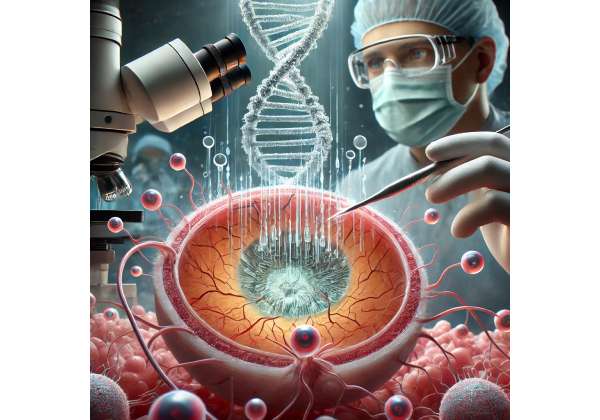
Age-Related Macular Degeneration (AMD) is a leading cause of vision loss worldwide, primarily affecting older adults. This progressive condition attacks the macula—the central part of the retina responsible for sharp, detailed vision—ultimately compromising a person’s ability to read, drive, and recognize faces. While conventional therapies have offered partial relief, recent advancements in gene editing have sparked new hope: CRISPR-enhanced cell therapy aims to revolutionize treatment by restoring retinal cells at the genetic level. Below, we explore this cutting-edge therapy’s core principles, clinical applications, efficacy, research insights, safety considerations, and financial factors, providing a holistic view of its transformative potential.
1. An Inside Look at CRISPR-Enhanced Cell Therapy: A Milestone in Macular Degeneration Care
CRISPR-enhanced cell therapy harnesses two groundbreaking biotechnologies: CRISPR-based gene editing and cell therapy (often involving stem cells or progenitor cells). By combining the capacity to precisely edit genetic material with the regenerative power of specialized cells, this therapeutic approach aims to tackle AMD at its source rather than merely slowing its progression.
What Makes This Therapy Unique?
- Precision Targeting: Traditional treatments for AMD—like injections aimed at controlling abnormal blood vessel growth—often focus on symptom management. CRISPR technology, on the other hand, can zero in on specific mutations or dysfunctional pathways.
- Regenerative Potential: Cell therapy offers a means to replace or revitalize lost or damaged retinal cells. When combined with CRISPR, transplanted cells can be genetically “corrected” or optimized for improved survival and integration.
- Broad Applicability: AMD is not a single-gene disorder; it is influenced by a complex interplay of genetic, lifestyle, and environmental factors. Nevertheless, certain key pathways—like complement system dysregulation—are now recognized as potential genetic editing targets.
A Shift in AMD Management
Traditionally, patients with wet AMD undergo anti-VEGF (Vascular Endothelial Growth Factor) injections to stem the growth of abnormal blood vessels, while those with dry AMD rely on nutritional supplements or other interventions to slow disease progression. CRISPR-enhanced cell therapy goes deeper, aiming to reprogram or restore essential retinal cells—particularly the retinal pigment epithelium (RPE)—which are crucial for supporting photoreceptors. This approach represents a paradigm shift: where current therapies primarily stabilize AMD, CRISPR-enhanced strategies strive to regenerate and revitalize vision.
Ethical and Regulatory Landscape
Regulatory bodies such as the FDA carefully scrutinize gene-editing therapies for safety and efficacy. While CRISPR-based approaches hold tremendous promise, the long-term implications of editing human DNA necessitate rigorous oversight. Many current clinical trials operate under strict protocols to safeguard patient welfare, ensuring the technology’s benefits substantially outweigh its risks.
Looking Forward
CRISPR-enhanced cell therapy stands poised to transform the course of AMD care. Early trials and preclinical studies are already yielding promising data, sparking optimism within the ophthalmic and scientific communities. As more research emerges, experts anticipate that CRISPR technology will become ever more refined, maximizing treatment effectiveness while minimizing potential side effects.
