Retinal tears are a critical eye emergency that can lead to permanent vision loss if left untreated. One of the most effective treatment methods to seal these tears and safeguard visual health is cryopexy, a specialized procedure that uses controlled, localized freezing to reattach or stabilize retinal tissue. Below is an in-depth look at this therapy’s core principles, benefits, clinical strategies, and scientific underpinnings, offering a comprehensive resource for those seeking to understand how cryopexy works to avert serious vision complications.
1. A Closer Look at Cryotherapy: An Essential Treatment for Retinal Tears
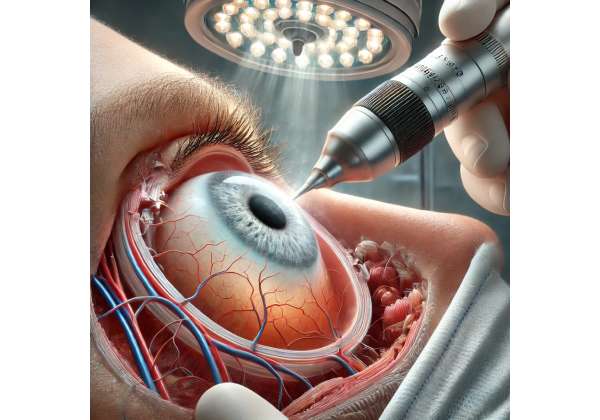
Cryopexy, often referred to as “cryo therapy” for the eye, is based on the principle of creating a meticulously controlled freeze-thaw cycle that promotes retinal adhesion. By applying extreme cold to the retina through a probe, ophthalmologists trigger a localized inflammatory response. This mild inflammation effectively “welds” or seals the retina back in place, preventing fluid from passing through the tear and halting the progress of potential retinal detachments. While the notion of freezing tissue may sound drastic, modern cryopexy techniques are highly refined, safe, and precise.
Background of Cryopexy in Ophthalmology
- Historical Roots: The concept of using cold therapy to treat eye disorders dates back several decades. Surgeons initially experimented with cryoprobes for various retinal issues, including tears and certain vascular lesions.
- Gradual Refinement: Over time, cryoprobes became smaller and more accurate, allowing surgeons to limit treatment to the precise retinal tear site without significantly impacting surrounding tissues.
- Synergy with Other Treatments: Cryopexy is frequently combined with other interventions, such as laser photocoagulation or scleral buckle surgery, depending on the complexity of the tear and the patient’s overall ocular health.
Why Cryotherapy Instead of Other Methods?
While laser photocoagulation is another leading choice for retinal tears, cryopexy offers unique advantages in certain cases:
- Opacities: If the patient’s view of the retina is obstructed (e.g., due to cataracts, hemorrhage, or clouding), lasers may not penetrate effectively, making cryopexy a more suitable option.
- Peripheral Tears: Peripheral retinal breaks that are hard to access with laser can often be better reached using a cryoprobe positioned under the conjunctiva.
- Effective Seal: Studies suggest that the freeze-thaw process creates a robust chorioretinal scar, securely sealing the tear site and lowering the likelihood of subsequent fluid leaks.
Patient Demographics
Cryopexy can be employed in a variety of patient populations:
- Younger Individuals: Occasional retinal tears from trauma or high myopia.
- Older Patients: Degenerative changes in the vitreous can pull on the retina, creating tears.
- Post-Surgical Patients: Cryopexy may be used as part of an integrated surgical plan if complications arise during or after cataract surgery, vitrectomy, or other ocular procedures.
Procedure Goals
The overarching objective is to halt the progression to retinal detachment, which can lead to profound vision loss. By acting swiftly—often as an outpatient procedure—cryopexy aims to minimize trauma, reduce surgical complexity, and preserve as much healthy retina as possible.
2. What Are Retinal Tears? Understanding Their Causes and Symptoms
Retinal tears occur when the light-sensitive layer at the back of the eye (the retina) develops a break or rip. These tears typically result from a combination of mechanical forces, age-related wear, or sudden trauma. Without prompt intervention, fluid from the vitreous cavity can seep through the tear, lifting the retina away from its underlying layers—an advanced stage referred to as retinal detachment.
Why Do Retinal Tears Happen?
- Vitreous Detachment: In many cases, the vitreous (a gel-like substance filling the eye) naturally shrinks or liquefies as people age. This process can tug on the retina, creating small rips.
- High Myopia (Nearsightedness): Individuals with significant myopia often have elongated eyeballs, which place the retina under increased tension.
- Eye Trauma: Accidents, sports injuries, or blunt force can generate sudden impacts that tear the retina.
- Surgical Complications: Certain eye surgeries (e.g., cataract removal or vitrectomy) carry a slight risk of causing or uncovering retinal breaks.
