Bullous keratopathy is a sight-threatening condition in which a failing or damaged corneal endothelium leads to persistent corneal swelling, opacification, and painful bullae (fluid-filled blisters). In years past, full-thickness corneal transplants were the mainstay for advanced endothelial disorders. However, modern breakthroughs now allow surgeons to isolate, culture, and transplant healthy corneal endothelial cells—an approach that can be far less invasive and yield excellent visual rehabilitation. This FDA-approved therapy for bullous keratopathy is changing the landscape of corneal care, expanding treatment options for thousands of patients each year. Below is a comprehensive, in-depth look at the therapy’s principles, clinical applications, safety profile, research findings, and costs.
1. Introducing Cultured Endothelial Cell Therapy: A New Paradigm in Corneal Replacement
Cultured endothelial cell therapy (CECT) involves growing functional corneal endothelial cells in specialized lab conditions and then delivering them to the patient’s diseased cornea. Historically, corneal transplants have relied on full or partial grafts of donor cornea. Yet limitations in donor tissue availability and the complexity of surgical graft insertion have spurred investigators to develop more targeted techniques.
What Sets This Therapy Apart
- Cell-Based, Not Tissue-Based
Instead of relying on intact donor corneas, surgeons can transplant expanded cultures of endothelial cells. This makes more efficient use of donor material because one donor cornea can yield multiple doses of cells, alleviating pressure on eye banks. - Minimally Invasive Delivery
In many protocols, these cultured cells are injected into the recipient eye through a small incision, often combined with a short-term air or gas bubble to press the cells against Descemet’s membrane. Patients can frequently recover faster than with a full-thickness graft. - Preservation of Corneal Structure
By replacing only the dysfunctional endothelium, the rest of the corneal layers—especially healthy stroma and epithelium—remain undisturbed. This approach retains the patient’s corneal shape and biomechanical strength, mitigating problems like high astigmatism or prolonged healing times.
FDA Approval Significance
The U.S. Food and Drug Administration’s endorsement underscores both the safety and efficacy of cultured endothelial cell therapy. Rigorous multi-phase clinical trials must establish that the intervention meets strict standards for minimizing risk and enhancing patient outcomes. Such approval paves the way for widespread clinical adoption, expanded insurance coverage, and ongoing refinement of treatment protocols.
Patient Populations That Benefit Most
- Bullous Keratopathy: Damage to the corneal endothelium—whether from surgical complications, trauma, or degenerative disease—leads to fluid accumulation, haze, and painful blisters. This new therapy offers a direct solution by restoring the endothelium’s pump function.
- Fuchs’ Endothelial Dystrophy: A common, inherited corneal endothelial disorder. Patients with early-to-moderate disease may benefit from cell therapy before advanced scarring develops.
- High-Risk Graft Failures: Individuals who have experienced repeated graft failures often have limited donor options. Cultured cells may provide a new route to achieve corneal clarity and relief from chronic edema.
Evolution from Concept to Clinic
The journey toward an FDA-approved solution for endothelial disorders involved basic research in stem cell biology, advanced culture techniques, and iterative surgical refinements. Collaborative efforts among corneal surgeons, cell biologists, and engineers have led to standardized processes for cultivating viable, high-density endothelial cell lines suitable for transplantation.
As an exciting bridge between regenerative medicine and ophthalmic surgery, cultured endothelial cell therapy is poised to transform how we address endothelial dysfunction. The next section dives deeper into the pathophysiology of bullous keratopathy, illuminating why such a high-precision therapy is necessary.
2. Bullous Keratopathy Explained: Why Endothelial Cells Matter
Bullous keratopathy is marked by persistent corneal swelling, or edema, that often leads to compromised vision and painful bullae formation on the corneal surface. This pathologic swelling stems from endothelial cell failure. Understanding the cornea’s complex architecture—and the endothelium’s essential function—highlights the importance of any therapy aimed at replacing lost or damaged endothelial cells.
Corneal Anatomy in Brief
The cornea is a transparent, dome-shaped window at the front of the eye. It comprises five primary layers:
- Epithelium: The outermost barrier, in contact with the tear film.