2. Age-Related Macular Degeneration: Unraveling the Core Challenges
Before delving into how CRISPR-enhanced cell therapy can reshape AMD management, it is crucial to understand the disease itself—its complexities, risk factors, and current interventions. With over 10 million Americans estimated to suffer from AMD, the condition represents a significant health concern, especially in aging populations.
Breaking Down AMD
AMD typically appears in two main forms: dry (atrophic) and wet (neovascular).
- Dry AMD (Atrophic)
- Characterized by the thinning of the macular region and the accumulation of protein-lipid deposits called drusen.
- Progresses slowly and can result in gradual central vision loss.
- Currently lacks highly effective treatments aside from nutritional interventions (AREDS2 supplements) that may slow progression.
- Wet AMD (Neovascular)
- Involves the abnormal growth of blood vessels beneath the retina, often leading to leakage of fluid or blood.
- Progresses rapidly and can cause sudden central vision loss.
- Standard treatments include periodic anti-VEGF injections designed to block blood vessel proliferation.
Risk Factors
- Age: The most significant factor; AMD typically manifests after age 50.
- Genetics: Variants in genes like CFH (complement factor H) and ARMS2 have been strongly linked to AMD risk.
- Lifestyle: Smoking, poor diet, and insufficient exercise can intensify disease progression.
- Ethnicity: Research suggests that people of European descent may be at elevated risk, though the condition affects all ethnic groups.
Challenges in Treatment
Despite the effectiveness of anti-VEGF for wet AMD, no cure exists for either form. Patients frequently require lifelong injections, which carry not only financial burdens but also inconvenience and potential procedural complications. Dry AMD, which constitutes around 80–90% of total AMD cases, remains particularly difficult to manage, as no regenerative therapy on the market fully reverses the loss of photoreceptors or RPE cells.
Why CRISPR?
CRISPR is uniquely suited for complex diseases like AMD because it can simultaneously address multiple genetic components. This advantage is significant given that AMD involves various molecular pathways, including oxidative stress, inflammation, and aberrant complement system activity.
Hopes for a Cure or Sustained Improvement
While experts caution that a universal cure for AMD may still be years away, CRISPR-enhanced cell therapy has invigorated the field with new possibilities. By leveraging precise genetic edits, practitioners could potentially correct detrimental mutations and replace degenerated cells, thereby offering a meaningful restoration of central vision for millions of affected individuals.
3. How CRISPR Brings Precision Editing to Retinal Cells
Central to the promise of CRISPR-enhanced cell therapy for AMD is CRISPR-Cas9, a gene-editing technology derived from bacterial immune systems. Understanding how CRISPR functions at the molecular level illuminates the therapy’s mechanism for repairing and rejuvenating retinal cells.
CRISPR-Cas9 Basics
- Guide RNA (gRNA): A specially synthesized RNA sequence that directs the Cas9 enzyme to a precise genetic location.
- Cas9 Enzyme: Often described as “molecular scissors,” Cas9 cuts DNA at the site targeted by the guide RNA.
- DNA Repair Processes: Once Cas9 creates a break, the cell’s natural repair pathways—non-homologous end joining (NHEJ) or homology-directed repair (HDR)—step in. Researchers can harness HDR to insert a healthy gene segment or a beneficial modification.
Targeting AMD-Relevant Genes
In AMD, a myriad of genes can contribute to pathological changes in the retina. Researchers may target:
- CFH (Complement Factor H): Mutations here can amplify inflammatory responses that damage retinal cells.
- VEGF Pathway Genes: Editing these genes might reduce the overproduction of vascular growth factors in wet AMD.
- Mitochondrial Function Genes: Restoring efficient energy production in retinal cells could combat oxidative stress, a major factor in AMD progression.
Strategic Gene Editing in Stem or RPE Cells
Cell therapy often involves human-induced pluripotent stem cells (hiPSCs), embryonic stem cells, or patient-derived RPE cells. In the context of CRISPR:
- Cell Harvesting: Cells may be extracted from a patient or a donor.
