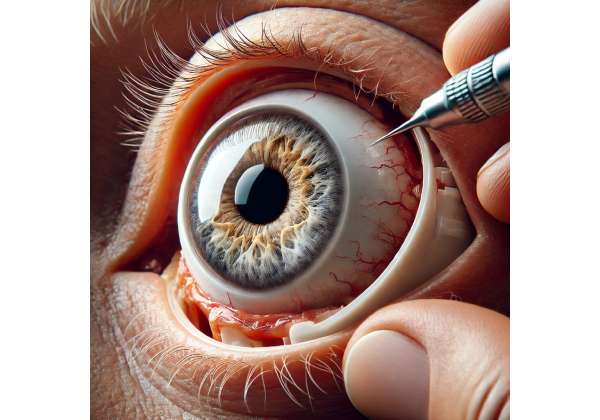
Ocular trauma can lead to devastating consequences for a person’s sight and self-confidence. In cases where the globe (eye) is severely damaged or needs removal, ocular prosthetics offer a path toward regaining a more normal appearance and enhancing quality of life. While stock (mass-produced) prostheses have provided relief for decades, modern approaches emphasize customized ocular prosthetics—highly individualized artificial eyes that match the wearer’s natural anatomy and coloration. Below is a comprehensive exploration of how these tailored devices are revolutionizing outcomes for those recovering from significant eye injuries.
1. A Personalized Approach: Why Customized Ocular Prosthetics Excel
Customized ocular prostheses are individually crafted artificial eyes, created to match the remaining natural eye in terms of color, shape, and alignment. Beyond aesthetics, they are designed to minimize discomfort and maximize safety, making them especially beneficial for people whose vision was compromised by trauma.
Shifting from “One-Size-Fits-All” to Tailored Solutions
Historically, patients who lost an eye or underwent enucleation (surgical removal of the eye) were fitted with generic, prefabricated prostheses. Although these solutions offered an immediate option, they often fell short in mimicking the precise hue, iris design, and scleral details of the healthy eye. As technology and ophthalmic artistry advanced, specialists realized the profound psychological and physical gains achievable through a patient-specific approach.
- Natural Aesthetic: By meticulously matching the colors, flecks, and patterns of the patient’s remaining eye, these prostheses are virtually indistinguishable from a real eye at normal viewing distances.
- Optimal Comfort: A custom-fit ocular prosthetic accounts for the unique contour of the orbital socket and any surgical modifications. This tailoring reduces friction and irritation, improving long-term wear.
- Enhanced Mobility: When crafted to align with the patient’s extraocular muscles or implant types, a personalized prosthesis can move more harmoniously, further boosting the cosmetic illusion of a “living” eye.
Ideal Candidates
Those who may benefit the most from custom ocular prostheses include:
- Trauma Survivors: Whether due to blunt force injuries, penetrating wounds, or chemical burns.
- Cancer Patients: Individuals who have undergone enucleation or exenteration to treat ocular or orbital tumors.
- Congenital Anomalies: Some children are born with microphthalmia (abnormally small eyes) and can benefit from specialized prosthetic expansions over time.
- Infection-Related Surgeries: Rare but severe eye infections sometimes necessitate surgical removal, leaving an empty socket that a prosthesis can fill.
Multidisciplinary Collaboration
Custom ocular prosthetics are often the result of a collaborative approach between:
- Ocularists: Skilled technicians or artists with expertise in fabricating prosthetic eyes.
- Ophthalmologists or Oculoplastic Surgeons: Medical doctors who assess the socket’s health, perform surgery, and ensure the prosthesis is medically sound.
- Patients and Families: Personal input on color matching, comfort levels, and aesthetic preferences is critical for an optimal result.
In sum, a customized ocular prosthetic stands out for its highly personalized design, remarkable natural look, and improved comfort, distinguishing it from off-the-shelf alternatives. The next section explains the traumatic eye injuries that precipitate such a need, casting light on why these specialized prosthetics play an indispensable role.