- Bowman’s Layer: A dense layer of collagen that provides structural integrity.
- Stroma: The thick, transparent middle layer, accounting for most of the cornea’s thickness and focusing power.
- Descemet’s Membrane: A thin, collagen-based membrane that supports the endothelial layer.
- Endothelium: The innermost monolayer of cells that crucially regulates corneal hydration and clarity.
Why the Endothelium is Irreplaceable
Unlike epithelial or stromal cells, human corneal endothelial cells do not regenerate significantly in vivo. When endothelial cells are lost—due to trauma, aging, disease, or surgery—they cannot multiply to replenish their ranks. The surviving cells must stretch and migrate to maintain coverage. Eventually, if enough cells are lost or compromised, the cornea cannot effectively pump out excess fluid, resulting in:
- Corneal Edema: Fluid accumulates in the stroma, making it thicker and more opaque.
- Bullae Formation: Fluid also seeps beneath the epithelium, creating painful blister-like bumps.
- Visual Distortion: Light scattering in the edematous cornea undermines clarity, leading to blurred or hazy vision.
Triggers and Risk Factors for Bullous Keratopathy
- Intraocular Surgeries: Procedures such as cataract extraction or intraocular lens placement can sometimes damage the endothelium, especially if complicated by high intraocular pressures or mechanical trauma.
- Fuchs’ Endothelial Dystrophy: Genetic predisposition leading to progressive endothelial cell dropout over time.
- Previous Corneal Transplants: Even partial transplants like Descemet’s Stripping Endothelial Keratoplasty (DSEK) or Descemet’s Membrane Endothelial Keratoplasty (DMEK) can fail, ultimately triggering bullous keratopathy if the new endothelium cannot maintain pumping capacity.
- Ocular Hypertension or Glaucoma: Chronically elevated intraocular pressures can harm endothelium, hastening cell loss.
Consequences of Long-Term Edema
- Pain and Light Sensitivity: Recurrent epithelial bullae can rupture, causing intense discomfort and photophobia.
- Corneal Scarring: Chronic swelling alters collagen fibrils in the stroma, leading to permanent haze or scars.
- Reduced Quality of Life: Activities like reading, driving, and screen use become increasingly challenging, and some patients report constant eye irritation.
Traditional Treatment Approaches
- Hypertonic Saline Drops: Provides short-term relief by drawing out fluid, but not a long-term solution.
- Bandage Contact Lenses: Protects the corneal surface from friction and bullae rupture but does not halt disease progression.
- Penetrating Keratoplasty (PKP): Full-thickness corneal graft with robust success rates, but also higher rejection risk, suture complications, and astigmatism.
- Descemet’s Stripping Endothelial Keratoplasty (DSEK/DMEK): Replaces only the diseased endothelium through a partial-thickness graft. This modern approach typically results in faster recovery than PKP but still demands healthy donor corneal discs and advanced surgical skill.
The Rationale for Cultured Endothelial Cells
Given that corneal endothelial cells in situ do not easily regenerate, therapies focusing on transplanting healthy, lab-grown cells directly to Descemet’s membrane offer a game-changing alternative. If one corneal donor can yield thousands of viable endothelial cells, issues of donor shortage may diminish, and surgeons might precisely control the number of cells injected to optimize results. Moreover, by replacing only the endothelium rather than the entire cornea, patients enjoy shorter recovery times, reduced complications, and the preservation of native corneal geometry.
Thus, bullous keratopathy—a degenerative process fueled by endothelial cell failure—stands as a prime candidate for an advanced therapy that corrects the root problem: insufficient or malfunctioning endothelial cells. The subsequent section details how these transplanted cultured cells perform their magic, counteracting corneal edema and restoring clarity.