- In Vitro Gene Editing: Using CRISPR, labs modify these cells by removing, replacing, or correcting problematic DNA sequences.
- Cell Differentiation: The edited cells are cultured under conditions that encourage them to develop into mature RPE cells or photoreceptors.
- Transplantation: These healthy, corrected cells are then implanted back into the patient’s retina, where they can ideally integrate and restore function.
Advantages Over Conventional Gene Therapy
- Precise Edits: CRISPR can make site-specific changes to the genome, reducing the risk of undesired “off-target” disruptions that occasionally occur with older gene therapy approaches using viral vectors.
- Permanent Correction: Once the genomic alteration is in place, it can persist indefinitely, eliminating the need for frequent re-treatment.
- Customizable: Each patient’s genetic background can be scrutinized, allowing for tailored gene edits that address individual risk profiles or mutational variants.
Minimizing Off-Target Effects
One important scientific challenge is ensuring CRISPR does not inadvertently cut or modify DNA in the wrong places. Current solutions include:
- High-Fidelity Cas9 Variants: Engineered versions of Cas9 that exhibit reduced off-target activity.
- In Silico Screening: Using computational tools to predict potential off-target sites and design guide RNAs with minimal overlap.
- Thorough Validation: Conducting extensive genomic sequencing both in vitro and post-therapy to confirm changes occurred only at the intended loci.
By working in tandem with cell therapy, CRISPR’s precision editing capacity holds immense promise for tackling AMD’s complex genetic underpinnings. In the following sections, we explore how these molecular breakthroughs transition from the laboratory to the clinical realm.
4. From Lab to Clinic: Protocols and Application Methods
Turning CRISPR-enhanced cell therapy into a viable treatment for AMD requires meticulous protocols that span patient selection, cell engineering, and transplant procedures. Each step leverages advanced ophthalmic and molecular biology techniques to promote safety and efficacy.
1. Patient Evaluation and Eligibility
- Genetic Profiling: Since AMD can be influenced by specific gene variants, comprehensive genetic testing helps identify prime candidates for CRISPR-based interventions.
- Ophthalmic Assessments: Tests like optical coherence tomography (OCT), fundus examination, and visual acuity measurements help pinpoint disease severity and progression.
- Medical History Review: A thorough medical history verifies the absence of contraindications (e.g., active ocular infections or other complicating factors).
2. Cell Harvesting and Preparation
Autologous vs. Allogeneic:
- Autologous: Cells derived from the patient, reduced risk of immune rejection but more time-intensive.
- Allogeneic: Cells derived from healthy donors, faster but requires immune suppression to avert transplant rejection.
Cell Types:
- RPE Cells: Harvested from donor sources or generated from patient-derived stem cells.
- Photoreceptor Precursors: Some labs focus on reconstituting not just support cells (RPE) but also photoreceptors, which are crucial for capturing light signals.
3. CRISPR Editing and Cell Cultivation
Once harvested, the cells undergo a series of laboratory steps:
- Gene Editing: Introduction of CRISPR-Cas9 components into the cells to correct or disable harmful mutations.
- Expansion and Differentiation: Edited cells are nurtured in specialized media that encourage them to mature into RPE or photoreceptor cells.
- Quality Control: Researchers screen for off-target edits, confirm expression of key retinal markers, and evaluate cell viability.
4. Surgical Delivery: Subretinal or Intravitreal Transplantation
Transplanting CRISPR-edited cells into the retina typically involves subretinal injections, wherein a small bleb of fluid containing the therapeutic cells is introduced beneath the retina. This approach ensures close contact between transplanted cells and the host retina, fostering better integration. In some experimental protocols, intravitreal injections—introducing the cells into the vitreous cavity—are explored but may not offer the same direct contact with diseased retinal layers.