2. The Reality of Ocular Trauma: Causes, Consequences, and the Path to Prosthesis
Ocular injuries can occur in an instant—whether from accidents, sports mishaps, violence, or workplace hazards. When trauma leaves the eye irreversibly damaged, emotional and physical repercussions can be profound. Comprehending the nature of these injuries offers insight into why prosthetic intervention becomes essential.
What Constitutes Ocular Trauma?
The term “ocular trauma” encompasses a wide range of incidents:
- Penetrating Injuries: Sharp objects or debris can breach the eye’s protective outer layers, potentially lacerating critical internal structures like the iris, lens, or retina.
- Blunt Force Impacts: Falls, punches, car accidents, or sports impacts can cause ruptures or severe internal bleeding in the eye, sometimes leading to irreversible damage.
- Chemical Burns: Workplace or household chemicals may induce corneal scarring, lens opacities, or severe tissue necrosis, making the eye nonfunctional.
- Thermal or Radiation Burns: High-heat exposures (e.g., explosions) or radiation accidents can destroy ocular tissue.
- Secondary Infections: A seemingly minor eye injury can spiral into severe infection (e.g., endophthalmitis), culminating in vision loss or necessitating enucleation.
Short- and Long-Term Impact on Vision
- Immediate Loss of Vision: Complete vision impairment occurs if trauma destroys optical structures or severs the optic nerve.
- Chronic Pain and Inflammation: Some patients endure persistent eye pain if inflammatory responses remain unresolved.
- Infection Risks: Open injuries are susceptible to bacterial or fungal invasion, endangering the entire globe.
- Psychological Burden: Depression, anxiety, and diminished self-esteem often follow traumatic eye loss or disfigurement.
Surgical Decision: When Removal is Inevitable
While modern ophthalmology strives to salvage the natural eye whenever possible—using reconstructive surgeries, corneal grafts, vitrectomies, or lens implants—some injuries are too severe. If repeated attempts at restoration fail, or if the damage is life-threatening (e.g., ocular cancers, uncontrollable infections), surgeons may choose enucleation (removal of the eyeball) or evisceration (removal of internal eye contents while retaining the scleral shell).
Post-Enucleation Complexities
Patients who undergo eye removal face:
- Orbital Volume Deficit: The empty socket can collapse inward without a suitable implant, causing facial asymmetry.
- Scar Tissue Formation: Surgical sites may form fibrotic tissue that complicates prosthetic fitting.
- Socket Infections or Granuloma Formation: Even after healing, the orbital environment needs ongoing monitoring to prevent complications that interfere with prosthetic wear.
Given these realities, a well-crafted, custom ocular prosthetic significantly aids in restoring facial symmetry, improving self-confidence, and enhancing quality of life. But how exactly do these prostheses function? The following section offers a closer look at their mechanical and biological synergy.
3. How Customized Prosthetic Eyes Work: Beyond Aesthetics and Toward Enhanced Function
At first glance, an ocular prosthesis appears to be purely cosmetic—replacing the visible portion of the lost eye. However, customized prosthetic eyes can also deliver functional advantages, such as improved tear distribution and better socket stability, essential for patients recovering from trauma.
Fundamental Components of a Customized Prosthesis
- Acrylic or Medical-Grade Polymers: Modern artificial eyes are typically fashioned from high-quality polymethyl methacrylate (PMMA) or similar materials. PMMA is biocompatible, nonporous, and can be polished to resemble the luster of a natural sclera.
- Intricate Iris Design: Skilled ocularists painstakingly hand-paint or digitally replicate the iris color, fiber patterns, and subtle flecks to mirror the patient’s real eye. This artistry ensures a lifelike appearance.
- Clear Protective Coat: A final resin or varnish layer seals the painted iris, preventing color fade and safeguarding against daily wear.
Mechanisms of Enhanced Comfort and Socket Health
- Smooth Surface Finish: A well-finished outer surface glides easily against the eyelids and conjunctiva, minimizing friction.
- Proper Weight Distribution: A prosthesis that accurately matches the orbital socket’s dimensions helps maintain natural eyelid function and tear flow.