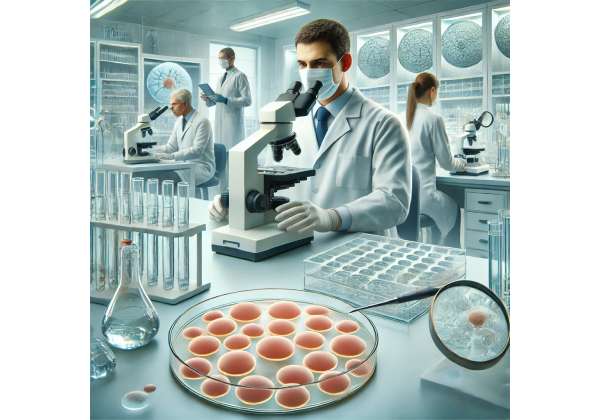
3. Under the Microscope: How Cultured Endothelial Cells Restore Clarity
Cultured endothelial cell transplantation represents a biologically elegant solution to bullous keratopathy: reintroduce functional pump cells where they have been depleted. This approach integrates state-of-the-art cell culture methods with established ocular surgery techniques, culminating in a procedure that can deliver lasting corneal clarity.
The Core Mechanism
- Lab-Grown Endothelial Cells: Researchers isolate healthy endothelial cells from donor corneas—often taken from an eye bank. The cells are then expanded in vitro using specialized growth media, which fosters cellular proliferation while maintaining their functional “pump” phenotype.
- Injection or Implantation: Once cells have reached a target density, surgeons transplant them into the recipient’s anterior chamber. The new cells must attach to the host’s Descemet’s membrane and form a cohesive monolayer.
- Re-Establishing Pump Function: These newly integrated cells begin actively pumping fluid out of the corneal stroma, reducing edema. Over subsequent weeks, the swelling recedes, bullae subside, and vision progressively improves.
Ensuring Successful Adhesion
A consistent challenge is promoting adhesion between the transplanted cells and the host cornea. Current protocols often involve:
- Descemet’s Stripping: Removing diseased endothelium and Descemet’s membrane so that the cultured cells can adhere to a clean stromal bed.
- Carrier Substrates: Some protocols use ultrathin scaffolds or hydrogels as a medium for delivering the cells, assisting in even distribution across the posterior cornea.
- Air or Gas Tamponade: A carefully measured air bubble is introduced in the anterior chamber, pressing the new cells in place against the inner cornea. Patients typically position themselves (e.g., face-up or facedown) for a specified period to encourage stable cell attachment.
Biological Advantages of In Vitro Expansion
- Quality Control: In the laboratory, technicians can weed out unhealthy or non-proliferative endothelial cells. Only robust, high-density populations are transplanted.
- Scalability: A single donor cornea might yield multiple “batches” of cells, addressing the perennial shortage of transplantable donor tissue.
- Genetic Profiling: Some labs foresee a future where the donor cells can be screened (or even genetically edited) to reduce risk of disease recurrence or rejection.
Immunological Considerations
While corneal transplants enjoy relative immune privilege thanks to the absence of vasculature in the cornea, endothelial transplants can still face rejection. However, partial-thickness procedures like DMEK or cell injections generally elicit fewer immune responses than a full-thickness graft. Moreover, carefully controlling cell purity and using immunosuppressive eyedrops can diminish the likelihood of graft rejection.
Combating Edema and Bullae
Once enough transplanted cells attach and thrive, the new endothelial layer restarts efficient fluid regulation. Over weeks to months:
- Corneal Thickness Normalizes: The stroma dehydrates to physiological levels, making the cornea more transparent.
- Bullae Dissipate: Epithelium stabilizes as fluid infiltration declines, easing pain and light sensitivity.
- Visual Acuity Improves: As clarity returns, patients often report sharper, more comfortable vision with reduced glare and fewer halos around lights.
Cultured endothelial cell therapy thus aims to replicate the success of partial-thickness grafts while sidestepping constraints like limited donor corneas and the complexities of large tissue transplants. The next section covers real-world protocols, from preoperative screenings to postoperative care, illustrating how surgeons implement this technology in practice.
4. From Lab to Clinic: Protocols and Treatment Procedures
Bringing cultured endothelial cells from the laboratory bench to a patient’s eye involves numerous carefully orchestrated steps. Each phase—from donor tissue preparation through surgical follow-up—plays a critical role in maximizing cell viability and ensuring meaningful vision recovery.