5. Post-Operative Monitoring
After the transplant, patients usually undergo:
- Imaging Follow-Up: OCT and fundus imaging to track the positioning and survival of transplanted cells.
- Visual Function Tests: Periodic examinations to measure possible gains in acuity, color discrimination, or contrast sensitivity.
- Immune Surveillance: Monitoring for inflammatory responses, especially if the therapy involves allogeneic cells.
6. Reinforcement Therapies
Researchers often pair CRISPR-enhanced cell therapy with supportive treatments, such as:
- Anti-VEGF Injections: If wet AMD is also present.
- Nutritional Support: Vitamins and minerals like zinc, lutein, and zeaxanthin to support retinal health.
- Immunomodulators: Drugs that reduce rejection risk or inflammation in the transplanted site.
The smooth transition from the lab bench to clinical practice hinges on these meticulously structured protocols. With best practices continuously refined through ongoing trials, the next step is to examine real-world outcomes, safety profiles, and the therapy’s overall effectiveness.
5. Positive Outcomes and Safety Profile: What We Know So Far
CRISPR-enhanced cell therapy stands at the intersection of regenerative medicine and gene editing, offering a unique vantage point to tackle AMD. While still emerging, both preclinical studies and early clinical investigations suggest notable benefits and a manageable safety profile.
1. Demonstrated Efficacy in Preclinical Models
Animal models, such as rodents genetically engineered to develop AMD-like symptoms, have shown:
- Retinal Cell Survival: Transplanted, CRISPR-edited cells improved photoreceptor and RPE survival rates.
- Enhanced Function: Electroretinogram (ERG) measures indicated stronger retinal responses compared to untreated controls.
- Reduced Inflammation: Targeting pro-inflammatory genes via CRISPR helped modulate damaging immune responses in the retina.
2. Early Clinical Observations
Though long-term data remains limited, preliminary reports from small clinical studies reveal:
- Improved Visual Acuity: Some patients experienced measurable gains in reading letters on an eye chart.
- Stable Integration: Imaging indicated that transplanted cells integrated with the host retina without extensive scarring or displacement.
- Durable Gene Edits: Tissue analyses from post-operative follow-ups showed that CRISPR-introduced genetic modifications persisted, suggesting a potential long-lasting effect.
3. Safety and Potential Risks
Like any pioneering therapy, CRISPR-enhanced cell therapy is not without risks. Key concerns include:
- Off-Target Editing: While advanced guide RNA design mitigates random DNA cuts, the possibility remains.
- Immunological Reactions: Allogeneic cell therapies may provoke immune responses, though immunosuppressive regimens can reduce these risks.
- Surgical Complications: Subretinal injections are delicate procedures that carry small yet significant risks of bleeding, infection, or retinal detachment.
Researchers and clinicians often highlight stringent monitoring as a cornerstone of early clinical applications. Patients typically remain under close observation for months or even years, with frequent genetic and ophthalmic testing to catch any emerging safety issues promptly.
4. Regulatory Oversight and Quality Control
Regulatory bodies require extensive documentation of manufacturing processes, including details on CRISPR-Cas9 constructs, cell culture conditions, and sterility measures. This vigilant oversight is designed to ensure that therapies maintain high standards of safety, purity, and consistency before reaching a broader patient population.
5. Ethical Considerations
As a form of gene editing, CRISPR-based treatments trigger ethical questions:
- Germline Alterations: Current protocols focus solely on editing somatic cells (like RPE cells), meaning changes are not passed to offspring.
- Equitable Access: High development costs could limit who benefits from these advancements, highlighting the need for policy interventions to ensure broad and fair availability.
Overall, early data depict a promising therapy with significant upside in terms of visual restoration and a safety profile that—while not entirely risk-free—seems encouraging. The next section explores how ongoing research, from small-scale pilot trials to larger, multi-center studies, is propelling CRISPR-enhanced cell therapy closer to mainstream application.
