative corneal diseases.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT is a specialized form of OCT that provides detailed imaging of the anterior segment, including the cornea, iris, and lens. It is particularly useful for assessing the depth and extent of corneal lesions and for pre-surgical planning.
- Biomechanical Assessment: Technologies like the Ocular Response Analyzer (ORA) and Corvis ST measure corneal biomechanical properties. These assessments are particularly useful in diagnosing keratoconus and evaluating the risk of ectasia in refractive surgery candidates.
Treatment
The treatment of corneal degenerations depends on the specific condition, its severity, and the patient’s overall health. Here, we delve into standard treatment options and highlight innovative and emerging therapies.
Standard Treatments
- Eyeglasses and Contact Lenses: For conditions like keratoconus, eyeglasses or specially designed contact lenses (such as rigid gas permeable lenses or scleral lenses) can correct visual distortions and improve vision. Contact lenses help by providing a smooth refractive surface, compensating for the irregular corneal shape.
- Medications: Anti-inflammatory medications, such as corticosteroid eye drops, can help manage inflammation in conditions like Mooren’s ulcer. In Fuchs’ endothelial dystrophy, hypertonic saline drops or ointments may be used to reduce corneal edema.
- Corneal Cross-Linking (CXL): CXL is a relatively new treatment primarily for keratoconus. It involves the application of riboflavin (vitamin B2) eye drops followed by exposure to UV light, which strengthens the corneal collagen fibers and stabilizes the cornea, preventing further progression.
- Intacs: These are small, crescent-shaped plastic inserts placed in the cornea to flatten the cone shape in keratoconus. Intacs can improve vision and may delay or eliminate the need for a corneal transplant.
- Phototherapeutic Keratectomy (PTK): PTK uses an excimer laser to remove superficial corneal opacities and irregularities, which can improve vision and reduce symptoms in conditions like band keratopathy.
- Corneal Transplantation: For advanced cases, corneal transplantation (keratoplasty) may be necessary. This can involve replacing the full thickness of the cornea (penetrating keratoplasty) or just the diseased layers (lamellar keratoplasty). Endothelial keratoplasty is often used for Fuchs’ endothelial dystrophy.
Innovative and Emerging Therapies
- Descemet Membrane Endothelial Keratoplasty (DMEK): This is a type of endothelial keratoplasty that involves transplanting only the endothelial layer and Descemet’s membrane. DMEK offers faster visual recovery and better outcomes compared to traditional full-thickness transplants.
- Stem Cell Therapy: Emerging research is exploring the use of stem cells to regenerate damaged corneal tissue. Stem cell therapy holds promise for conditions like limbal stem cell deficiency and severe keratoconus, potentially restoring normal corneal function and transparency.
- Gene Therapy: Advances in gene therapy are being investigated to correct genetic mutations responsible for certain corneal degenerations. While still experimental, gene therapy could offer a targeted approach to treating hereditary corneal disorders.
- Artificial Corneas: For patients who are not candidates for traditional corneal transplants, artificial corneas (keratoprostheses) provide an alternative. These devices can restore vision in cases where other treatments have failed.
- Nanotechnology-Based Treatments: Research into nanotechnology is opening new avenues for drug delivery systems in eye care. Nanoparticles can be designed to deliver therapeutic agents directly to the cornea, enhancing the efficacy and reducing side effects of treatments.
Trusted Resources
Books
- “Corneal Degenerations and Dystrophies” by Jay H. Krachmer
- “Corneal Disorders: Clinical Diagnosis and Management” by Howard M. Leibowitz