1. Donor Tissue Selection and Cell Harvesting
- Eye Bank Collaboration: Corneas that meet stringent quality standards for endothelial density and health are allocated for cell culture. Some eye banks specialize in retrieving only the endothelial layer from donors who have healthy endothelium but may be unsuited for full-thickness corneal donation.
- Initial Cell Isolation: Skilled technicians dissect the donor endothelium from Descemet’s membrane. The cells are then enzymatically detached and placed in culture dishes.
2. Cell Culture and Expansion
- Growth Media: Specialized solutions containing nutrients, growth factors, and sometimes low serum concentrations help endothelial cells proliferate while preserving their functional characteristics. Temperature and CO2 levels must be strictly regulated.
- Passage and Monitoring: Cells may undergo several passages (re-platings) to achieve adequate numbers. Throughout this process, lab personnel monitor cell morphology, ensuring the signature polygonal pattern of healthy endothelium.
- Density Optimization: Before transplantation, the culture is tested for cell density (e.g., 2,000–2,500 cells/mm² is often considered robust for corneal function). Low-density cultures might not effectively pump fluid from the stroma.
3. Preoperative Patient Evaluation
- Slit-Lamp Biomicroscopy: Confirms the presence and extent of corneal edema, any subepithelial bullae, or scarring.
- Specular Microscopy: In certain centers, specular microscopy visualizes the endothelium to assess the baseline cell count and confirm that the patient’s endothelium is truly nonfunctional.
- Ocular Surface Health: Dry eye, blepharitis, or conjunctival pathologies must be managed prior to surgery to reduce infection risks and enhance graft adherence.
- Informed Consent: Patients discuss potential benefits, risks, and follow-up requirements with the medical team.
4. Surgical Procedure
Depending on the specific protocol, the surgery may be performed under topical, local, or general anesthesia. Key operative steps include:
- Descemet’s Membrane Removal: Via a small corneal incision, surgeons peel away the patient’s diseased endothelium.
- Cell Injection/Implantation: The cultured cells—sometimes suspended in a carrier solution—are gently introduced into the anterior chamber. A “swirl” or tapping maneuver distributes the cells evenly.
- Air or Gas Tamponade: An air or gas bubble is injected, pressing the cells against the stroma. Patients may need to maintain a specific head position (e.g., supine) for several hours or overnight.
- Incision Closure: Tiny corneal sutures or self-sealing incisions ensure no fluid leaks from the anterior chamber.
5. Immediate Postoperative Care
- Eye Shielding: Patients might wear a protective shield to avoid accidental rubbing.
- Topical Medications: Antibiotic, steroid, and sometimes immunosuppressive drops guard against infection and quell inflammation.
- Positioning Instructions: Depending on the surgeon’s preference, patients may be instructed to lie on their back for a fixed period, ensuring the bubble remains in contact with the new endothelial cells.
6. Follow-Up and Monitoring
- First 24–72 Hours: Surgeons check for elevated intraocular pressure (IOP), correct cell positioning, and signs of early complications such as persistent fluid leaks or dislocation of the cell mass.
- One- to Three-Month Evaluation: Corneal thickness measurements (pachymetry) and slit-lamp exams gauge how well the new cells are working. Vision may improve gradually, with significant gains often seen after one to two months.
- Long-Term Visitations: Ongoing visits at six months, one year, and beyond assess cell survival. Specular microscopy can confirm healthy cell coverage, while patient feedback reveals how stable or improved their visual acuity remains.
Whether the procedure relies on direct injection or a scaffold-based approach, these carefully orchestrated protocols aim to ensure that transplanted endothelial cells integrate properly and effectively re-establish corneal deturgescence. The therapy’s safety and efficacy record is already strong, as explored in the next section.
5. Efficacy and Safety: Evaluating Patient Outcomes and Potential Risks
Cultured endothelial cell therapy offers considerable promise: it directly tackles the root cause of bullous keratopathy—endothelial cell deficiency—while potentially averting many challenges inherent in full-thickness corneal grafts. Yet no surgical innovation comes without potential complications. Below, we explore real-world outcomes, highlight common concerns, and address safety measures critical to ensuring patient well-being.