- Supporting Orbital Implants: When surgeons place an orbital implant post-enucleation—often made of porous materials like hydroxyapatite—it can be integrated with the prosthesis to enhance movement and alignment, elevating cosmetic outcomes further.
Rebuilding Symmetry and Movement
- Eyelid Support: Properly contoured prostheses push outward against the eyelid. This outward pressure helps maintain normal eyelid position, combating droopiness or asymmetry that might arise post-surgery.
- Synchronized Gaze: Although an artificial eye cannot see, it may move in tandem with the healthy eye—thanks to coupling with existing muscles or an orbital implant pegging system. This subtle motion significantly boosts the prosthesis’ believability in day-to-day interactions.
- Realistic Luster: The reflective properties of medical-grade acrylic closely mimic the cornea’s shine, offering a sense of “moisture” that can trick the observer’s eye.
Long-Term Biocompatibility
A prime reason for using acrylic or silicone-based materials is their low allergenic profile. Additionally, modern prostheses are shaped to create minimal pockets where bacteria could proliferate. This design fosters a healthier ocular surface environment, often lowering infection and irritation risks.
Addressing Secondary Facial Trauma
Many trauma patients have damage extending beyond the eye, such as facial fractures or scarring around the orbit. Custom prostheses can be tweaked to accommodate these variations, ensuring a more uniform facial appearance and better integration with reconstructive surgeries (e.g., orbital floor repair).
In essence, the modern custom ocular prosthesis is more than a static “glass eye.” Instead, it leverages sophisticated materials, anatomical customization, and synergy with surgical implants to provide both psychological and biomechanical advantages. The subsequent section tackles how these prostheses are typically prescribed, molded, and fitted in practice.
4. From Evaluation to Final Fit: Protocols for Customized Ocular Prosthetic Placement
A quality ocular prosthetic journey spans multiple stages—initial exams, socket preparation, impression-taking, detailed artistry, and final checks. Though the process requires patience, the result is a lifelike, well-fitting artificial eye that can last for years with proper upkeep.
1. Comprehensive Evaluation
- Initial Consult: An oculoplastic surgeon or ocularist assesses the orbital socket’s condition, looking for signs of infection, excessive scar tissue, or insufficient volume. Baseline measurements of eyelid position, socket depth, and any existing implants are recorded.
- Medical History: Understanding the specifics of the patient’s trauma, prior surgeries, or underlying diseases informs decisions about timing and prosthesis type.
2. Preparation of the Socket
- Healing Period: Typically, surgeons recommend waiting several weeks (to months) after enucleation or reconstructive surgery before fitting a permanent prosthesis. This allows inflammation to subside and tissues to stabilize.
- Use of Conformer Shells: Post-surgery, patients may wear a clear conformer shell to maintain the socket shape. This shell prevents the socket from contracting or collapsing during healing.
3. Impression Process
- Custom Mold Creation: The ocularist often injects a safe impression material into the socket to capture minute surface details.
- Trial Fitting: A preliminary plastic or wax shell is constructed using the mold. This “trial eye” is placed in the socket to test comfort, ensure correct eyelid closure, and approximate movement.
4. Hand Painting and Fabrication
- Iris Craftsmanship: Ocularists examine the patient’s healthy eye under various lighting conditions to replicate nuances of color, pupil size, and iris depth. They often paint by hand, layering pigments to build a realistic color gradient.
- Scleral Tinting: The sclera (the white part) might incorporate subtle veins or shading to emulate the contralateral eye precisely.
- Final Polishing: Once the paint is sealed, the entire prosthesis undergoes shaping and high-polish finishing. This yields a mirror-smooth surface that is easy to clean and gentle on the eyelids.
5. Fitting and Adjustments
- Insertion and Assessment: The patient tries on the finished prosthesis. The ocularist checks its position, eyelid closure, comfort, and alignment. Minor adjustments to thickness or curvature can further refine the fit.
- Movement Testing: If the patient has an integrated orbital implant or healthy extraocular muscles, the ocularist evaluates how well the new eye moves alongside the existing one.