Signs and Symptoms
Retinal tears can present with subtle or sudden symptoms, underscoring the importance of seeking an ophthalmic evaluation if you notice:
- Flashes of Light: Brief, bright flashes, especially in peripheral vision, can indicate retinal traction.
- Floaters: Dark specks or strands drifting across the field of vision, which can signify bleeding or vitreous changes near the tear.
- Shadow or Curtain: A dark curtain-like shape encroaching from the edges of the visual field may signal progression toward detachment.
- Blurred or Distorted Vision: Although less common for small tears, advanced cases can cause significant distortion.
Diagnostic Tools
Ophthalmologists rely on a variety of instruments and tests to diagnose retinal tears:
- Dilated Fundus Examination: Using a magnified view of the retina, the specialist checks for tears, holes, or suspicious lesions.
- Ocular Ultrasound: Useful if the retina cannot be visualized directly due to cloudiness or bleeding.
- Optical Coherence Tomography (OCT): Provides high-resolution, cross-sectional images of the retina, revealing fluid accumulation or subtle breaks.
Risk Factors
- Family History: Certain inherited retinal degenerations may predispose individuals to tears.
- Lifestyle: Activities involving intense eye strain or potential impact (e.g., heavy sports) could increase risk.
- Medical History: Existing eye conditions like lattice degeneration or previous ocular surgeries can raise susceptibility.
When to Act
Rapid treatment can be the difference between stable vision and significant loss. If a tear progresses to partial or total retinal detachment, more complex surgeries (e.g., scleral buckle, vitrectomy) may be necessary. Therefore, early detection and timely intervention remain paramount.
3. How Cryopexy Works: The Science Behind Freezing Lesions
At first glance, freezing tissue might appear counterintuitive for healing. However, cryopexy exploits the body’s natural inflammatory and regenerative mechanisms. By inducing a controlled freeze at the tear site, physicians harness a response that bonds the retina to the underlying tissue (the choroid), effectively sealing off any entry points for fluid or further vitreous traction.
The Physics of Freezing the Retina
- Cryoprobe Application: During cryopexy, a thin, pen-like probe is inserted through the conjunctiva (the clear membrane covering the sclera) or gently placed on the eye’s surface over the approximate tear location.
- Rapid Temperature Drop: The cryoprobe lowers the temperature of the target tissue to well below freezing, often between -60°C to -80°C.
- Ice Crystal Formation: Small ice crystals form within the retinal layers, creating a zone of localized tissue injury.
Phase of Controlled Inflammation
Once the tissue is carefully thawed, the body’s immune system sends repair cells to the area:
- Inflammatory Response: White blood cells, cytokines, and other mediators arrive to clean up and stabilize the region.
- Scar Formation: A mild scar, or adhesion, forms between the retina and underlying layers. This seal is strong enough to prevent fluid from re-entering.
- Long-Term Reinforcement: Over time, the inflammatory signals diminish, leaving a permanent, secure bond.
Precision and Timing
Ensuring the freeze is both accurate and sufficiently localized is essential:
- Spot Freezing: Often, small, circular “freeze burns” are applied around and across the tear perimeter.
- Multiple Applications: Surgeons may repeat the freeze-thaw cycle several times to achieve an optimal chorioretinal scar.
- Real-Time Visualization: Ophthalmologists use an indirect ophthalmoscope or specialized lenses to visualize the retina throughout the procedure, ensuring the cryoprobe targets the exact tear location.
Advantages of the Freeze-Thaw Method
- Reduced Bleeding: Compared to surgical incisions or more invasive techniques, cryopexy typically results in minimal bleeding.
- Effective for Peripheral Lesions: By maneuvering the cryoprobe externally, surgeons can reach even peripheral or posterior segment tears that might be difficult to visualize through a laser.
- Minimal Collateral Damage: The controlled freeze focuses on the tear area, minimizing harm to adjacent healthy retina or surrounding tissues.
Possible Discomfort and Mitigation
While cryopexy is often performed under local anesthesia, patients may feel pressure or mild pain:
- Topical or Local Anesthesia: Numbing eye drops or a minor anesthetic injection can significantly reduce discomfort.
- Short-Term Swelling: Some swelling of eyelids or mild redness may persist for a day or two but generally subsides quickly.
Understanding these physiological and procedural elements helps demystify why cryopexy is highly effective at managing retinal tears and preventing more severe complications like detachment. In the next sections, we look deeper into the specific steps, safety, and overall success rates connected with this therapy.
4. Step-by-Step Treatment Protocols for Cryopexy
Cryopexy can be administered as a stand-alone treatment for straightforward retinal tears or incorporated into a multi-pronged surgical plan for more complicated cases. While individual approaches vary by patient and specialist, the outline below provides a snapshot of the key phases involved in performing cryopexy.