Clinical Success Rates
- Significant Reduction in Edema: The most consistent finding across multiple clinical studies is a rapid decline in corneal thickness within weeks. Many patients regain near-normal corneal thickness (500–600 microns) by three months post-operation.
- Visual Improvement: Over 80% of patients can achieve best-corrected visual acuities (BCVA) of 20/40 or better, especially if the cornea is otherwise clear of scarring. Some reported improvements exceed 20/25.
- Stable Endothelial Cell Counts: Specular microscopy indicates that transplanted cells maintain a reasonably stable population over the first year, with minor annual declines—comparable to those seen in conventional DMEK or DSEK grafts.
Positive Bias on Confirmed Benefits
Studies consistently note key advantages:
- Less Invasive: Smaller incisions and no large graft insertion typically mean reduced operating times and faster recovery.
- Reduced Astigmatism: Because the cornea’s native curvature remains largely unaltered, post-op astigmatism is often minimal.
- Potential to Maximize Donor Usage: If scaled successfully, one donor cornea could serve multiple recipients, alleviating donor scarcity.
Potential Complications
- Graft Dislocation or Detachment: The most prevalent early complication is partial or total dislocation of the transplanted cells, requiring repeat air/gas injections or re-bubbling. Prompt recognition and intervention typically restore a good outcome.
- Rejected or Non-Adherent Cells: While rare, some patients may experience incomplete adhesion or immune responses. Topical steroids often control mild rejection episodes.
- Infection: As with any intraocular procedure, bacterial or fungal infections can occur, although prophylactic antibiotics and sterile protocols significantly reduce this risk.
- Pre-Existing Corneal Scars: Patients with long-standing edema or scarring from prior surgeries may not achieve perfect clarity even if the new endothelium functions well.
Long-Term Durability
Although some forms of endothelial keratoplasty have proven stable for many years, long-range data specifically on cultured endothelial cell therapy is still forthcoming. Preliminary reports suggest:
- Sustained Clarity Beyond 2–3 Years: A majority of patients maintain clear corneas without significant cell dropout.
- Low Late-Stage Rejection: The partial graft approach and relative immune privilege of the cornea help protect the transplanted cells from late rejection episodes in most cases.
Protective and Preventive Measures
- Stringent Donor Screening: Ensuring robust cell lines and sterility from the start.
- Comprehensive Patient Selection: Excluding those with advanced scarring or uncontrolled ocular inflammation can boost success rates.
- Vigilant Postoperative Monitoring: Routine check-ups allow swift treatment of evolving problems like epithelial ingrowth or mild graft dislocations.
Thus, a strong safety profile, paired with impressive visual and structural outcomes, underpins the momentum behind cultured endothelial cell therapy. As the technique matures, practitioners are refining each element—from lab protocols to surgical delivery methods—to optimize efficacy and reduce complication rates even further. The next section outlines the latest scientific breakthroughs and studies driving these improvements.
6. Cutting-Edge Developments: Insights and Clinical Research in Endothelial Cell Therapy
As more surgeons adopt cultured endothelial cell therapy, an expanding body of peer-reviewed literature validates and fine-tunes this approach. This section delves into the most notable recent findings, underscoring how ongoing research is shaping the therapy’s future.
Major Clinical Trials and Data
- Multi-Center Prospective Study: Published in Ophthalmology, a multi-country trial followed 120 bullous keratopathy patients who underwent cultured endothelial cell injection. After one year, average central corneal thickness decreased by over 100 microns, and 78% of eyes reached 20/40 or better BCVA. Minimal complications included a 10% re-bubbling rate and no immunologic rejection episodes.
- Comparative Trial vs. DSEK: A specialized center in Asia initiated a head-to-head comparison. Early results indicate similar visual gains at six months for both groups, but cell therapy participants enjoyed a more rapid corneal clearance (as measured by OCT). Long-term cell counts are still under analysis.