6. Education and Maintenance
- Wear Instructions: Most patients wear the prosthesis continuously, removing it only for periodic cleaning. Ocular lubricants or artificial tears may be recommended to enhance comfort.
- Cleaning Regimen: Typically, a gentle daily rinse in sterile saline or mild soap solution suffices. Some prefer specialized soaking solutions to reduce protein buildup and maintain clarity.
- Follow-Up Appointments: Over time, changes in the socket or natural eye can necessitate re-polishing or adjustments. Many ocularists advise annual check-ups to keep the prosthesis in prime condition.
By adhering to a meticulous sequence of steps—socket preparation, impression-making, artistic design, and thorough follow-up—patients can enjoy a prosthesis that looks and feels like a natural eye. Our next section addresses the real-world outcomes that underscore how effectively custom ocular prosthetics restore confidence and day-to-day functioning.
5. Gauging Success: Effectiveness and Safety of Modern Artificial Eyes
Decades of refinement in ocular prosthetic design underscore their reliability, comfort, and potential to restore a degree of normalcy for individuals coping with ocular trauma. Nonetheless, understanding potential risks and realistic expectations helps patients approach the process with clarity.
Positive Outcomes Documented
- High User Satisfaction: Numerous surveys among prosthetic eye users indicate satisfaction rates exceeding 80%, largely attributed to improved self-image and social interactions.
- Stable Fit Over Time: Properly crafted prostheses may retain their shape and clarity for several years—sometimes five or more—before significant changes or replacements are required.
- Lifestyle Improvements: Many patients resume public-facing roles, sports (with caution), or active social lives thanks to renewed self-confidence.
Key Benefits
- Psychological Uplift: By removing the visible signs of an eye loss, prostheses help many patients mitigate trauma-related anxiety or depression.
- Functional Eyelid Support: Some individuals report that blinking feels more natural, and dryness is reduced because the prosthesis helps evenly distribute tears.
- Protective Buffer: Artificial eyes may guard delicate orbital tissues, preventing foreign particles from irritating or injuring the socket.
Addressing Safety Concerns
- Risk of Socket Irritation: If the prosthesis is ill-fitting or if daily hygiene is neglected, irritations, discharge, or mild infections can ensue. Regular cleaning and periodic checkups minimize these issues.
- Allergic Reactions: Rarely, patients show sensitivity to the prosthetic’s materials or cleaning solutions. Switching to alternative, hypoallergenic formulas typically resolves the issue.
- Movement Limitations: The prosthesis relies on muscle or implant coupling for motion. If an orbital implant is not present or muscle function is compromised, eye movement range may be somewhat limited.
- Future Adjustments: Children, in particular, require frequent adjustments or expansions as they grow, ensuring symmetry with the developing facial structures.
Combining Prosthetics with Other Therapies
In certain cases, patients might explore:
- Eyelid Surgery: Blepharoplasty or eyelid reconstruction to optimize the eyelid contour and cosmetic result.
- Socket Augmentation: Orbital implants, dermal grafts, or fat transfers to correct volume deficits.
- Psychological Support: Counseling or support groups that help individuals process the emotional toll of trauma and adapt to prosthesis wear.
Given these multifaceted considerations, it’s clear that ocular prostheses, especially when customized, remain a safe and effective choice for addressing both cosmetic and functional concerns post-trauma. As clinical research evolves, new materials, manufacturing techniques, and digital design processes are further enhancing outcomes, as elaborated in the next section.
6. Latest Research and Innovations: Advancing Ocular Prosthetic Science
Science and art seamlessly intertwine in the realm of ocular prosthetics. While the classical approach of hand-painting remains invaluable, contemporary researchers and technicians are pioneering new methods to boost precision, comfort, and longevity. Recent studies underscore these breakthroughs, highlighting how they can refine the lives of trauma survivors.
1. Digital Imaging and 3D Printing
- High-Resolution Eye Scans: Ophthalmologists increasingly use scanning technology (like OCT or specialized camera systems) to capture the healthy eye’s shape and color. This data guides the creation of a digitally rendered iris or sclera, ensuring near-flawless color matching.