1. Preoperative Evaluation
- Patient History: Medical and ocular histories are reviewed to ensure no contraindications exist (e.g., severe eye infections).
- Imaging: If the tear is not easily visible, ultrasound or OCT can help determine its exact size and location.
- Discussion of Options: An ophthalmologist may consider laser photocoagulation instead of cryopexy if the tear is small and easily accessed. If the tear is peripheral or visual clarity is poor, cryopexy may be the better choice.
2. Anesthesia
Depending on the patient’s comfort level and the complexity of the tear:
- Topical Eye Drops: Sufficient for minor tears near the eye’s front portion.
- Local Injection (Retrobulbar or Peribulbar): Offers more profound anesthesia for deeper or multiple tears.
3. Positioning and Visualization
- Patient’s Position: The patient typically reclines in a specialized examination or operating chair that tilts backward.
- Indirect Ophthalmoscope: Allows the surgeon to see a wide field of the retina.
- Scleral Depression: In some cases, the physician may gently press on the outside of the eye to manipulate the retina into a better view.
4. Application of the Cryoprobe
- Identifying the Tear: The surgeon aligns the tip of the cryoprobe over the sclera in the exact spot corresponding to the retinal break.
- Initiation of the Freeze: The cryoprobe is activated to lower the tissue temperature rapidly, forming a small white spot or “ice ball” visible through the ophthalmoscope.
- Cycle Duration: Each freeze typically lasts a few seconds. The probe may be activated multiple times to ensure a robust chorioretinal scar.
- Monitoring: The surgeon frequently checks the freeze intensity and spread, adjusting as needed to avoid overtreatment.
5. Postoperative Management
- Medication: Antibiotic eye drops or anti-inflammatory agents might be prescribed to prevent infection and control inflammation.
- Activity Restrictions: Patients are often advised to avoid strenuous activities for at least a week or two, allowing the retina to heal.
- Follow-Up Visits: Re-examination of the retina helps confirm that the tear is sealed and that no new breaks have developed.
6. Combining Cryopexy with Other Interventions
Cryopexy can be used in tandem with:
- Scleral Buckle: A band placed around the eye’s circumference to relieve traction on the retina.
- Vitrectomy: Removal of the vitreous gel to clear blood or scar tissue, often followed by gas or silicone oil injection.
- Pneumatic Retinopexy: Injection of a gas bubble that presses the retina against the eyewall, supplemented by cryopexy to seal any breaks.
Because of its versatility, cryopexy integrates well with a range of surgical solutions for retinal tears and early detachments, enhancing overall success rates and preventing the progression of vision-threatening complications.
5. Efficacy and Safety of Cryopexy for Retinal Tears
Cryopexy has garnered respect in the ophthalmic community for its proven track record in stabilizing retinal tears and halting further complications like detachment. Below is a closer look at the procedure’s success, potential risks, and postoperative considerations that influence patient outcomes.
Efficacy and Success Rates
- High Retinal Re-Attachment Rates: Studies indicate that when applied appropriately—especially in the early stages—cryopexy can lead to successful retinal reattachment rates exceeding 90%.
- Long-Term Stability: Once a firm chorioretinal scar forms, the treated area often remains stable for the patient’s lifetime, significantly reducing the risk of recurrent breaks.
- Minimal Recurrence: Compared to untreated tears, cryopexy lowers the chance of a tear enlarging or leading to a full-blown detachment, which could require more invasive procedures.
Safety Profile
Despite its effectiveness, like any medical procedure, cryopexy comes with certain risks:
- Temporary Vision Changes: Patients may notice blurred vision or increased floaters during the immediate recovery phase.
- Intraocular Pressure Changes: The intense cold can momentarily affect ocular fluid dynamics, but this issue usually resolves quickly.
- Risk of Infection: Rare yet possible; sterile techniques and postoperative antibiotic drops help mitigate this risk.
- Mild Bleeding: If the probe inadvertently damages a small blood vessel, minor bleeding might occur but typically subsides without intervention.
Potential Side Effects
- Swelling and Redness: Mild swelling of the eyelid or mild eye irritation can appear postoperatively.
- Subconjunctival Hemorrhage: This bruise-like appearance under the conjunctiva may develop but generally resolves on its own.
Factors Influencing Outcomes
- Timing of Intervention: Earlier detection and prompt treatment yield higher success rates.
- Operator Experience: Surgeons skilled in cryopexy can effectively locate and freeze the tear without excessive damage to surrounding tissue.
- Follow-Up Adherence: Patients who attend all recommended post-op appointments and follow guidelines on activity restrictions are less likely to experience complications.