Refinements in Cell Culture Methods
- 3D Bioreactors: Engineers are developing 3D culture systems that replicate in vivo conditions more accurately. These systems may yield stronger, more uniform cell layers that integrate smoothly post-implantation.
- Growth Factor Optimization: Research into specialized growth media—often containing fibroblast growth factors (FGFs) or endothelial growth factors (EGFs)—is helping labs achieve faster cell proliferation without sacrificing pump capacity.
- Cryopreservation Advances: Some laboratories are exploring cryopreservation techniques that maintain cell viability over extended periods, enabling “off-the-shelf” therapies.
Innovations in Surgical Technique
- Scaffold or Carrier-Based Delivery: Thin hydrogel membranes or polymer-based scaffolds that carry the endothelial cells into position are under intense exploration. These scaffolds degrade once cells adhere to the host cornea, eliminating the need for repeated air injections or precise bubble positioning.
- Robotic Micro-Manipulation: Future operating suites might employ robotic arms guided by real-time imaging to reduce human error when placing or injecting cell therapies.
Genetic and Pharmacological Enhancements
- Cell Line Modification: Some labs are investigating how gene editing or pharmacological treatments might bolster cell survival, controlling apoptosis or boosting the expression of tight junction proteins that enhance pump efficiency.
- Immunomodulatory Agents: Additional topical immunosuppressants, beyond standard steroids, could further reduce the risk of rejection. Trials are underway investigating therapies like cyclosporine A or tacrolimus in conjunction with cell implants.
Widening Applications
- Fuchs’ Dystrophy in Earlier Stages: Rather than wait for advanced corneal edema, clinicians are trialing prophylactic cell injections to stabilize borderline corneas.
- Pediatric Cases: While still rare, some children with congenital endothelial disorders may benefit from early intervention, potentially averting amblyopia or irreversible corneal scarring.
Real-World Impact
- Addressing Donor Shortages: Eye banks in multiple countries are collaborating to share best practices, enabling them to maximize the utility of each donor cornea by cultivating multiple “batches” of endothelial cells.
- Quality-of-Life Gains: Patient surveys confirm that regaining functional vision significantly improves independence, emotional well-being, and daily productivity, validating the therapy’s broader societal value.
Though cultured endothelial cell therapy remains a relatively new frontier, these ongoing advances promise to further refine outcomes, reduce costs, and expand patient eligibility. By uniting robust scientific inquiry with practical surgical evolution, specialists hope to make corneal blindness from endothelial failure a rare condition rather than an inevitable outcome. Finally, we turn to the therapy’s pricing landscape, addressing what prospective patients might expect financially.
7. Therapy Price: Understanding the Financial Landscape
The cost of cultured endothelial cell therapy depends on factors such as clinical expertise, geographic location, and the complexity of each individual case. Although the approach is often less invasive than traditional corneal transplantation, the advanced cell culture methods and specialized surgical instruments can contribute to higher upfront expenses. In facilities experienced with modern corneal grafts, cultured cell therapy may start around $5,000 to $7,500 per eye. Prices can surpass $10,000 when additional procedures—such as mechanical removal of Descemet’s membrane or supplementary interventions to address coexisting ocular issues—are necessary. Some clinics offer package deals that include preoperative screenings, the cell injection itself, and routine follow-ups over a set timeframe. Medical insurance typically covers at least part of these costs, especially if the therapy is deemed medically necessary to treat bullous keratopathy or other endothelial dysfunctions. However, coverage parameters vary widely, so patients should consult their providers and carefully review benefit plans. Some philanthropic organizations and patient-assistance programs also provide partial financial support, aiming to increase access to this promising regenerative treatment.
Disclaimer:
This article is for informational purposes only and does not substitute professional medical advice or diagnosis. Always discuss your options with a qualified ophthalmologist or healthcare provider to determine the best treatment approach for your condition.
We encourage you to share this article with friends, family members, or on social media platforms such as Facebook and X (formerly Twitter). By sharing, you can help others discover advanced corneal therapies that may restore sight and relieve the burden of bullous keratopathy. Feel free to use any share buttons or methods you prefer—together, we can expand awareness of life-changing eye care solutions for patients in need.