- 3D-Printed Shells: Some labs are experimenting with printing the prosthetic shell from biocompatible polymers, reducing reliance on manual carving. Early-phase studies suggest that 3D-printed shells can achieve an even closer anatomical fit, minimizing alignment issues.
2. Lifelike Movement Enhancements
- Advanced Orbital Implants: Porous implants (e.g., Medpor or hydroxyapatite) allow fibrovascular ingrowth, which better anchors the prosthesis to the socket’s muscles. Studies report improved ocular motility and patient satisfaction with these integrated solutions.
- Magnetic Coupling: A few experimental designs utilize small magnets embedded in the orbital implant and the prosthesis, facilitating more synchronized movement. While still niche, case reports indicate potential for realistic motion and stable retention.
3. Bacterial-Resistant Materials
Research has emerged focusing on antimicrobial coatings or impregnating the prosthetic surface with silver nanoparticles. Preliminary findings in Contact Lens & Anterior Eye suggest such modifications could reduce biofilm formation, leading to fewer complications like socket discharge or mild conjunctivitis.
4. Customized Prosthetics for Pediatric Applications
Children who lose an eye to trauma or congenital anomalies pose unique challenges because their sockets and orbits are still growing:
- Expandable Prostheses: Studies show some success with adjustable or “expandable” prosthetic shells that can be incrementally enlarged, minimizing repeated surgeries.
- Longitudinal Research: Ongoing trials track how well these devices preserve facial symmetry into adolescence, aiming to reduce the psychological burden on pediatric patients.
5. Psychosocial Impact Analyses
Recent qualitative research underscores that beyond the cosmetic dimension, custom ocular prosthetics significantly influence social reintegration. In interviews, patients consistently report greater self-esteem, less self-consciousness in public, and an enhanced sense of identity. Investigations also find that robust psychosocial support—like counseling or peer support groups—further amplifies these gains.
6. Artificial Intelligence (AI) in Color Matching
A small but growing body of work explores AI algorithms that can identify subtle color variations in an individual’s iris and sclera, generating custom “paint recipes” for ocularists to replicate. Early pilot data from a tech-ophthalmology consortium found that these color-precision techniques can cut down manual painting time while increasing color-matching accuracy.
Such innovations signal an exciting future for custom ocular prosthetics, one where cutting-edge science meets the artisanal craft to produce the most realistic and comfortable artificial eyes possible. Still, many prospective patients weigh their financial options carefully—a subject we tackle in our next and final section.
7. Therapy Price: Cost Factors and Financial Considerations
For those interested in customized ocular prosthetics, navigating the financial aspect is a critical part of the decision-making process. Costs can vary widely based on geographic region, ocularist expertise, and the complexity of the patient’s condition. In many cases, a high-quality prosthetic eye ranges from $2,500 to $5,000, though fees may be higher for advanced techniques like magnetic coupling or specialized orbital implants. Some ocularists bundle additional services—such as color revisions, minor adjustments, or annual polishing visits—into the initial price. Insurance coverage often depends on whether the prosthesis is deemed medically necessary, which frequently applies to individuals who have undergone enucleation or suffered severe ocular trauma. Certain private insurers and national health programs partially or fully reimburse these expenses, while others might require a copay. Patients can also explore financing plans, charitable foundations, or specialized grants that help mitigate out-of-pocket costs. Ultimately, comparing quotes from multiple ocularists, consulting with the primary eye surgeon, and clarifying insurance details can guide a more informed, budget-friendly choice.
Disclaimer:
This article is intended for informational purposes only and does not replace professional medical advice or consultation. Always seek personalized guidance from a qualified eye care specialist or ocularist regarding your unique circumstances.
We invite you to share this article with friends, colleagues, or on social media platforms such as Facebook and X (formerly Twitter). By spreading knowledge about customized ocular prosthetics, you can help empower individuals who are recovering from ocular trauma to find renewed confidence and a more natural appearance. Feel free to use any share buttons or methods you prefer—together, we can raise awareness and support positive outcomes for those in need of advanced eye care solutions.