Comparing Cryopexy and Laser Photocoagulation
Both cryopexy and laser therapy create a chorioretinal scar to seal a retinal tear, but their methodologies differ. While laser uses heat from focused light energy, cryopexy employs extreme cold. Laser photocoagulation is less invasive from the outside perspective—often done in-office with minimal external manipulation—but demands clear visibility of the retina. Cryopexy, on the other hand, can be performed with or without a clear line of sight, ideal for tears in obscured or peripheral regions.
Postoperative Quality of Life
The vast majority of patients resume normal activities within days to weeks, depending on the tear’s severity and any combined procedures. Many report no lingering discomfort once inflammation subsides, and some note confidence knowing that the risk of detachment has markedly decreased.
6. Recent Clinical Findings: Advancements in Cryopexy Research
Although cryopexy has been a cornerstone in retinal tear management for decades, ongoing research continues to refine its techniques, enhance safety, and optimize outcomes. Below, we explore the latest studies, emerging trends, and technological innovations that further support cryopexy’s vital role in ophthalmology.
Evidence-Based Efficacy
Multiple peer-reviewed articles underscore cryopexy’s strong efficacy in preventing retinal detachment:
- Retina Journal: Published data from a multicenter study showing that prompt cryopexy intervention for fresh retinal tears resulted in over 94% success in preventing progression to detachment during a two-year follow-up period.
- Ophthalmology Research: A comparative study of laser photocoagulation vs. cryopexy found that both methods had similar success rates for central or equatorial tears, but cryopexy was more effective for peripheral or difficult-to-visualize tears.
Innovations in Probe Design
Manufacturers are experimenting with:
- Miniature Cryoprobes: Smaller-diameter probes can minimize trauma, enabling precise freezing of micro-tears.
- Enhanced Temperature Control: Modern cryosystems allow surgeons to adjust freezing speed and intensity in real time, ensuring a more custom fit for each tear.
Combination Therapy Studies
Recent trials focus on pairing cryopexy with new adjunct therapies or advanced imaging:
- Intraoperative OCT Guidance: Real-time 3D imaging helps surgeons confirm the exact location and depth of the freeze, potentially reducing unnecessary scarring.
- Biologic Sealants: Investigational biologic adhesives, when combined with cryopexy, may reinforce the adhesion and expedite healing.
Long-Term Outcomes and Patient Satisfaction
Research indicates:
- High Retention of Visual Acuity: Patients treated early often maintain or regain near-normal visual acuity, emphasizing cryopexy’s value in preserving central vision.
- Positive Patient Experience: Surveys show that cryopexy patients generally find the procedure tolerable, noting only short-lived discomfort.
Therapy for Peripheral Retinal Degenerations
Ophthalmologists are also applying cryopexy to lattice degenerations, a thinning of peripheral retina where tears often originate. Preliminary results highlight fewer retina-related complications and stable ocular health over extended monitoring periods.
Future Directions
- Refined Imaging Protocols: Ocular imaging is advancing rapidly, offering more accurate tear detection, which can direct the freeze precisely.
- Robot-Assisted Surgery: Still in early stages, robotic instruments could eventually provide even more exact cryoprobe positioning and temperature control, further improving success rates and reducing surgeon fatigue.
These findings underscore cryopexy’s ongoing relevance in the clinical setting. As research evolves, cryopexy continues to prove its value for preventing serious vision loss among patients facing the threat of retinal tears.
7. Therapy Price: Cost Factors and Financial Considerations
Although pricing for cryopexy varies based on country, healthcare system, and individual patient factors, the overall cost typically falls between $1,500 to $3,500 if performed as an outpatient procedure in a specialized clinic. More complex cases requiring additional surgeries—like scleral buckle or vitrectomy—can significantly increase total expenses. Insurance coverage often helps offset costs, especially if the procedure is deemed medically necessary to prevent permanent vision loss. Some clinics offer payment plans or financial counseling for individuals concerned about upfront fees. Prices also differ depending on the surgeon’s expertise, the facility’s geographic location, and the need for advanced imaging or anesthesia services. Ultimately, an itemized cost breakdown from the treating facility is crucial for clarity.
Disclaimer:
This article is intended for informational purposes only and does not substitute professional medical advice. Always consult a qualified ophthalmologist or healthcare provider for personalized guidance regarding retinal tears or any other eye condition.
We invite you to share this article with friends, family, or on social media platforms such as Facebook and X (formerly Twitter). By sharing, you can help others learn about cryopexy’s benefits in preserving sight and preventing retinal detachment. Feel free to use our share buttons or any other method you prefer—together, we can spread knowledge and protect vision for more people.