6. Recent Breakthroughs: Research, Trials, and Real-World Results
The momentum behind CRISPR-enhanced cell therapy for AMD has accelerated thanks to collaborative efforts among academic institutions, biotech firms, and clinical research centers. Below are some latest research insights reflecting the current landscape.
Landmark Clinical Trials
- Phase I/II Studies with CRISPR-Corrected RPE Cells
- Multiple institutions have launched early-phase trials to test safety and initial efficacy in wet AMD patients. According to interim reports, participants have shown stabilization in visual acuity and minimal adverse events.
- Imaging data confirm that transplanted cells remain viable up to a year post-injection.
- Multi-Center Investigations on Dry AMD
- Researchers in Europe and North America are collaborating on a trial targeting complement pathway genes known to exacerbate dry AMD. Preliminary data suggest CRISPR-modified RPE transplants can slow drusen accumulation and reduce atrophic changes.
- These findings are particularly significant given the lack of robust treatments for advanced dry AMD.
Real-World Case Studies
- Notable Single-Patient Success: In one high-profile case, a patient in a Phase I trial regained enough visual function to distinguish faces and read larger print without magnification, a marked improvement from their baseline.
- Reduced Injection Frequency: Another early trial indicated that patients receiving CRISPR-edited cell therapy required fewer follow-up anti-VEGF injections—an encouraging sign for wet AMD management.
Supporting Data and Statistics
- Durability of Gene Edits: A paper published in Nature Biomedical Engineering reported that over 70% of gene edits remained stable in transplanted RPE cells six months after injection.
- Enhanced RPE Function: Lab-based assays demonstrated up to a 40% increase in phagocytosis, a critical function of RPE cells for cleaning up photoreceptor outer segments.
International Collaborations and Funding
Major funding bodies such as the National Institutes of Health (NIH) in the U.S. and the European Commission’s Horizon Europe program are supporting expanded research on CRISPR-based interventions for retinal diseases. This global attention boosts both the scale and quality of research, expediting progress toward mainstream availability.
Looking Ahead
Future trials aim to refine:
- Delivery Mechanisms: Improving subretinal injection techniques to minimize surgical risk and maximize cell engraftment.
- Off-Target Evaluation: Employing advanced sequencing technologies to continuously monitor for unintended edits.
- Combination Therapies: Pairing CRISPR-enhanced transplants with new pharmacological agents targeting retinal metabolism or immune regulation.
Every new study contributes valuable insights into how to optimize CRISPR-enhanced cell therapy for AMD, paving the way for larger trials that will ultimately shape regulatory approvals, clinical guidelines, and patient access.
7. Weighing the Costs: A Closer Look at Therapy Pricing
CRISPR-enhanced cell therapy for AMD entails intricate laboratory processes, specialized surgical expertise, and extensive post-operative monitoring. These factors contribute to a considerable price tag, which can vary widely based on the treatment center, region, and specific protocol. Some biotech companies place initial therapy costs in the range of $50,000 to $150,000, but prices can escalate for more complex cases requiring custom-engineered cells or multi-stage procedures. Insurance coverage is still evolving; select plans may partially reimburse such experimental treatments, while others classify them under “investigational” and do not cover the associated expenses. Additionally, some clinical trials offer subsidized or fully covered treatments for eligible participants, easing the financial burden. As gene editing technologies become more widespread, experts anticipate the possibility of reduced costs and broader accessibility, allowing more individuals with AMD to benefit from this transformative approach.
Disclaimer:
This article is intended for informational purposes only and does not replace professional medical consultation. Always seek the guidance of a qualified healthcare provider with any questions about your medical condition or treatment options.
We encourage you to share this article with friends, family, or on social media platforms like Facebook and X (formerly Twitter). By doing so, you can help others learn about the promising future of CRISPR-enhanced cell therapy and its potential to restore vision in Age-Related Macular Degeneration. Simply use the share buttons provided or any other method you prefer—together, we can bring renewed hope and awareness to people seeking advanced eye care solutions.